Translate this page into:
Glioma diagnosis and comprehensive management during COVID-19 pandemic: A proposed algorithm
*Corresponding author: Djohan Ardiansyah, Department of Neurology, Faculty of Medicine-Universitas Airlangga / Dr. Soetomo General-Hospital, Surabaya, Indonesia. djohan.ardiansyah@fk.unair.ac.id
-
Received: ,
Accepted: ,
How to cite this article: Cecilia C, Ardiansyah D. Glioma diagnosis and comprehensive management during COVID-19 pandemic: A proposed algorithm. J Neurosci Rural Pract 2023;14:395-8.
Abstract
The coronavirus disease 2019 (COVID-19) has significantly changed the health-care system. COVID-19 patients with comorbidities are more likely to have severe disease, often leading to death. As one primary concern in this pandemic era, glioma patients have an incidence of 30%. It has a high mortality rate. Glioma has multiple comorbidities, at risk of contracting COVID-19, such as elderly, taking high-dose steroid therapy with adjuvant radiotherapy (RT) and chemotherapy. An algorithm for patient-doctor communication, inpatient-outpatient selection, and treatment goals in glioma patients should be carefully made according to local preparation for COVID-19. Surgery, RT, and chemotherapy should be tailored individually to increase survival rate, quality of life, and reduce the risk of COVID-19 exposure. All communication between the health-care provider and patient will be using telemedicine. The patient who requires to visit the inpatient ward will be carefully selected. Asymptomatic glioma or with no progressivity of the disease should have the treatment postponed. Symptomatic high-grade glioma patients with progressive neurological deficits and increased intracranial pressure will be treated with COVID-19 protocols. Surgery, RT, and chemotherapy, especially Temozolomide, will be given after evaluating the patient’s age, Karnofsky Performance Scale (KPS) Score, and molecular finding of O6-methylguanine DNA methyltransferase (MGMT), isocitrate dehydrogenase, and gene 1p/9q. Therefore, it is necessary to have a modified algorithm for glioma patients during this pandemic.
Key Messages:
A strategy to minimize hospital contact for glioma patients in a pandemic crisis while not delaying their diagnostics and treatments
Keywords
Glioma
Radiotherapy
Temozolomide
COVID-19
INTRODUCTION
The healthcare system worldwide has gone through tremendous change since coronavirus disease 2019 (COVID-19) started escalating from Hubei, Wuhan, in December 2019, where accessibility and communication became major issues between healthcare providers and patients. COVID-19 presents rapid transmission with high morbidity and mortality rates. The risk of infection is increasing in people with older age, cardiovascular diseases, and immunosuppressive therapy. Cancer patient is the most prevalent in using immunosuppressive treatment with other comorbidities.[1] Centre of Disease Control and Prevention states that COVID-19 patients with cancer have more severe clinical manifestations.
