Translate this page into:
Ganglioglioma Arising from the Septum Pellucidum
Bishal Shrestha, MBBS Department of Neurosurgery, Annapurna Neurological Institute and Allied Sciences Maitighar, Kathmandu, +977 Nepal cantona7best@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
A 24-year-old gentleman presented to us with complaints of occasional headache for 2 years. Magnetic resonance imaging showed enhancing supra sellar mass with nonenhancing cystic components, extending superiorly up to the body of bilateral lateral ventricle, laterally displacing septum pellucidum, and compressing the third ventricle with obstructive hydrocephalus. Hormone profile depicted adrenocorticotropic hormone <5.00 pg/mL, growth hormone 1.32 ng/mL, insulin-like growth factor-1 <3.0 ng/mL. The patient underwent surgical resection. Histological finding was suggestive of ganglioglioma World Health Organization grade I. Customized immunohistochemistry panel was advised and revealed positive CD 56, NSE, and GFAP immunohistochemical stains. Gangliogliomas are less frequent neoplastic lesions confined to only a handful of case reports and studies. Accounting less than 2% of intracranial neoplasms, these lesions primarily affect those in the first 3 decades of their life. As ubiquitous it is in nature, we hereby present a case of ganglioglioma in a young adult male arising from septum pellucidum.
Keywords
ganglioglioma
septum pellucidum
brain neoplasm
Introduction
Gangliogliomas are World Health Organization Grade I, well-differentiated, benign tumor of glioneuronal origin.1 2 Perkins, in 1926, was the first to coin the term ganglioglioma. Documented to comprise 3% of all primary brain neoplasms, demographic studies have shown that this tumor primarily affects children and young adult with male sex preponderance (male:female: 1.9:1) and peak age of occurrence at 11 years.3 Despite being an omnipresent entity, most of these lesions are supratentorial, affecting the temporal lobes (>70%), in the basal diencephalon; the hypothalamus and within the vicinity of its slit-like cerebrospinal fluid cavity; and the third ventricle or the frontal lobes.1 4 However, they are found to rarely involve the brainstem. The most common mode of presentation is seizure or change in the pattern of preexisting seizure activity which are usually refractory to pharmacotherapy. Other neurological manifestations are based on the site of the neoplasm. Following a complete resection, this is associated with a favorable 10-year survival rate as high as 82 to 93%.3
Only a few cases of intraventricular ganglioglioma have been reported making it a rare entity. As scarce is the lesion, septum pellucidum gangliogliomas are so few and far between that there are only three cases described as of now,5 6 7 and we report a clinical vignette in a patient who underwent complete surgical resection of the tumor.
Case Report
A 24-year-old gentleman showed up to our institution who had the chief condition of occasional headache for 2 years. It was gradual in onset, involving the bilateral temporal region, mild in intensity, on and off recurring every 3 to 4 days, without any aggravating or relieving factors. It then increased in severity and became continuous in nature for 15 days. Later, it was followed by blurring of vision of right eye. General examination revealed angiofibromas involving his face, ear lobules, nape of the neck, and shagreen patches over his lower back. Examination of visual acuity revealed loss of temporal vision of his right eye. Rest of the neurological examinations was unremarkable.
Magnetic resonance imaging (MRI) scan of the brain demonstrated T1/T2 isointense avidly enhancing suprasellar space occupying lesion with nonenhancing cystic components, extending superiorly up to the body of bilateral lateral ventricle, laterally displacing septum pellucidum and compressing the third ventricle with obstructive hydrocephalus (Fig. 1A–C). Hormone profile depicted adrenocorticotropic hormone <5.00 pg/mL, growth hormone 1.32 ng/mL, and insulin-like growth factor-1 <3.0 ng/mL.
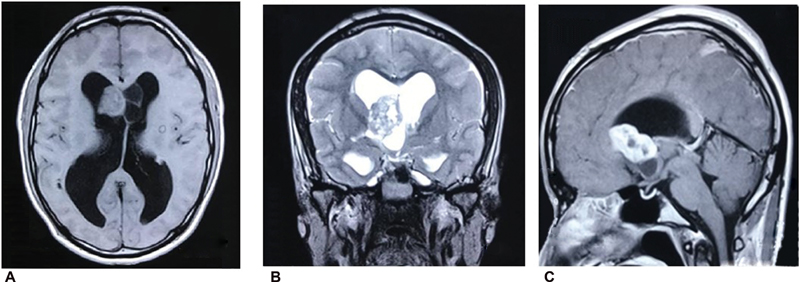
-
Fig. 1 (A) T1 axial isointense supra sellar mass (3.9 cm × 3.5 cm × 2.4 cm) with cystic component extending superiorly up to the body of B/L lateral ventricle. (B) T2 coronal isointense mass atop the sellar region laterally displacing septum pellucidum causing compression on the third ventricle with obstructive hydrocephalus. (C) Contrast-enhanced MRI showing nonenhancing cystic component. MRI, magnetic resonance imaging.
