Translate this page into:
External Validation of the Rotterdam Computed Tomography Score in the Prediction of Mortality in Severe Traumatic Brain Injury
Address for correspondence: Dr. Jose D. Charry, Fundacion Universitaria Navarra, Calle 10 No. 6-41, Neiva, Colombia. E-mail: danielcharry06@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Traumatic brain injury (TBI) is a public health problem. It is a pathology that causes significant mortality and disability in Colombia. Different calculators and prognostic models have been developed to predict the neurological outcomes of these patients. The Rotterdam computed tomography (CT) score was developed for prognostic purposes in TBI. We aimed to examine the accuracy of the prognostic discrimination and prediction of mortality of the Rotterdam CT score in a cohort of trauma patients with severe TBI in a university hospital in Colombia.
Materials and Methods:
We analyzed 127 patients with severe TBI treated in a regional trauma center in Colombia over a 2-year period. Bivariate and multivariate analyses were used. The discriminatory power of the score, its accuracy, and precision were assessed by logistic regression and as the area under the receiver operating characteristic curve. Shapiro–Wilk, Chi-square, and Wilcoxon tests were used to compare the real outcomes in the cohort against the predicted outcomes.
Results:
The median age of the patient cohort was 33 years, and 84.25% were male. The median injury severity score was 25, the median Glasgow Coma Scale motor score was 3, the basal cisterns were closed in 46.46% of the patients, and a midline shift of >5 mm was seen in 50.39%. The 6-month mortality was 29.13%, and the Rotterdam CT score predicted a mortality of 26% (P < 0.0001) (area under the curve: 0.825; 95% confidence interval: 0.745–0.903).
Conclusions:
The Rotterdam CT score predicted mortality at 6 months in patients with severe head trauma in a university hospital in Colombia. The Rotterdam CT score is useful for predicting early death and the prognosis of patients with TBI.
Keywords
Neurological outcome
prognosis models
traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is a major disease with a significant impact at the global level. Incidence has been reported close to 200 cases per 100,000 people worldwide.[1] According to the Global Burden of Disease Study published in 2010 by the World Health Organization, trauma remains a public health problem and generates an important burden of disease in health-care systems in Latin American countries.[23] In Colombia, the burden of injuries particularly affects the male, economically active population aged between 12 and 45 years old. In 2013, 26,000 deaths were due to trauma and most of them were associated with interpersonal violence. Of these injuries, a large percentage was associated with closed and penetrating TBI.[4]
TBI remains the main cause of death and disability in young adults worldwide.[56] It is a heterogeneous disease with respect to cause, pathology, severity, and prognosis. This results in considerable uncertainty in the expected outcome of individual patients. Several outcome prediction models have been developed for the prognosis of TBI patients to help ease this uncertainty.[7] These prognostic models can be used to combine different characteristics of individual patients to predict their clinical outcome. Prognostic models may also be useful as tools to compare outcomes across institutions, health-care systems, and countries, and may be an essential part of the planning of new studies in the field of brain injury.
The Glasgow Outcome Scale (GOS) is a general measure widely used in TBI management and surgery outcome studies.[8] Another diagnostic technique for assessing TBI is brain imaging by computed tomography (CT) and magnetic resonance imaging. Brain imaging significantly helps the early diagnosis and the effective treatment of life-threatening conditions in patients with TBI.[9] However, the brain CT is the gold standard for assessing patients with acute TBI. Currently, there are two CT-based systems for evaluating CT findings, the Marshall Classification System (MCS) and the Rotterdam Scoring System (RSS).[1011] The MCS, developed by Marshall et al. in 1991, was the first CT-based system for determining the prognosis of TBI. The MCS classifies CT findings into four grades: Grade 1, no pathologic findings; Grade 2, basal cisterns are present and midline shift is <5 mm; Grade 3, basal cisterns are compressed; and Grade 4, midline shift is >5 mm.[10] This system was developed primarily for predicting patient outcomes and the risk for increased intracranial pressure in patients with severe TBI. In 2005, Maas et al. introduced the RSS. This system provides a better estimation of disease prognosis using certain criteria such as basal cisterns’ condition, midline shift, traumatic subarachnoid or intraventricular hemorrhage, and the epidural hematoma. Rotterdam scores predict posttrauma 6-month mortality rate as follows: score 1, 5%; score 2, 7%; score 3, 16%; score 4, 26%; score 5, 53%; and score 6, 61%.
In this study, we aimed to examine the accuracy of the prognostic discrimination and prediction of mortality of the Rotterdam CT score in a cohort of trauma patients with severe TBI in a university hospital in Colombia.
