Translate this page into:
Giant Calcified Cavernous Hemangioma Managed with Modified Double Concentric Craniotomy
Vikas Chandra Jha, MS, MCh, FINR(Zurich) Department of Neurosurgery, All India Institute of Medical Sciences Patna, Bihar India drvikaschandrajha@aiimspatna.org
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Giant calcified cavernous hemangioma is uncommon, and calvarial invasion with intracranial extension and dural breach is rare. Radiological resemblance to lesions like meningioma is unreported. Surgical excision of such lesions is technically challenging. A 35-year-old female presented with recurrent generalized tonic-clonic seizures for 2 years. Imaging suggested a highly vascular lesion arising from the skull, mimicking intraosseous meningioma, sarcoma, metastases, and so on. Double concentric craniotomy was done with lifting of bones separately around sinuses with radial cuts of dura to visualize tumor-cortical interface to safeguard neurovascular structures, and complete excision was achieved. Histopathology was suggestive of calcified cavernous hemangioma. The patient was asymptomatic at 1 year of follow-up.Differentiating angiomatous and intraosseous meningioma from calcifying giant hemangioma and other mimicking lesions may be difficult on imaging. Modified double concentric craniotomy, although used uncommonly, can be a useful technique safeguarding the neurovascular structures in its proximity.
Keywords
giant cavernous hemangioma
intraosseous meningioma
modified double concentric craniotomy
Introduction
