Translate this page into:
Epilepsy care and outcome in low- and middle-income countries: A scoping review
*Corresponding author: Nourou Dine Adeniran Bankole, Department of Research, Association of Future African Neurosurgeons, Yaounde, Cameroon. bankolenouroudine@yahoo.fr
-
Received: ,
Accepted: ,
How to cite this article: Bankole N, Dokponou Y, De Koning R, Dalle D, Kesici O, Egu C, et al. Epilepsy care and outcome in low- and middle-income countries: A scoping review. J Neurosci Rural Pract. 2024;15:8-15. doi: 10.25259/JNRP_527_2023
Abstract
Objectives:
Epilepsy is a common neurological condition in low- and middle-income countries (LMICs). This study aims to systematically review, analyze, evaluate, and synthesize information on the current state of medical and surgical management and outcomes of epilepsy in LMICs.
Materials and Methods:
Systematic searches were conducted on MEDLINE, EMBASE, World Health Organization Global Index Medicus, African Journals Online, WOS, and Scopus, covering the period from the inception of the databases to August 18th, 2021, focusing on studies reporting management and outcomes of epilepsy in LMICs.
Results:
A total of 2298 unique studies were identified, of which, 48 were included (38035 cases). The mean age was 20.1 ± 19.26 years with a male predominance in 60.92% of cases. The type of seizure commonly reported in most of the studies was absence seizures (n = 8302, 21.82%); partial focal seizure (n = 3891, 10.23%); and generalized tonic-clonic seizures (n = 3545, 9.32%) which were the next most common types of seizures. Mesiotemporal epilepsy was less frequently reported (n = 87, 0.22%). Electroencephalogram was commonly used (n = 2516, 6.61%), followed by computed tomography scan (n = 1028, 2.70%), magnetic resonance imaging (n = 638, 1.67%), and video telemetry (n = 484, 1.27%) in the care of patients with seizures. Primary epilepsy was recorded in 582 patients (1.53%) whereas secondary epilepsy was present in 333 patients (0.87%). Carbamazepine was the most used anti-epileptic drug (n = 2121, 5.57%). Surgical treatment was required for 465 (1.22%) patients.
Conclusion:
In LMICs, epilepsy is underreported. There is still a lack of adequate tools for the diagnosis of primary or secondary epilepsy as well as adequate access to medical management of those reported.
Keywords
Epilepsy
Diagnosis
Management
Outcomes
Low- and middle-income countries
INTRODUCTION
Epilepsy affects over 45 million people worldwide and has a significant impact on global population morbidity and mortality.[1] Health inequity is stark when comparing regions by their income status, particularly in terms of healthcare personnel expertise, diagnostic capacity, management options, and cultural perceptions.[2,3] The underlying etiology of epilepsy also varies with asphyxia during birth, central nervous system infections, and traumatic brain injury (TBI) accounting for a larger proportion of epilepsy in low-and-middle-income countries (LMICs).[4] Although from a geographical, sociocultural, and political perspective, LMICs are a heterogeneous group with significant differences in epidemiology, etiology, and perceptions of epilepsy.
The World Health Organization (WHO) reports that nearly 80% of the global population with epilepsy resides in LMICs.[5,6] This represents a considerable global health challenge in providing accessible and adequate epilepsy care that is both affordable and effective. Epilepsy is particularly prevalent in young adults in LMICs.[7,8] Recent reports focusing on one continent suggest that the epilepsy treatment gap across Africa is significantly higher than in other resource-poor settings.[9] It is suggested that <20% of patients with epilepsy across Africa have consulted a healthcare professional for treatment, and inappropriate care is contributing to the high mortality of those inflicted with this condition.[10]
It is important to establish how practices vary for the diagnosis and treatment of epilepsy across the world. Sharing best practices between centers within and between countries could reduce the currently debilitating disease burden imposed by epilepsy in LMICs. Therefore, this study aims to gain an understanding of the current state of the medical and surgical management of epilepsy across LMICs. We aim to capture the variability in diagnostic and treatment methods as well as the barriers to the optimization of these methods to determine the level of variability in epilepsy management across the LMICs.
MATERIALS AND METHODS
Search strategy
The Arksey and O’Malley framework guided this scoping review.[11] The Preferred Reporting Items for Systematic Review and meta-Analysis Extension for Scoping Reviews guidelines were used to report the findings.[12]
Inclusion and exclusion criteria
We included studies that fulfilled specific inclusion criteria discussed in our published protocol. Studies of interest discussed epilepsy in the LMIC population. Only published articles with original data were included in this review. This does not include abstracts or letters. There were no restrictions to the period of the publications considered. Only publications in English and French languages were considered. Studies were excluded if they did not include data on the medical or surgical management of epilepsy in LMICs.