This crisis also has an impact on glioma patients. The incidence rate of high-grade gliomas in the United States from 2010 until 2014 was 6.0/100.000 population. The glioma incidence rate is 30% of all central nervous system (CNS) tumors, with glioblastoma multiforme (GBM) accounting for 40% of primary CNS malignancies.[2,3] Case fatality rate for cancer patients compared to non-cancer patients in the absence of COVID-19 is 5,6:2,1.[4] The study conducted by Liang et al. in cancer patients during COVID-19 pandemic showed that 38% had a higher risk of severe events. The severe events include patients requiring invasive ventilation, intensive care unit, or death. Cancerous patients have faster clinical deterioration than non-cancerous patients.[5] The incidence rate of glioma increases with age, and so do its comorbidities. In addition, high-dose steroid consumption, immunosuppressive therapy, and the risk of thromboembolic events related to the tumor make them vulnerable to COVID-19 infection.[6] Therefore, a particular modified algorithm according to each region’s policy during the pandemic era is necessary to help reduce the risk of COVID-19 exposure in hospitals and maintain health-care system accessibility.[6]
HOSPITAL MANAGEMENT OF GLIOMA PATIENTS DURING THE PANDEMIC
Guidelines for outpatient in managing patient with glioma has yet to be established, but several centers have been applying a similar concept. Telemedicine has become pivotal in the outbreak of COVID-19, which requires the collaboration of medical neurooncologists, neurosurgeons, and radiation oncologists.[1]
Patients with glioma who need outpatient care visits must undergo COVID-19 screening, wear a minimum surgical mask, and do social distancing adapted to local health protocol.[6] Patients who are compulsory to visit a hospital or clinic should be carefully selected for procedures such as brain imaging, radiotherapy (RT), urgent neurosurgery, and patients with high-grade gliomas or progressive neurological deficits.[7]
All patients admitted during the outbreak should go to the emergency unit for COVID-19 screening, including those with glioma. COVID-19 screening might vary according to the availability of the facilities in the hospital. It is recommended that highly susceptible COVID-19 patients should get 2 times reverse transcription polymerase chain reaction (RT-PCR) SARS-CoV-2 test following a negative result. Patients who need an urgent procedure in <24 h should get CT-thorax and RTPCR SARCOV-2. A meta-analysis by Mahmoud et al. showed that the CT thorax was superior in detecting early pneumonia in COVID-19, which is beneficial in screening COVID-19.[8]
Glioma patients who are positive for COVID-19 should get treatment for the infection and postpone the surgery, chemotherapy, and RT if possible; unless it is urgently needed, the procedure can be carried out using COVID-19 protocols.[1] Patients should be immediately discharged after the treatment goals are achieved to reduce in-hospital COVID-19 transmission. The patient’s selection is shown in [Figure 1].
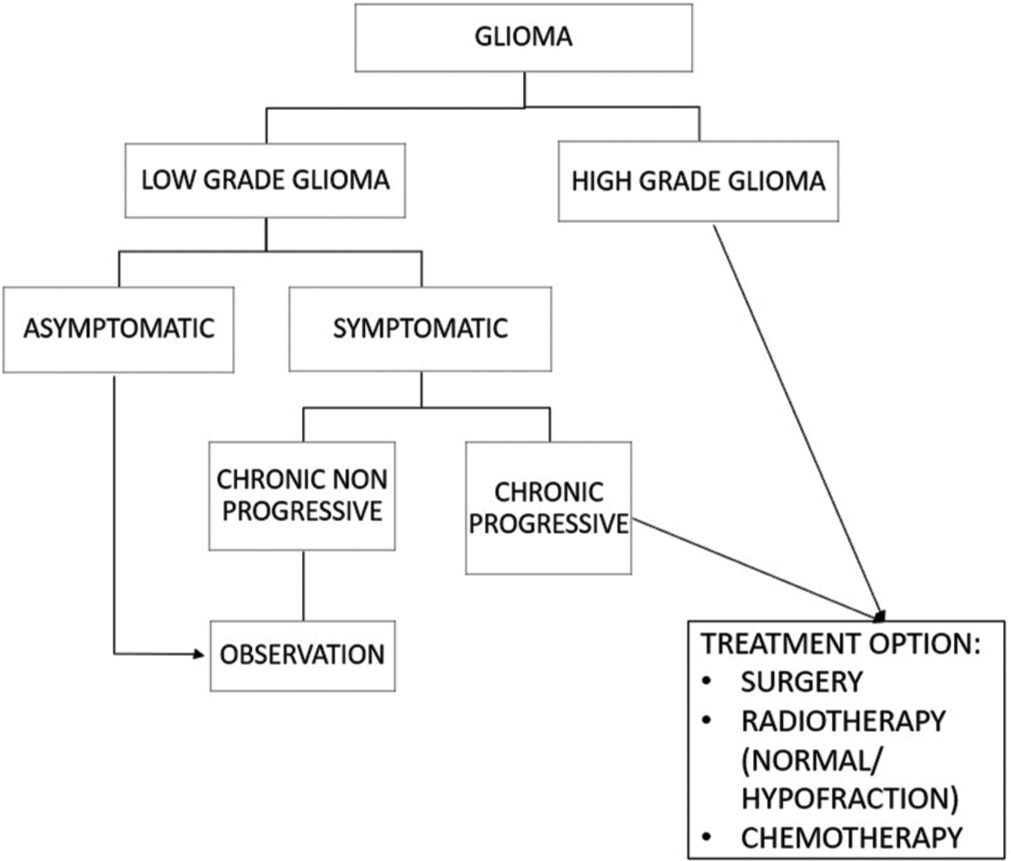
- Glioma management during COVID-19 pandemic.
