Translate this page into:
High Prevalence of Asymptomatic Anterior Tarsal Tunnel Syndrome in Toddy Tappers of South India: A Case Series of 21 Participants
Ajay Panwar, MD, DM Department of Neurology, Guardian Multispeciality Hospital Warangal 506007 Telangana India ajay19panwar@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Anterior tarsal tunnel syndrome (ATTS) is an uncommon entrapment neuropathy which occurs due to the compression of deep peroneal nerve under the inferior extensor retinaculum at the ankle. We observed a frequent occurrence of this syndrome in toddy palm tappers and hence, planned to study the association between the two.
Materials and Methods We studied the prevalence of isolated deep peroneal neuropathy at the ankle among the asymptomatic toddy tappers enrolled over a period of 3 months.
Results In our case series, 81% (17/21) of the study participants had ATTS of which 43% (9/21) had unilateral and 38% (8/21) had bilateral involvement. There was a strong inverse association (p < 0.001) of “duration of toddy tapping in years” with peroneal (extensor digitorum brevis) amplitudes on both the sides.
Conclusion Our study confirms “palm tree climbing” to be an occupational etiology of ATTS.
Keywords
anterior tarsal tunnel syndrome
deep peroneal mononeuropathy
palm tree
toddy tapping
Introduction
Borassus flabellifer, commonly known as toddy palm, is native to the Indian subcontinent. Kallu, a beverage made from the sap of the toddy tree, is a popular drink in rural parts of Telangana. The extraction and collection of sap from the tree are called tapping. Many people work as toddy tappers in this region.
Among the patients seen in our routine neurology clinics, we observed a frequent occurrence of anterior tarsal tunnel syndrome (ATTS) in toddy tappers; so, toddy tree climbing appeared to be an occupational risk factor for ATTS.
ATTS is an entrapment neuropathy which occurs due to the compression of deep peroneal nerve (DPN) under the inferior extensor retinaculum at the ankle.1 The DPN is a major branch of common peroneal nerve which travels in the anterior compartment of the leg. It is mainly a motor nerve and supplies tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius muscles in the leg.2 At the ankle, DPN passes beneath the extensor retinaculum and enters the anterior tarsal tunnel which is a flat space bounded laterally by the malleoli, inferiorly by the talus and navicular, and superiorly by inferior extensor retinaculum.3 In the tarsal tunnel, DPN divides into two terminal branches, the lateral branch gives a motor supply to the extensor digitorum brevis (EDB) muscle, while the medial cutaneous branch provides sensation to the web space between the first and second toes4 (Fig. 1). Thus, ATTS may present with foot pain, paresthesias, and decreased sensation in the first web space, atrophy, and weakness of EDB. The known causes of DPN compression in the anterior tarsal tunnel are trauma, bony abnormalities of the ankle, pes cavus, ganglion cysts, and wearing tight-fitting or high-heeled shoes.5 6

-
Fig. 1 A sketch drawing showing the anatomy of the anterior tarsal tunnel.
Fig. 1 A sketch drawing showing the anatomy of the anterior tarsal tunnel.
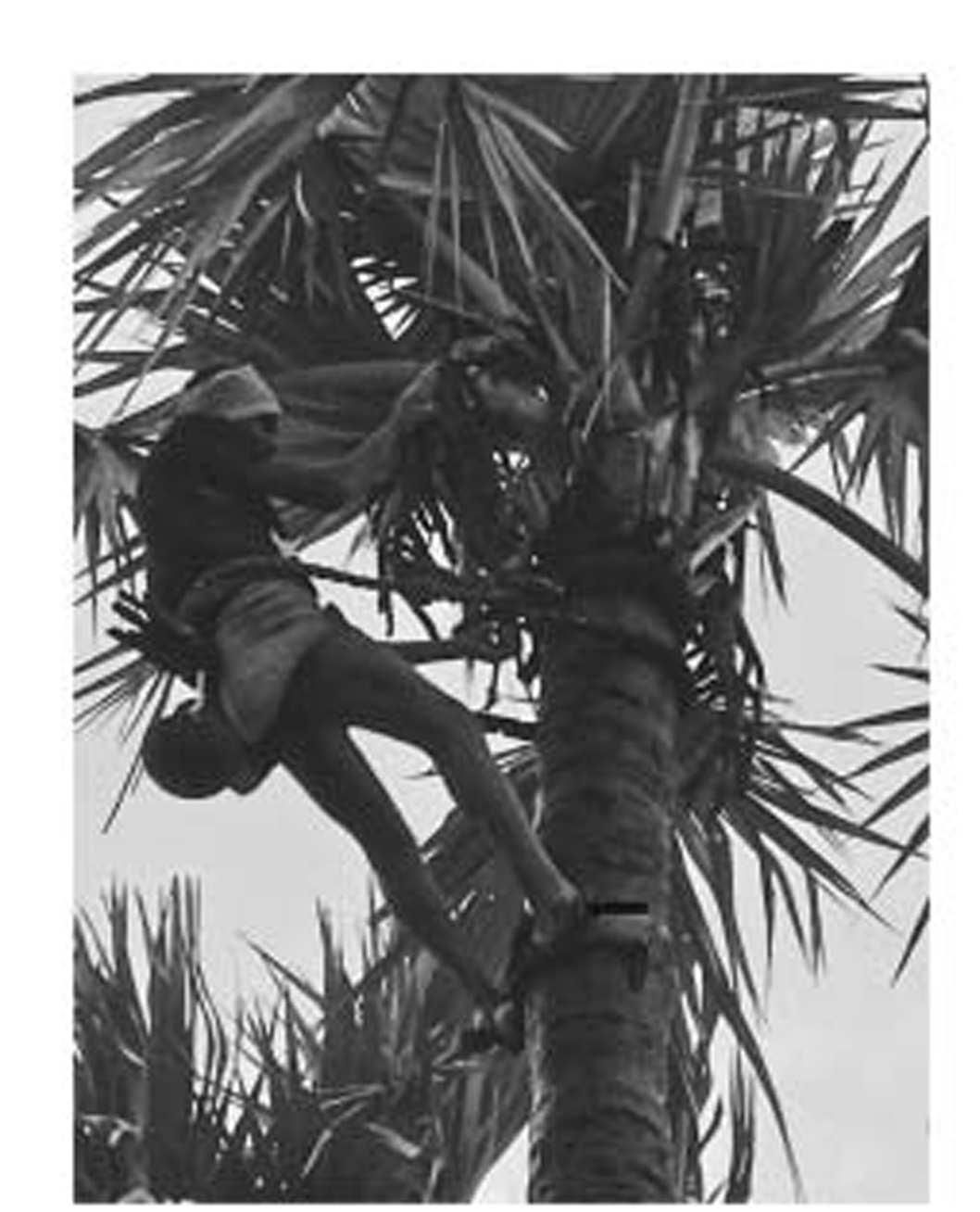
Toddy tappers wrap gujji (a ring-like equipment made of tire rubber and ropes) around their ankles, which helps them to maintain a firm grip on the tree trunk while climbing up for tapping (Fig. 2). Hence, chronic prolonged use of gujji may cause DPN compression at the ankle, resulting in ATTS. The occupational association of ATTS is well known in dancers wearing tight shoes.5 Palm tree tapping too appears to be characteristically associated with ATTS; however, it does not find a mention in the medical literature. Consequently, we planned to estimate the prevalence of ATTS in toddy climbers and, therefore, to observe its causal association with this occupation.
-
Fig. 2 A toddy tapper climbing up the palm tree with gujji (black arrow) wrapped around his ankles.
Fig. 2 A toddy tapper climbing up the palm tree with gujji (black arrow) wrapped around his ankles.
Materials and Methods
A cross-sectional evaluation of 21 toddy tappers was conducted in the Neurology Department of Kakatiya Medical College and associated Mahatma Gandhi Memorial Hospital at Warangal. The Institutional Ethics Committee approved the study protocol, and informed consent was obtained from the participants enrolled in the study. The study participants were consecutively enrolled over a period of 3 months from June 2018 to August 2018. The recruitment was done from the healthy adult (age ≥18 years) male persons accompanying the outpatients whose occupation was toddy tapping. We conducted the study among healthy toddy tappers instead of those with neurological symptoms, so as to test the direct association of toddy tapping with ATTS, while avoiding any potential confounding factors. A brief questionnaire with leading questions concerning medical history and screening of neurological symptoms was used to select healthy toddy tappers. The initial enrollment was done in medicine and neurology outpatient departments; however, all the enrolled patients underwent screening in the neurology department.