Search strategy
The search protocol for this scoping review was executed on MEDLINE, EMBASE, WHO Global Index Medicus, African Journals Online, WOS, and Scopus covering the period between inceptions of the databases to August 18th, 2021. The search strategy used variants and combinations of search terms related to epilepsy, diagnostic modalities, medical and surgical treatment, and LMICs. The exact content and order of the search string queries is shown in Appendix 1. A hand-search of Google Scholar was also conducted to identify additional articles that were not captured in the above process.
Study selection
All the articles resulting from the search were exported into Rayyan,[13] where duplicates were identified and deleted. Rayyan is professional research software that is widely used by collaborators for ease of study selection decisions. The study selection process consisted of multiple steps. First, two reviewers independently screened the titles and abstracts of the identified articles based on the pre-defined inclusion and exclusion criteria. Any disagreement in the decision between the two reviewers prompted further discussion. If a disagreement persisted, it was resolved by one of the senior authors (NDAB, SB, and YCHD). The full texts of the remaining articles were retrieved and screened by two reviewers independently as per the process above. Pilot screening and a consensus meeting were conducted before each stage.
Data extraction
All participants underwent a training session on data extraction followed by a pilot phase to ensure everyone was extracting data homogeneously. An Excel sheet was utilized for data collection with columns for each data point of specific interest such as study design, patient demographics/characteristics, management modality (medical management and surgical procedure), and outcomes (mortality, morbidity expressed in quality of life, and free seizure) of care, diagnosis means (electroencephalogram [EEG], video EEG, histological, and molecular), neuroimaging (magnetic resonance imaging [MRI], computed tomography [CT] scan, and angiography), regions (LMICs), and resource availability (medical staff, infrastructure, and financial risk protection). Following the pilot stage, the final data extraction sheet was agreed on through a consensus meeting before embarking on the proper data extraction stage.
Data analysis