SURGERY INDICATION IN GLIOMA PATIENT DURING COVID-19 PANDEMIC
The surgery rate in one of German’s neuro-oncological departments has dropped 2 weeks after the lockdown during the outbreak.[9] Neuro-oncological admission from emergency units were reduced by almost half in April 2020. European mortality monitoring activity also showed increases in mortality rate 2–3 times during this period. It not only reflects COVID-19 fatality but also delays in hospital admission and therapy postponement could be contributing factors.[9] Since many contributing factors are affecting the current situation, there still needs to be more studies about the glioma mortality rate related to surgery during the COVID-19 outbreak.[7]
Surgery goals in glioma patients are maximal safe resection to prolong survival rate, reduce symptoms, and provide the histologic and molecular diagnosis.[10] Surgical approach technique covers stereotactic core biopsy, total resection, and partial resection followed by adjuvant or concurrent chemotherapy and/or RT. The transsphenoidal and the transoral approach should be avoided due to aerosol inducing procedure.[7] Surgery for biopsy only is not recommended. Glioma diagnosis should be made by clinical and radiological findings to reduce in-hospital COVID-19 contamination.[6]
German Society of Neurosurgery (DGNC) suggest that surgery will be performed for high-grade glioma with KPS ≥60, glioma with progressive neurological deficits, and an increase in intracranial pressure, and younger patients below 40 years old are preferable.[6,9,11] This suggestion is also similar to the Professional Association of German Neurosurgeons (BDNC), several studies conducted in Italy and India. Exclusion criteria for surgery are multicentric tumor and high-grade glioma in the eloquent area.[6] COVID-19 screening procedure for emergency surgery should consist of RT-PCR SARS-CoV-2 and CT thorax.[6] Surgery in highly suspectable COVID-19 patients, regardless of their COVID-19 screening result, should be carried out in a standardized operation room such as a negative pressure operating room and proper personal protective equipment according to COVID-19 guidelines.[9] Glioma patients and families admitted to the hospital should be educated to wash their hands properly, wear protective masks, and be assisted by one family member only.[4]
Surgery for asymptomatic glioma patients or with non-progressive neurological deficits will be delayed during the outbreak. Watchful waiting and normal neuroimaging, such as magnetic resonance imaging, can be used to evaluate a patient’s condition.[6,7] Health providers should use telemedicine services to monitor each case. If needed, RT and chemotherapy will be performed as soon as possible to reduce steroid consumption.[7,10]
CHEMOTHERAPY AND RT INDICATION IN GLIOMA PATIENTS DURING COVID-19 PANDEMIC