Exclusion Criteria
The participants with neurological symptoms and any systemic or neuromuscular disease were excluded. Those with a history of neurotoxic drug intake, prolonged exposure to neurotoxins, or alcoholism were excluded. The presence of pes cavus, soft-tissue swelling, and bony abnormalities of the ankle also met the exclusion criteria. The participants with a history of ankle trauma were also excluded. The enrolled participants underwent routine blood chemistry, including blood sugar, and those observed to have abnormal results were excluded.
The participants included underwent nerve conduction studies (NCSs) of both the lower limbs according to our institution's routine NCS protocol. Motor studies were conducted for peroneal and tibial nerves and sensory studies for sural nerve. Peroneal nerve studies were performed for EDB and tibialis anterior muscles and tibial studies for abductor hallucis brevis (AHB). Isolated peroneal (EDB) neuropathy with an increased distal latency of compound muscle action potential (CMAP) and/or reduced amplitudes along with normal tibialis anterior CMAPs was considered as the electrophysiological correlate of ATTS.
All patients were examined for physical signs of ATTS, namely, EDB atrophy, decreased sensation in web space between the great and second toes, and Tinel's sign by percussion over the anterior ankle.
Nerve Conduction Studies
NCSs were performed using Neuroperfect plus EMG-2000 (Medicaid systems, Chandigarh, India). The room temperature was maintained at 25 to 30°C. Filters were used at 2 Hz and 10 kHz for motor studies and 20 Hz and 2 kHz for sensory studies. The sweep speed for motor and sensory studies was set at 5 milliseconds/division and 2 milliseconds/division, respectively. The sensitivity settings of 20μV per division and 200 μV per division were used for sensory and motor studies, respectively. Motor and sensory amplitudes were measured from baseline to negative peak. Supramaximal stimulations were used to obtain amplitudes. All the motor studies were performed with participants lying comfortably in a supine position. Standardized techniques as detailed by Preston and Shapiro were used to perform the studies.7
Peroneal Motor (Extensor Digitorum Brevis) Study
The active electrode (G1) was placed on the dorsolateral foot over the muscle belly, and the reference electrode (G2) was placed over the metatarsophalangeal joint of the little toe. The ground electrode in all the studies was placed between the stimulator and recording electrodes. Distal stimulation was given at the ankle anteriorly, slightly lateral to tibialis anterior tendon. Two proximal stimulations were performed, the first on the lateral calf, one to two fingerbreadths below the fibular head, and the second in the lateral popliteal fossa, at a distance of 10 to 12 cm from the below-fibular head site.
Peroneal Motor (Tibialis Anterior) Study
G1 electrode was placed on the muscle belly of the tibialis anterior, at nearly one-third of the distance from tibial tubercle to lateral malleolus.8 G2 electrode was placed distally over the anterior ankle on the bony surface of the tibia. Distal stimulation was performed on the lateral calf, one to two fingerbreadths below the fibular head. Proximal stimulation was performed at the lateral knee, just medial to the tendons of external hamstring, at a distance of 10 to 12 cm from the distal stimulation site.
Tibial Motor Study
G1 electrode was placed over the AHB muscle, 1 cm below and behind the navicular prominence. G2 placed over the first metatarsophalangeal joint. The distal stimulation was performed just above and behind the medial malleolus, and the proximal stimulation was given in the midposterior knee over the popliteal artery.
The cut-off values used for normal distal latency, amplitude, and conduction velocity were ≤6.5 milliseconds, ≥2 mV, and ≥44 m/s for peroneal (EDB), respectively; ≤6.7 milliseconds, ≥3 mV, and ≥44 m/s for peroneal (tibialis anterior), respectively; and ≤5.8 milliseconds, ≥4 mV, and ≥41 m/s for tibial (AHB), respectively.7 These cut-off values allowed for a stricter threshold in determining abnormalities as compared with normative data (mean with three standard deviation [SD] values) from Indian patients, thus to ensure a high specificity in diagnosing ATTS.9
Sural Sensory Study
Antidromic sural studies were performed with patients lying on their sides and the recording leg facing up. G1 was placed behind the lateral malleolus, and G2 was placed 3 to 4 cm distal to G1. Stimulation was given over the posterolateral calf. Maximal response was attempted by slight repositioning of the recording electrodes from the original position. Side-to-side comparisons for latency and amplitude were performed.
The cut-off values used for normal sural studies were distal latency ≤4.4 ms, amplitude ≥6 μV, and conduction velocity ≥40 m/s.7
Statistical Analysis
The data entry was done in Microsoft Excel 2016 and analyses were done on software statistical package SPSS version 16.0 (IBM, Inc., Chicago, Illinois, United States). Categorical variables were expressed as percentages and continuous variables as means ±SD.