Fig. 1 (A) T1 axial isointense supra sellar mass (3.9 cm × 3.5 cm × 2.4 cm) with cystic component extending superiorly up to the body of B/L lateral ventricle. (B) T2 coronal isointense mass atop the sellar region laterally displacing septum pellucidum causing compression on the third ventricle with obstructive hydrocephalus. (C) Contrast-enhanced MRI showing nonenhancing cystic component. MRI, magnetic resonance imaging.
Bicoronal craniotomy, interhemispheric transventricle transseptal strategy, and gross total surgical clearance of the tumor in piecemeal were achieved (approximately 4 cm × 4 cm × 3 cm, soft to firm in consistency, and moderately vascular lesion involving the anterior horn of right ventriculus lateralis encroaching into septum pellucidum and floor of the third ventricle with heterogeneous tissue architecture containing cystic masses in the contralateral ventricle).
Histopathological examination was suggestive of ganglioglioma with dysplastic ganglion cells in a disorganized pattern and clustering in a fibrillary background. Few of these cells have cytomegaly and pleomorphism with prominent nucleoli. Astrocytic component showed increased cellularity. Brightly eosinophilic round granular bodies of variable size and Rosenthal fibers, which are elongated “cork screw” eosniophilic intracellular inclusions, are also seen (Fig. 2A,B).
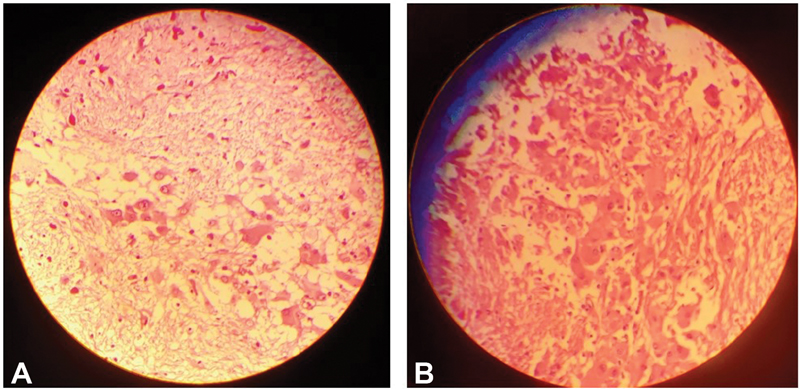
-
Fig. 2 (A) Histopathological examination showing dysplastic ganglion cells in a disorganized pattern and clustering in a fibrillary background. Few of these cells exhibit cytomegaly and pleomorphism with prominent nucleoli. Astrocytic component showing increased cellularity. Eosinophilic round granular bodies and intranuclear Rosenthal fibers are appreciated (magnification 10 × ). (B) Magnification 40 × .
Fig. 2 (A) Histopathological examination showing dysplastic ganglion cells in a disorganized pattern and clustering in a fibrillary background. Few of these cells exhibit cytomegaly and pleomorphism with prominent nucleoli. Astrocytic component showing increased cellularity. Eosinophilic round granular bodies and intranuclear Rosenthal fibers are appreciated (magnification 10 × ). (B) Magnification 40 × .
Customized immunohistochemistry panel was advised and revealed immunoreactive CD 56, NSE, and GFAP suggestive of ganglioglionic cells and Ki-67 immunoreactive in only 1 to 2% of lesional cells suggestive of benign morphology (Fig. 3).
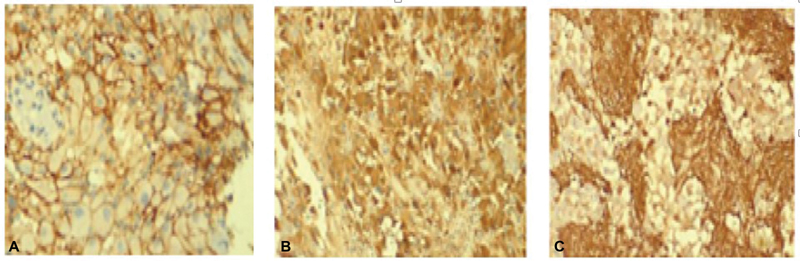
-
Fig. 3 Immunohistochemistry immunoreactive for (A) CD 56, (B) NSE, and (C) GFAP.
Fig. 3 Immunohistochemistry immunoreactive for (A) CD 56, (B) NSE, and (C) GFAP.
The postoperative course was uneventful and the patient improved with no neurological deficits. The patient was discharged on 10th day in an ambulatory state with no neurological deficits.