Few skull tumors attain large size with breach of inner and outer tables, like intraosseous meningioma, sarcomas, hemangioma, fibrous dysplasia, metastases, etc. Differentiating them on imaging presents a technical challenge. Hemangioma comprises 10% of skull lesions, but giant calcified cavernous hemangioma are rare.1 These enhance brilliantly on contrast computed tomography (CT)/magnetic resonance imaging (MRI) and have a “sunburst” appearance on angiography. While preoperative embolization may be helpful in decreasing vascularity, craniotomy with visualization of meninges all-around for vascular control and avoidance of sinus injury is paramount in reducing the surgical morbidity.2 3 Double concentric craniotomy (DCC) may safeguard the vital neurovascular structures.4 In giant and diffuse lesions, partial modification with additional calvarial removal over the sinuses further reduces the risk of vascular injury which has been clearly demonstrated by this case report. This case is being reported for its rarity and the utilization of modified surgical technique for its management.
Case Presentation
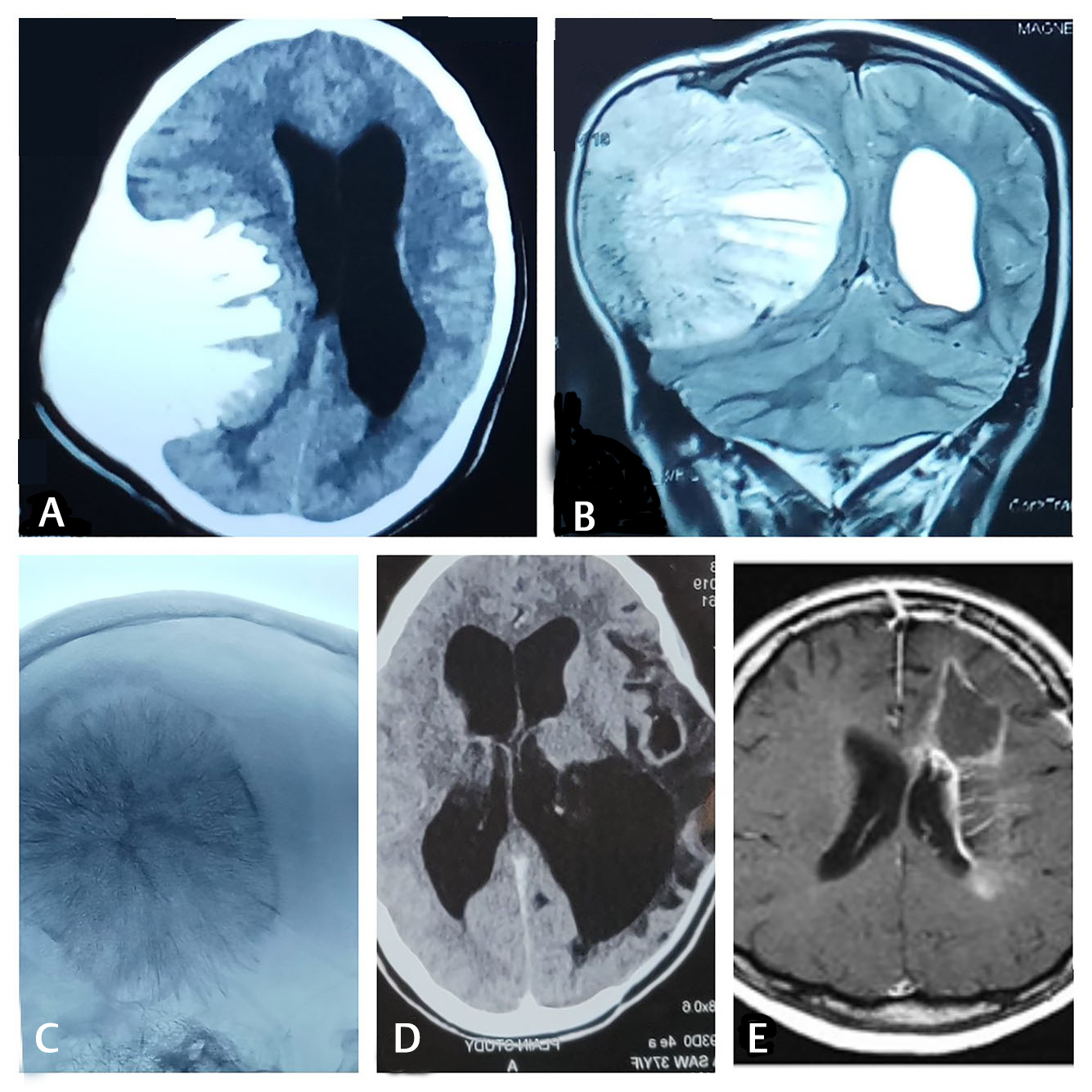
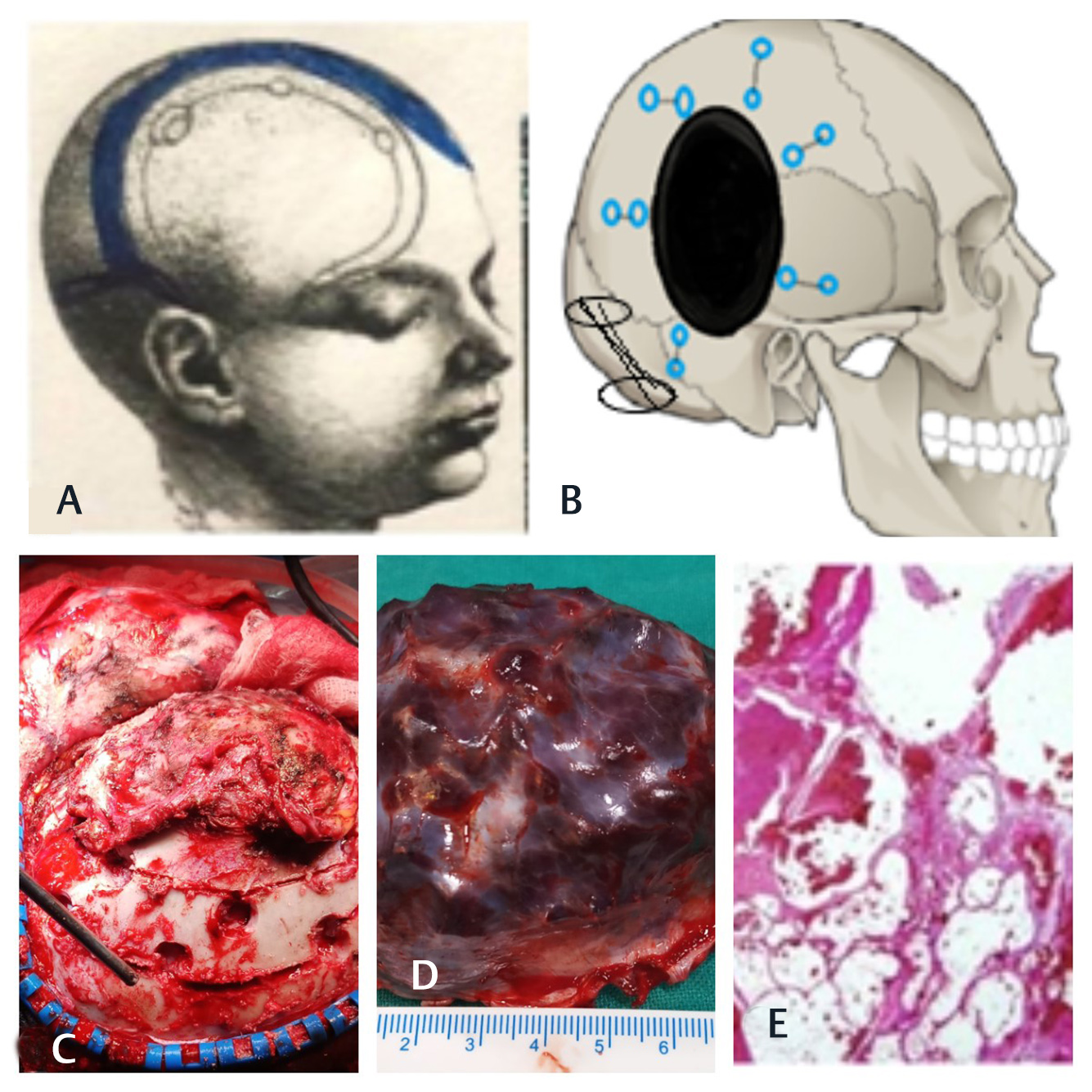
A 35-year-old female presented with persistent diffuse headache and recurrent generalized tonic-clonic seizures for 2 years. Nothing specific was noted on neurological examination. Contrast enhanced computerized tomography head revealed a 10 × 7 × 7-cm hyperdense, spiculated lesion arising from the intradiploic space, breaching the inner and outer tables of the skull with major intracranial extension. MRI revealed a hyperintense lesion with intermittent hypointensities on T1 sequence, which was contrast enhancing too. A lesion with arborizing pattern and tumor blush, suggesting high vascularity, was noted on digital subtraction angiography (DSA) (Fig. 1A–D). Differential diagnoses included angiomatous/intraosseous meningioma, sarcoma, metastases, and fibrous dysplasia, etc. Total excision of the lesion was