Results
We observed 21 toddy tappers with a mean age of 46.3 (±10.4) years. Mean duration of toddy tapping was 24.7 (±9.25) years. NCS values were within the normal range for peroneal (tibialis anterior), tibial, and sural nerves. For these three, a paired t-test showed no significant difference and Pearson's correlation showed a strong correlation in NCS values among the two sides. We have arbitrarily shown the right-side data analysis for peroneal (tibialis anterior), tibial, and sural nerves in Table 1. Besides, we observed a high prevalence of isolated peroneal (EDB) neuropathy. It was observed in 81% (17/21) of the participants of which 43% (9/21) had unilateral and 38% (8/21) had bilateral involvement. Mean peroneal (EDB) amplitudes for the left and right sides were significantly different and below the normal range, being 01.64 (±1.56) mV and 0.85 (±1.12) mV, respectively (Table 1). Mean peroneal (EDB) distal latencies were bilaterally increased (left, 6.65 ±0.51 milliseconds and right, 6.72 ±1.53 milliseconds); however, the difference among the sides was not statistically significant.
|
Variables |
Values |
|---|---|
|
Abbreviations: ATTS, anterior tarsal tunnel syndrome; DAMP, distal amplitude; DL, distal latency; EDB, extensor digitorum brevis; NCV, nerve conduction velocity. aPeroneal, tibial, and sural latencies and conduction velocities are measured in ms and m/s, respectively. Peroneal and tibial amplitudes are measured in mV while sural amplitude as μV. |
|
|
Age (y) |
46.33 ±10.42 |
|
Duration of toddy tapping (y) |
24.76 ±9.25 |
|
ATTS features (%) |
|
|
EDB atrophy |
17 (81.0) |
|
Unilateral |
11 (52.4) |
|
Bilateral |
6 (28.6) |
|
Decreased sensation in the first web space |
12 (57.2) |
|
Unilateral |
9(42.9) |
|
Bilateral |
3 (14.3) |
|
Tinel's sign |
3 (14.3) |
|
Peroneal (EDB) neuropathy |
17 (81.0) |
|
Unilateral |
9(42.9) |
|
Bilateral |
8 (38.1) |
|
Nerve conduction valuesa |
|
|
Peroneal (EDB) DAMP |
|
|
Left |
1.64 ±1.56 |
|
Right |
0.85 ±1.12 |
|
Peroneal (EDB) DL |
|
|
Left |
6.65 ±0.51 |
|
Right |
6.72 ±1.53 |
|
Peroneal (EDB) NCV |
|
|
Left |
45.21 ±4.54 |
|
Right |
43.75 ±3.57 |
|
Peroneal (tibialis anterior) DAMP |
6.83 ±2.03 |
|
Peroneal (tibialis anterior) DL |
4.58 ±0.93 |
|
Peroneal (tibialis anterior) NCV |
53.33 ±7.54 |
|
Tibial DAMP |
7.26 ±1.45 |
|
Tibial DL |
4.63 ±0.70 |
|
Tibial NCV |
49.19 ±5.11 |
|
Sural amplitude |
17.17 ±8.36 |
|
Sural DL |
2.06 ±0.29 |
|
Sural NCV |
55.60 ±8.66 |
Clinical Features of Anterior Tarsal Tunnel Syndrome
EDB atrophy was present in 81% (17/21) of participants of which 52% (11/21) had unilateral and 29% (6/21) had bilateral atrophy. Decreased sensation in the first web space was present in 57% of study participants with the majority having unilateral involvement (43%). Tinel's sign was positive in 14% of participants.
Correlational Analysis of Toddy Tapping with Electrophysiological Parameters
Pearson's correlation test showed a strong inverse association (p < 0.001)of duration of toddy tapping in years with peroneal (EDB) amplitudes on both the sides. The association with distal latencies, however, was not significant.
Discussion
Our results show a high prevalence of isolated DPN neuropathy at the ankle in asymptomatic toddy tappers. Along with, other components of ATTS, such as EDB atrophy and decreased sensation in the first web space, were also observed in high frequency. Thus, our clinical observation of a high prevalence of ATTS among toddy tappers was confirmed. The association of tapping with ATTS was further strengthened by the correlational studies which showed a strong inverse association between peroneal (EDB) amplitudes and the duration of toddy tapping.