Discussion
It dates back to early 19th century when the general rule for applying a new label to a newly identified growth must fulfill the criteria that it should be able to explain the etiology, describe its location, its histological features, or, preferably, its histogenesis. The nomenclature of ganglioglioma has evolved over time with different terms linked to the pathology to indicate the chief features of its constituent elements. Perkins, in 1926, first coined the term ganglioglioma. In 1930, Courville provided a review of 20 cases of ganglioglioma.8
Accounting for an approximately 2% of intracranial lesions, gangliogliomas are composed of dysplastic neuronal and glial cells. They are found frequently in the supratentorial compartment, most common than not in the temporal lobe (84%).9 However, they have been encountered anywhere along the neuraxis, namely, frontal (10%), occipital (2%), and parietal lobes, along with the spinal cord, optic chiasm, and the pineal gland. Intraventricular gangliogliomas and brainstem gangliogliomas are rare with only 26 cases10 and 3 cases11 described in literature, respectively.
Gangliogliomas are found often in males with an average age at presentation to be ranging in between 16 and 29 years.4 However, some variants of ganglioglioma are more frequent in male,12 while some have and equal sex distribution.9 The usual mode of presentation is due to signs and symptoms of raised intracranial pressure, focal neurological deficit, or seizure.4 Contrary to the usual clinical scenario of seizure, our patient had no such manifestation. The duration of symptoms was found to range from 3 months to 45 years of age (mean age: 11 years) by the time the patient presented for surgical intervention.9
The preferred treatment resort for ganglioglioma is surgery, the extent of resection depending upon intraoperative circumstances. Surgery is the greatest predictor of prognosis.12 Outcomes in the form of complete resolution of symptoms, partial improvement of symptoms, and death have been reported with surgical intervention. In those ineligible for complete resection due to tumor geography and potential hazardous neurological deficit following surgery, gamma knife radiosurgery is considered as an alternative.13
Gangliogliomas appear as a hypodense lesion in computed tomography (CT) scan with variable degrees of enhancement and foci of calcifications.14 The pattern of enhancement may be seen either in the form of homogeneous or inhomogeneous enhancement. Rarely, the tumor may not be visible at all even in a contrast-enhanced CT.9
In a MRI, gangliogliomas have a multitude of appearances. Approximately 20 to 40% appear hypointense while 40 to 70% are isointense in T1-weighted MRI.3 Likewise, in T2-weighted MRI, they appear isointense in 20 to 30% and hyperintense in 70 to 90%.
Based on an imaging alone, a conclusive diagnosis of intraventricular ganglioglioma cannot be made. Presurgical possibilities such as ependymoma, subependymoma, astrocytoma, choroid plexus papilloma, germ cell tumor, neurocytoma, and metastasis should be considered in the list of differential diagnoses.
Conclusion
We have presented a very rare case of ganglioglioma arising from the septum pellucidum. Definite diagnosis prior to histopathological examination based on clinical and radiological features is often fallacious. It is therefore necessary to do a histopathological study and immune histological analysis to corroborate the diagnosis. Complete resection, if achieved, has a better prognosis in terms of progression-free survival.
Conflict of Interest
None declared.
References
- Gangliogliomas: an intriguing tumor entity associated with focal epilepsies. J Neuropathol Exp Neurol. 2002;61(7):575-584.
- [Google Scholar]
- The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803-820.
- [Google Scholar]
- Cerebral gangliogliomas: clinical characteristics, CT and MRI. Acta Neurochir (Wien). 1999;141(2):135-141.
- [Google Scholar]
- Ganglioglioma: single-institutional experience of 24 cases with review of literature. Asian J Neurosurg. 2016;11(4):407-411.
- [Google Scholar]
- Ganglioglioma in the bilateral ventricles arising from the septum and extending to the third ventricle. Clin Neuropathol. 2015;34(1):50-53.
- [Google Scholar]
- Intraventricular ganglioglioma with bleed: a rare case report. Neurol India. 2010;58(3):477-480.
- [Google Scholar]
- Ganglioglioma: Tumor of the central nervous system; review of the literature and report of two cases. Arch Neurol Psychiatry. 1930;24(3):439-491.
- [Google Scholar]
- Gangliogliomas: clinical, radiological, and histopathological findings in 51 patients. J Neurol Neurosurg Psychiatry. 1994;57(12):1497-1502.
- [Google Scholar]
- Ganglioglioma arising from the septum pellucidum: case report and review of the literature. Pediatr Neurosurg. 2019;54(1):36-45.
- [Google Scholar]
- Ganglioglioma of the brainstem: report of three cases and review of the literature. Surg Neurol. 2001;56(5):315-322. , discussion 322–324
- [Google Scholar]
- Supratentorial gangliogliomas: histopathologic grading and tumor recurrence in 184 patients with a median follow-up of 8 years. Cancer. 2004;101(1):146-155.
- [Google Scholar]
- Treatment and outcomes for gangliogliomas: a single-center review of 16 patients. Brain Tumor Res Treat. 2014;2(2):49-55.
- [Google Scholar]
- Intracranial ganglioglioma: clinicopathological and MRI findings in 16 patients. Clin Radiol. 2008;63(1):80-91.
- [Google Scholar]