National Comprehensive Cancer Network guidelines for RT and chemotherapy in glioma patients with modifications related to comorbidities and age in this COVID-19 outbreak are used. Clinical trial treatment should be postponed.[6] Combination of RT and chemotherapy should be evaluated individually considering patient age, KPS, and molecular statuses such as MGMT methylation, isocitrate dehydrogenase (IDH) mutation, and chromosome 1p/19q codeletion if possible.[10] If not prolonging the patient’s life and giving a good functional outcome, choosing one of the adjuvants should be considered instead of giving both.[11]
In asymptomatic low-grade glioma or with the slow progressing disease, RT can be postponed, as shown in [Figure 1].[7] Hypofractionated RT should be considered for patients with older age, poor KPS Score, and or with a high risk of COVID-19 infection. Chemotherapy with Temozolomide (TMZ) is preferable because the patients do not need hospitalization.[6] TMZ is strongly indicated for methylated MGMT and or mutant IDH gliomas.[12] Patients with unmethylated MGMT or unknown MGMT should not be given TMZ. Based on a study by Bernhardt et al., the lifespan between RT with TMZ and single RT did not show a significant difference with 12.7:11.8 months, respectively.[12]
[Figure 2] shows an algorithm for the World Health Organization Grade 3 divided into IDH mutation and IDH wild type. IDH wild type algorithm similar to algorithm for GBM. Mutant IDH or tumor with codeleted gene 1p/19q could be given conventional RT or hypo-fractionated RT with additional TMZ with very strong indication. Procarbazine, CCNU (Lomustine), and Vincristine (PCV) should be replaced with TMZ. It has a bigger immunosuppressive effect. In noncodeleted 1p/19q tumors, standard RT 60 Gy/30 fraction with or without TMZ was recommended if possible.[12]
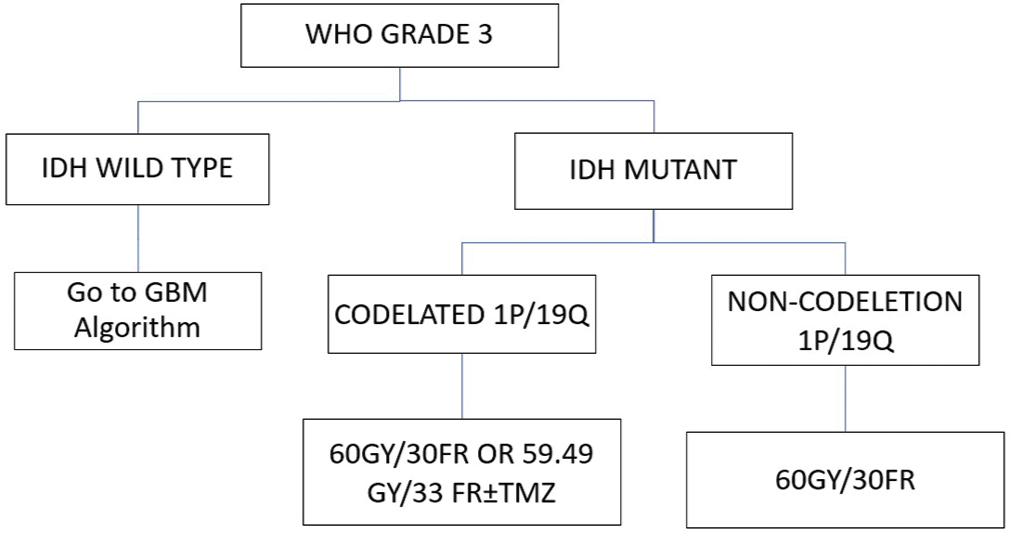
- Glioma World Health Organization Grade 3 management during COVID-19 pandemic.
GBM patients under 60 years old with a KPS score ≥60 and a low risk of contracting COVID-19 can receive normal RT 60 Gy/30 fraction. Patients with poor KPS scores or with a high risk of contraction COVID-19 should be given hypo-fractionated RT 40 Gy/15 fraction with TMZ and single 34 Gy/10 fraction or 25 Gy/5 fraction.[10,12] The study conducted by Roa et al. showed that 60 Gy in 30 fractions over 6 weeks was equivalent to 40 Gy over 3 weeks and single RT in an elderly patient (>60-years-old). They also show no survival rate difference in an elderly and frail patient who received hypofractionation RT 40 Gy/15 fractions with short course RT 25 Gy/5 fractions without TMZ.[3,12]
Patients older than 60 with a KPS score ≥60 can be given hypofractionation RT 40 Gy/15 fraction with or without TMZ. In this group with KPS<50 or Eastern Cooperative Oncology Group Score, 3–4 should be given only one of the adjuvant therapy.[6,12] In the case of methylated MGMT glioma, TMZ will be given while RT will be postponed. For patients with a high risk of COVID-19 infection, TMZ is preferred.