MATERIALS AND METHODS
Patient population
This retrospective, observational cohort study was performed at Neiva University Hospital (NUH) in Southern Colombia. Patients with severe TBI who were admitted at NUH between January 2014 and December 2015 were included in the study. Approval from the NUH quality improvement office and the Institutional Review Boards of NUH was obtained prior to conducting this study.
NUH is a 504-bedded, level I trauma center, and tertiary referral hospital in Southern Colombia that admits approximately 2000 adult trauma patients per year and has 30 adult ICU beds. This hospital is the primary trauma center for 3.2 million inhabitants living in a region extending over 60,000 square miles. Patients in the age group of 18 years or older and suffering from TBI defined as a score of ≤8 points on the Glasgow Coma Scale (GCS) clinical outcome. The variables and results were evaluated according to the GOS at 6 months’ postinjury, and a dichotomous variable with favorable outcome (GOS 4 or 5) and unfavorable outcome (GOS 1–3) was created.[1213] In addition, we evaluated the prediction of mortality that was given by Rotterdam CT score versus those obtained in the study patients.
Prediction of outcome
We used the RSS which provides a better estimation of disease prognosis using certain criteria such as basal cisterns’ condition, midline shift, traumatic subarachnoid or intraventricular hemorrhage, and epidural hematoma. Rotterdam scores predict posttrauma 6-month mortality rate as follows: score 1, 5%; score 2, 7%; score 3, 16%; score 4, 26%; score 5, 53%; and score 6, 61%.[10]
Statistical analysis
Values are reported as median. Discrete variables are reported as median and range. Logistic fit and receiver operating characteristic (ROC) statistics were used as indicated. The statistical software used was SSPS Statistic (Version 21, IBM, Corporation, Pittsburgh, United States) and the R software environment (Version 2.15.2, The R Foundation for Statistical Computing, Vienna, Austria). P < 0.05 was regarded statistically significant. The discriminatory power of the models, its accuracy, and precision were assessed by logistic regression and as the area under the ROC curve (area under the curve [AUC]). Shapiro–Wilk, Chi-square, and Wilcoxon tests were used to compare real outcomes in the cohort against predicted outcomes and a multivariate logistic regression analysis was performed. We excluded variables that were not significant at 5% level. We quantified each variable's predictive contribution by its z score (the model coefficient divided by its standard error). We explored linearity and interactions between the variables, and all predictors were evaluated by P value and the Confidence interval (CI).
RESULTS
A total of 127 patients were admitted with a diagnosis of severe TBI over a period of 2 years in the NUH. A8 Median age was 33 years, 84.25% were male, blunt trauma was in 88.98% of the patients. Imaging findings showed that 50.39% of the patients had closed basal cisterns. 46.46% had midline shift, and 20.47% had epidural hematoma was present in CT scan. The characteristics of the 127 patients included and this is one of the most common causes of TBI. 1 in this study are described in Table 1.
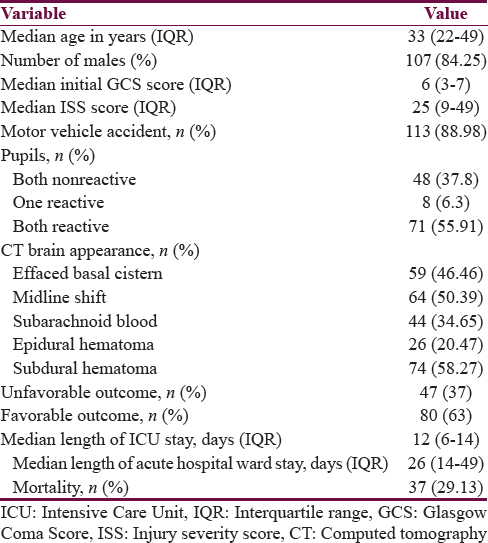
The 6-month mortality was 29.13%, and the Rotterdam CT score predicted a mortality of 26% (P < 0.0001) (AUC: 0.825; 95% confidence interval: 0.745–0.903). These results are shown in Figure 1.