The anterior tarsal tunnel is a relatively unprotected area in the ankle which is highly prone to external pressure. Quite commonly, even the stretch due to tight shoe straps can result in DPN injury. The nerve is kept under intense pressure when the foot is plantiflexed and digits are extended. By placing the feet in the same position, wearing high-heeled shoes results in frequent injury of DPN at the ankle.10 11In the same context, wearing gujji around the ankle for prolonged duration can traumatize DPN. Furthermore, the tappers have to keep their feet often in plantar flexion, while coming down the tree, which may also contribute to the development of ATTS. This is an uncommon entrapment neuropathy with limited scientific data available concerning its etiology, frequency of occurrence, and electrophysiological characteristics.10 11 12 13 14 A few varying etiologies have been reported in seldom published case reports. Liu et al observed 10 cases of DPN mononeuropathy at the ankle of which two patients had ganglia in the anterior tarsal tunnel, two patients developed ATTS due to talonavicular osteophytosis and another two due to tightly laced shoes, one had a contusion of the dorsal foot, while three had a pes cavus deformity.14 Akyüz et al reported ATTS in 14 cases who developed it by performing namaz over the years which resulted in chronic stretching of the DPN at the ankle.44 The strong inverse correlation of peroneal (EDB) amplitudes with number of years of tapping in our study also suggests the chronic stretching of the DPN. Respecting the existing literature, dancing is the only profession to have a strong causal association with ATTS. Our case series highlights palm tree tapping, yet another occupation to have a robust causal association with this syndrome.
The results of a singularly published large-scale study of 85 ATTS patients had reported all patients to be asymptomatic, except a dull foot ache in 19.15 The present series also reiterates the same by showing a high frequency of the disorder in asymptomatic participants. The patients with this syndrome may not present with overt motor symptoms even in an advanced stage with EDB atrophy because EDB's function is taken over by the extensor digitorum longus and extensor hallucis longus.1 16 Thus, ATTS is one disorder which may continue to exist in its subclinical form despite progressing to a severe stage.
Conclusion
Considering that peroneal (EDB) nerve study is a part of routine NCS protocol, isolated peroneal neuropathy coupled with failure to recognize ATTS may trigger further unwarranted investigations as a part of the evaluation for neuropathy and lumbosacral radiculopathy. Consequently, it becomes imperative to perform an additional peroneal (tibialis anterior) study in the cases showing abnormal EDB observations, in order not to miss the cases of ATTS. It becomes still more important to pay serious attention while performing the electrophysiological studies in selected professional groups, such as dancers and palm tree climbers.
Finally, although our observations are restricted to toddy climbers of South India, these indeed suggest palm tree climbing as a probable occupational etiology of ATTS.
Conflict of Interest
None declared.
References
- Surgical exposures for nerves of the lower limb.Nerves and Nerve Injuries. San Diego: Academic Press; 2015. p. :139-53. In: CA
- [Google Scholar]
- MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. 2010;30(4):1001-1019.
- [Google Scholar]
- Anterior tarsal tunnel syndrome. Electromyogr. Clin Neurophysiol. 2000;40(2):123-128.
- [Google Scholar]
- Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations. (3). Philadelphia: Saunders; 2013. p. :349. rd ed
- [Google Scholar]
- The anterior tarsal tunnel syndrome. Report of two cases. J Neurosurg. 1981;54(1):89-92.
- [Google Scholar]
- Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations. (3). Philadelphia: Saunders; 2012. p. :115-124. rd ed
- [Google Scholar]
- Reference values for peroneal nerve motor conduction to the tibialis anterior and for peroneal vs. tibial latencies. Am J Phys Med Rehabil. 2003;82(4):296-301.
- [Google Scholar]
- PO1.1 normative data of nerve conduction studies in 440 nerves (220 healthy Indian subjects) from university hospital, North India. Clin Neurophysiol. 2009;120:S35.
- [Google Scholar]
- [The anterior tarsal tunnel syndrome: a case report] Rev Med Liege. 2015;70:400-404. (7,8)
- [Google Scholar]
- Anterior tarsal tunnel syndrome: case report. Changge-ng Yi-xue Zazhi. 1999;22(3):503-507.
- [Google Scholar]
- Anterior tarsal tunnel syndrome: a misunderstood and a misleading entrapment neuropathy. Neurol Sci. 2014;35(5):773-775.
- [Google Scholar]