GBM patients aged younger than 60 years old, with good KPS (KPS ≥ 60), and no risk of COVID-19 can be given standard therapy, while in low risk and high risk of COVID-19 should be given 40 Gy/15 fraction with or without TMZ and a short course of RT 34 Gy/10 fraction or 25 Gy/5 fraction alone, respectively.
A single chemotherapy regimen is preferred compared to multiple regimens during an outbreak. In case of GBM relapse, single Bevacizumab is chosen; also PVC was replaced by TMZ.[7] if the benefits of TMZ were unclear in Glioma patients, the treatment should not be given.[13] GBM with IDH mutation and methylated MGMT should be treated with TMZ with RT.[7] Summary of the chemotherapy and RT approach is shown in [Figure 3].
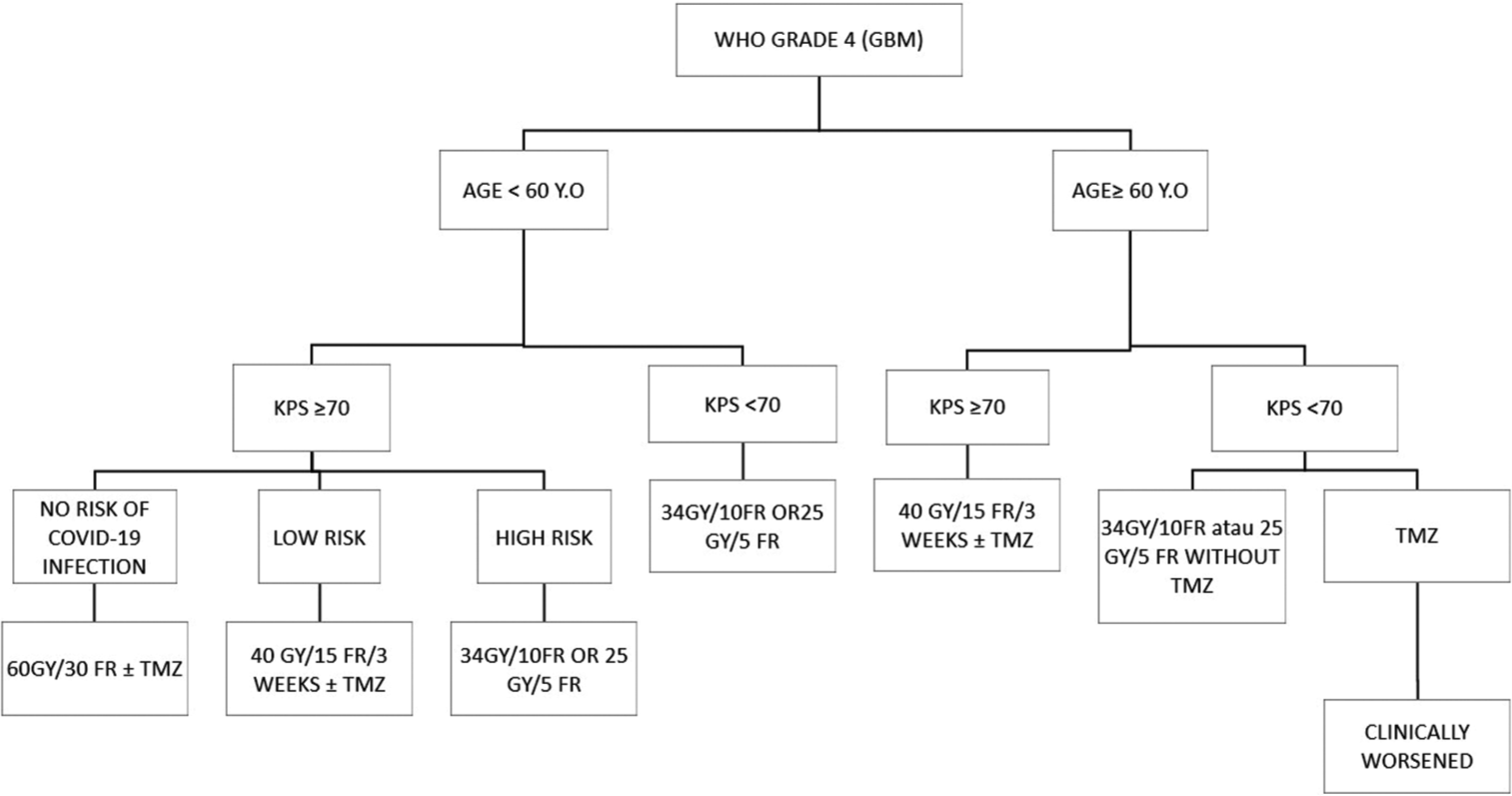
- Radiotherapy and chemotherapy approach in Grade IV glioma patients during COVID-19 pandemic.