planned by concentric craniotomy (CC)—making multiple burr holes in two concentric circles around the lesion. As the tumor was widely involving the calvarium and normal dura was not exposed, a third outer ring around the lesion and sinuses was performed to take control of the meningeal feeders. Bone strip around the transverse-sigmoid junction was lifted separately by making burr holes on both inner and outer sides. Radial dural cuts around the tumor were made to visualize the interface between tumor and brain parenchyma. The extradural upper half of the tumor was removed piecemeal with drill, while the lower (intradural) half was mobilized by creating a plane of dissection between tumor and cortical tissue (Fig. 2A–D).
-
Fig. 1 (A) Axial CT showing hyperdense lesion with spikes like projections medially involving calvaria. (B) T2 coronal MRI showing hypoattenuating cleft between hyperattenuating lesion extending to midline compressing brain parenchyma. (C) Digital subtraction angiography showing supply from middle cerebral artery with tumor blush. (D) Immediate postoperative CT suggesting complete removal. (E) T2 axial MRI on follow up suggesting complete removal with cranioplasty. CT, computed tomography; MRI, magnetic resonance imaging.
Fig. 1 (A) Axial CT showing hyperdense lesion with spikes like projections medially involving calvaria. (B) T2 coronal MRI showing hypoattenuating cleft between hyperattenuating lesion extending to midline compressing brain parenchyma. (C) Digital subtraction angiography showing supply from middle cerebral artery with tumor blush. (D) Immediate postoperative CT suggesting complete removal. (E) T2 axial MRI on follow up suggesting complete removal with cranioplasty. CT, computed tomography; MRI, magnetic resonance imaging.