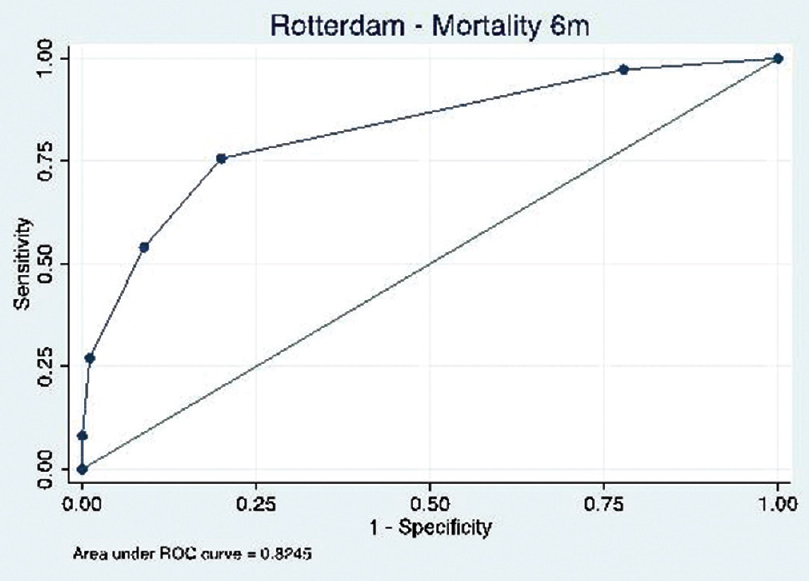
- Area under the curve of Rotterdam score for 6-month mortality
DISCUSSION
TBI is a medical and surgical disease of major importance globally.[8] The World Health Organization predicts that traffic accidents will be the third leading cause of illness and injuries worldwide by 2020, and this is one of the most common causes of TBI. Prognostication is important when considering outcome, especially when considering a potentially lifesaving. Traditionally, neurosurgeons have relied on individual clinical parameters such as age, the initial GCS score, and pupillary responses combined with a radiological assessment to guide clinical decisions and when counseling family members and surrogate decision makers regarding prognosis.[111415] Different models have been described for predicting mortality and adverse neurological outcome in TBI patients, the best known are Marshall CT score, Rotterdam CT score, and IMPACT CRASH models. Our study cohort had victims of severe head trauma and we applied the Rotterdam CT score, and we evaluated the observed versus predicted mortality at 6 months after the trauma. In our study, we found good performance in the Rotterdam CT score to predict mortality, different studies have been commissioned to validate the Rotterdam performance finding that the CT score the 4 criteria of the RSS (i.e., basal cisterns absent, midline shift, epidural lesions, and intraventricular or subarachnoid hemorrhage) Us in our study we show a good performance score in the cohort of patients with TBI.[151617]
CONCLUSIONS
The Rotterdam CT score predicted mortality at 6 months in patients with severe head trauma in a university hospital in Colombia. The Rotterdam CT score is useful for predicting early death and the prognosis of patients with severe TBI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Reflections on the global burden of disease 2010 estimates. PLoS Med. 2013;10:e1001477.
- [Google Scholar]
- Comportamiento del homicidio en Colombia, 2013. Instituto de Medicina Legal y Ciencias Forenses. Forensis 2013:79-125.
- [Google Scholar]
- Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728-41.
- [Google Scholar]
- Systematic review of prognostic models in traumatic brain injury. BMC Med Inform Decis Mak. 2006;6:38.
- [Google Scholar]
- The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma. 1992;9(Suppl 1):S287-92.
- [Google Scholar]
- Prediction of outcome in traumatic brain injury with computed tomographic characteristics: A comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery. 2005;57:1173-82.
- [Google Scholar]
- Rotterdam computed tomography score as a prognosticator in head-injured patients undergoing decompressive craniectomy. Neurosurgery. 2012;71:80-5.
- [Google Scholar]
- Predicting outcome after traumatic brain injury: Development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008;5:e165.
- [Google Scholar]
- Prediction of outcome after moderate and severe traumatic brain injury: External validation of the International Mission on Prognosis and Analysis of Clinical Trials (IMPACT) and Corticoid Randomisation After Significant Head injury (CRASH) prognostic models. Crit Care Med. 2012;40:1609-17.
- [Google Scholar]
- Validation of the CRASH model in the prediction of 18-month mortality and unfavorable outcome in severe traumatic brain injury requiring decompressive craniectomy. J Neurosurg. 2014;120:1131-7.
- [Google Scholar]
- The Rotterdam scoring system can be used as an independent factor for predicting traumatic brain injury outcomes. World Neurosurg. 2016;87:195-9.
- [Google Scholar]
- A comparative study between Marshall and Rotterdam CT scores in predicting early deaths in patients with traumatic brain injury in a major tertiary care hospital in Nepal. Chin J Traumatol. 2016;19:25-7.
- [Google Scholar]
- Predicting outcomes of decompressive craniectomy: Use of Rotterdam Computed Tomography Classification and Marshall Classification. Br J Neurosurg. 2016;30:258-63.
- [Google Scholar]