CONCLUSION
COVID-19 has wavered all aspects of the worldwide system. It is not only focusing on COVID-19 but also affecting other diseases such as glioma. Particular guidelines are needed for glioma patients receiving RT, chemotherapy, and steroids because they are more susceptible to contracting COVID-19. Telemedicine should be used effectively during this crisis to maintain communication between patients and health-care providers. Treatment goals in glioma patients are maximal safe resection, which can improve their quality of life, shorten hospital stays, and reduce steroid usage. Clinical trial and treatment which has not been proven effective should be delayed during the outbreaks. Every treatment modality with its downside should be discussed individually with glioma patients so that they know their progression and the risk.
Acknowledgments
The author would like to thank all supervisors in the university, family, and friend who has been teaching and supporting us.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Inpatient and outpatient case prioritization for patients with neuro-oncologic disease amid the COVID-19 pandemic: General guidance for neuro-oncology practitioners from the AANS/CNS Tumor Section and Society for Neuro-Oncology. J Neurooncol. 2020;147:525-9.
- [CrossRef] [PubMed] [Google Scholar]
- Establishment of age group classification for risk stratification in glioma patients. BMC Neurol. 2020;20:310.
- [CrossRef] [PubMed] [Google Scholar]
- Abbreviated course of radiation therapy in older patients with glioblastoma multiforme : A prospective randomized clinical trial. J Clin Oncol. 2004;22:1583-8.
- [CrossRef] [PubMed] [Google Scholar]
- Radiotherapeutic management of brain tumours during the COVID-19 pandemic. J Radiother Pract. 2020;9:1-4.
- [CrossRef] [Google Scholar]
- Cancer patients in SARS-CoV-2 infection : A nationwide analysis in China. Lancet Oncol. 2020;21:335-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of patients with glioma during the COVID-19 pandemic: What we learned and what we take home for the future. Neurosurg Focus. 2020;49:E10.
- [CrossRef] [PubMed] [Google Scholar]
- Coronavirus disease 2019 pandemic and its implications on triaging patients with brain tumors for surgery, radiotherapy, and chemotherapy. Cancer Res Stat Treat. 2021;4:181-2.
- [CrossRef] [Google Scholar]
- Can chest CT improve sensitivity of COVID-19 diagnosis in comparison to PCR ? A meta-analysis study. Egypt J Otolaryngol. 2020;36:49.
- [CrossRef] [Google Scholar]
- Involuntary ambulatory triage during the COVID-19 pandemic-A neurosurgical perspective. PLoS One. 2020;15:e0234956.
- [CrossRef] [PubMed] [Google Scholar]
- Management of glioma patients during the coronavirus disease 2019 pandemic. Glioma. 2020;3:31-3.
- [CrossRef] [Google Scholar]
- How we treat patients with brain tumour during the COVID-19 pandemic. ESMO Open. 2020;4:e000789.
- [CrossRef] [PubMed] [Google Scholar]
- Neuro-oncology management during the COVID-19 pandemic with a focus on WHO grade III and IV Gliomas. Neuro Oncol. 2020;22:928-35.
- [CrossRef] [PubMed] [Google Scholar]
- Management of glioblastoma multiforme as a big challenge for neurosurgeons and radiation oncologists in Covid-19 era: An institutional experience in a rural sub-himlayan region. J Surg Surg Res. 2020;6:152-5.
- [CrossRef] [Google Scholar]