-
Fig. 2 (A, B) Schematic illustration of burr hole placement and craniotomy. (C) Intraoperative image showing extensive calvaria involvement with modified double concentric craniotomy. (D) cortical surface of excised tumor, spiculated, calcified with brownish black appearance of max diameter 10 cm. (E) Histopathology of excised lesion suggestive of dilated venous sinus with thrombus and occasional central and peripheral calcifications suggestive of calcified cavernous hemangioma.
Fig. 2 (A, B) Schematic illustration of burr hole placement and craniotomy. (C) Intraoperative image showing extensive calvaria involvement with modified double concentric craniotomy. (D) cortical surface of excised tumor, spiculated, calcified with brownish black appearance of max diameter 10 cm. (E) Histopathology of excised lesion suggestive of dilated venous sinus with thrombus and occasional central and peripheral calcifications suggestive of calcified cavernous hemangioma.
Histopathology suggested giant cavernous hemangioma with scattered calcification (Fig. 2E). Postoperative contrast CT indicated complete removal of the lesion (Fig. 1D,E). At 1-year follow-up, patient was neurologically intact, cranioplasty with polyacrylate graft was performed for remaining bony defect.
Discussion
Hemangiomas are common in the vertebrae but are rare in the skull, comprising less than 1% of total.4 5 6 Cavernous hemangioma grows slowly in the diploic space and usually erodes the outer table of the skull. Breach of both outer and inner tables with calcification, intracranial extension and breach of dura with such giant size is rare, and only few cases are reported till date.6 7
Presently, there exists no fixed criteria to classify a cavernous hemangioma as giant; however, we have considered the lesion in our case as giant based on the proposition by Lawton et al,2 where lesion larger than 6 cm was classified as giant and in present study lesion had a maximum diameter of 10 cm.
Patients with cavernous malformations (CMs) typically present with a hemorrhagic event and dull aching pain due to undue traction on the underlying brain surface.2 3 4 5 6 Our case, however, presented with recurrent generalized tonic-clonic seizures—possibly due to repeated intratumoral bleed and edema in the brain parenchyma surrounding the lesion (which had an insidious and expansible growth).
In the present case, due to extensive calcification and involvement of temporal, parietal and occipital calvaria with giant size tumor and its close proximity to the sinuses, we performed CC by putting burr holes around tumor and adjacent to sinuses in concentric fashion making it triple concentric and raised boneflap separately around the sinuses exposing healthy dura around tumor. Radial dural cuts facilitated cortical-tumor interface visualization with safe excision. Various ways of performing concentric craniotomies have been described in the literature. Kao et al had suggested the use of two burr holes (one on either side of the tumor and performing inner craniotomy by joining the inner edge and outer craniotomy by joining the outer edge of burr holes),8 but this technique would not be feasible for lesion with close proximity to the sinuses as cortico-tumoral interface might not be adequately visualized, thereby increasing the risk of its injury to nearby neurovascular structure. Another technique of CC, proposed by Michael et al, named as DCC. Here, the first concentric ring around the tumor attached to the skull was left undisturbed and a second wider CC was used to expose the normal dura.9 However, in his case, there was no dural breach, but in tumors with large intradural component and dural breach, radial dural cuts would facilitate visualization of tumor cortical interface, thereby ensuring complete excision of tumor and safeguarding neurovascular structure.
CC had been performed for different lesions involving the skull, with intracranial extension. Details of these cases are summarized in Table 1. Spennato et al performed DCC for the removal of calvarial nail following penetrating injury of the skull, and Sekhar et al performed it for fronto-orbital meningioma and Ibarra DelaTorre et al for posterior fossa medulloblastoma, etc.10 11 12 Tumor in present patient study differs from previous reported cases as it was larger in size, completely calcified, spiculated medial margins, involving medial cranial fossa, highly vascular with dilated intraosseous arteries and veins, and in close proximity to transverse and sigmoid sinuses for which triple CC was performed. To the best of my knowledge, this technique of modified DCC had been performed for the first time to excise tumor with intra- and extracranial extension and thus needs mention. Plastic reconstruction is always a concern, and in majority of the cases cranioplasty is done by acrylate graft, as in this case.2 4 8
|
S. No. |
Study (Year) |
Age (y) |
Clinical presentation |
Gender |
Tumor size (cm) |
Surgical technique |
HPE |
|---|---|---|---|---|---|---|---|
|
Abbreviations: DCC, double concentric craniotomy; F, female; HPE, histopathology; lt, left; M, male; Rt, right. |
|||||||
|
1 |
Fornaro et al4(2015) |
45 |
Skull swelling |
M |
5 cm |
DCC + cranioplasty (single burr hole lateral to sagittal sinus with cc from inner and outer edge of burr hole |
Atypical meningioma without medial spiculated margin and mainly convexity not in proximity to sinuses |
|
2 |
Michael et al9(2014) |
32 |
Skull swelling |
M |
5 cm |
DCC |
Hemangioma with intracerebral extension without dural breach and extracranial extension |
|
3 |
Kao et al8(2016) |
15 |
Scalp swelling |
M |
8 cm |
DCC + cranioplasty |
Ewing’s sarcoma no proximity to sinus, no spiculation, no diffuse calcification and dural breach |
|
4 |
Spennato et al10 (2005) |
25 |
M |
1 |
DCC + cranioplasty |
Nail removal |
|
|
5 |
Sekhar et al11 (1999) |
45 |
M |
5 cm |
DCC + cranioplasty |
Spheno-orbital meningioma not in proximity to sinus |
|
|
6 |
Ibarra DelaTorre et al12 (2012) |
35 |
Posterior fossa tumor |
M11F6 |
4 cm |
Concentric craniotomy |
Medulloblastoma glioma pineal region tumor No calcifying lesion with calvarial invasion |
|
7 |
Present case |
35 |
Fronto-parietal-occipital swelling |
F |
10 cm |
Calcified cavernous hemangioma, spiculated medial margin with close proximity to transverse and sigmoid sinus |
|
Conclusion
Differentiating angiomatous/intraosseous meningioma from calcifying giant hemangioma and other mimicking lesions may be difficult on imaging. Modified double CC is a useful technique safeguarding the neurovascular structures in proximity, for the giant vascular lesions arising from dura or calvaria and extending both intracranially and extracranially.
Conflict of Interest
None declared.
Funding None.
References
- Giant infiltrative cavernous malformation: clinical presentation, intervention, and genetic analysis: case report. Neurosurgery. 2004;55(4):979-980.
- [Google Scholar]
- Giant calvarial cavernous hemangioma: a rare case report and review of literature. Asian J Neurosurg. 2019;14(2):578-580.
- [Google Scholar]
- Double concentric craniotomy: safe and effective technique to achieve an en bloc resection of tumor involving both skull and duraa. Int J Surg Case Rep. 2015;12:117-119.
- [Google Scholar]
- Giant primary ossified cavernous hemangioma of the skull in an adult: a rare calvarial tumor. J Neurosci Rural Pract. 2011;2(2):174-177.
- [Google Scholar]
- Calvarial bone cavernous hemangioma with intradural invasion: an unusual aggressive course-Case report and literature review. Int J Surg Case Rep. 2016;22:79-82.
- [Google Scholar]
- Modified concentric craniotomy for the removal of a huge calvarial metastatic tumor: technical note. Childs Nerv Syst. 2016;32(2):365-368.
- [Google Scholar]
- Concentric craniotomy: removal of tumor involving the skull and the intracranial space. World Neurosurg. 2014;81:651.e15-651.e16. (3-4)
- [Google Scholar]
- Double concentric craniotomy for a craniocerebral penetrating nail. Case report and technical note. Surg Neurol. 2005;64(4):368-371.
- [Google Scholar]
- Fronto-orbital approach. In: Sekhar L., de Oliveira E., eds. Cranial Microsurgery Approaches and Techniques. Thieme; New York: 1999:54-60.
- [Google Scholar]
- Suboccipital concentric craniotomy as variant for posterior cranial fossa surgery. In: Signorell, ed. Explicativ Cases of Controversial Issues in Neurosur-gery. InTech; New York: 2012:87-96.
- [Google Scholar]