Extracted data was analyzed by the Statistical Package for the Social Sciences v.26 (IBM, USA). High heterogeneity between the studies meant that neither a simple pooling of results nor weighted averages of the incidence rates would be appropriate. Instead, a narrative synthesis has been conducted. The total number of patients across all studies (and the proportion of the total) was reported for each categorical variable being analyzed. A comparison of findings was done between LMICs as per the World Bank Country and Lending Groups.[14]
RESULTS
We identified 2295 records (96.23%) through the database search and 90 (3.77%) through supplemental hand-search. We excluded 1878 articles (78.77%) at the title and abstract screening, and 370 (15.52%) at full-text screening. Forty-eight articles (2.01%) were eligible for inclusion [Figure 1]. India had the highest number of publications (n = 12/48, 25.05%), and the majority of literature on this topic was published in the 21st century (n = 41/48, 85.4%) [Table 1]. The studies included were mostly retrospective (n = 16, 33.3%) and prospective (n = 14, 29.16%) cohort studies, and the study population consisted of 38,046 cases from 24 LMICs [Table 1]. The young adult (18–40 years) age group was the most affected (n = 22128, 58.17%) with a male predominance (n = 23173, 60.92%).
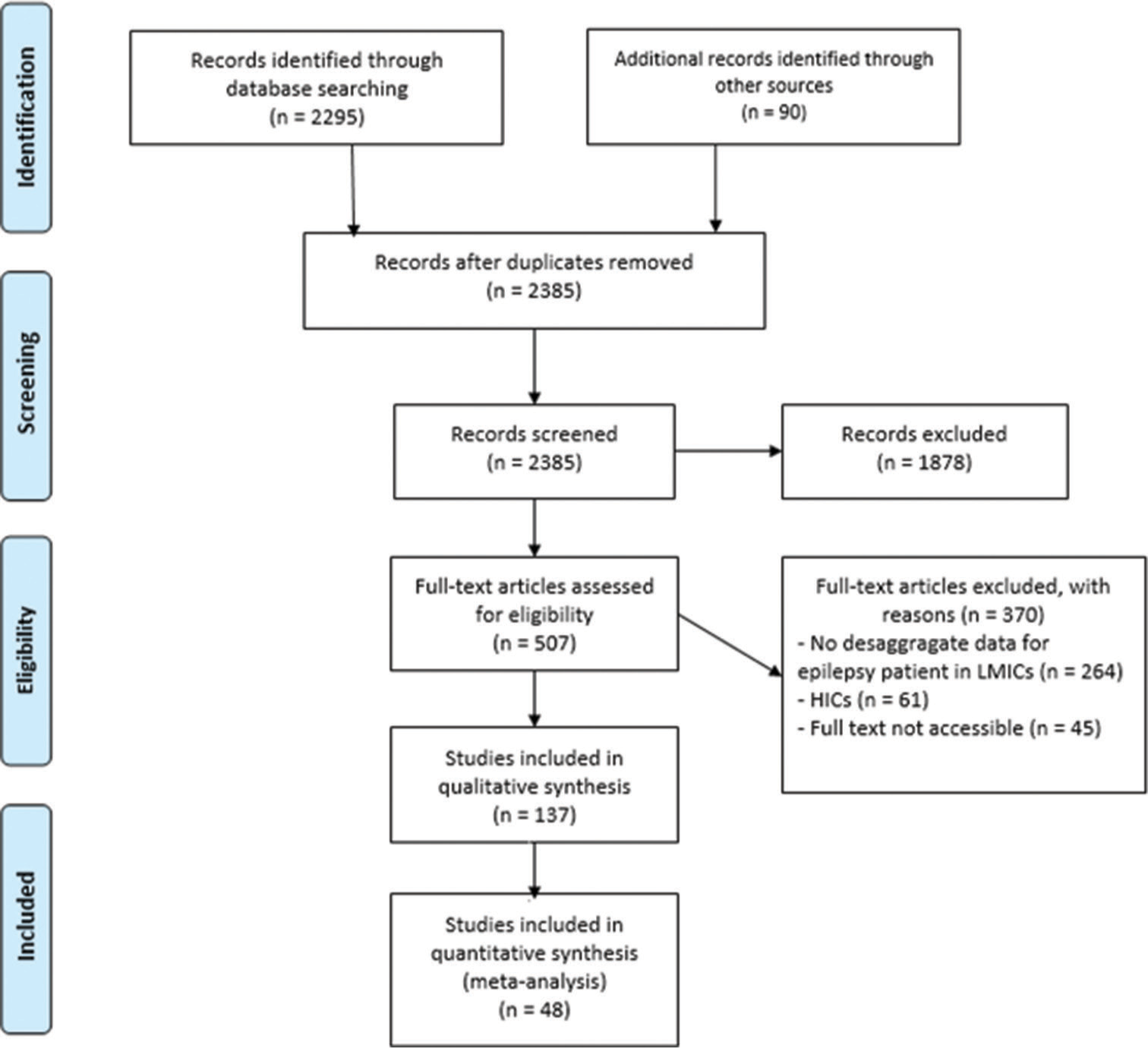
- Epilepsy care and outcome in low- and middle-income countries (LMICs): search strategy using Preferred Reporting Items for Systematic Review and Meta-analysis flowchart. HICs: High-income countries.
| Characteristics | Frequency (percentage) |
|---|---|
| Publication year | |
| 1980–1990 | 2 (4.2) |
| 1991–2001 | 8 (16.7) |
| 2002–2012 | 10 (20.8) |
| 2013–2021 | 28 (58.3) |
| Study setting | |
| India | 12 (25.0) |
| China | 5 (10.4) |
| Mali | 3 (6.2) |
| Nigeria | 2 (4.2) |
| Morocco | 2 (4.2) |
| LAO PDR | 2 (4.2) |
| Colombia | 2 (4.2) |
| Zambia | 2 (4.2) |
| Malaysia | 1 (2.1) |
| Bolivia | 1 (2.1) |
| Lebanon | 1 (2.1) |
| Sri Lanka | 1 (2.1) |
| Tanzania | 1 (2.1) |
| Uganda | 1 (2.1) |
| Kenya | 1 (2.1) |
| South Africa | 1 (2.1) |
| Serbia | 1 (2.1) |
| Lybia | 1 (2.1) |
| Cambodia | 1 (2.1) |
| Pakistan | 1 (2.1) |
| Turkey | 1 (2.1) |
| Haiti | 1 (2.1) |
| Ecuador | 1 (2.1) |
| Zimbabwe | 1 (2.1) |
| Study design | |
| Cross-sectional | 10 (20.8) |
| Case report | 1 (2.1) |
| Case series | 03 (6.2) |
| Retrospective study | 16 (33.3) |
| Prospective study | 14 (29.2) |
| Randomized controlled trial | 03 (6.2) |
| Validation study | 1 (2.1) |
LMICs: Low- and middle-income countries, LAO PDR: Lao People’s Democratic Republic
The type of seizure commonly reported in most of the studies was absence seizures (n = 8302, 21.82%); partial focal seizure (n = 3891, 10.23%): and generalized tonic-clonic seizures (n = 3545, 9.32%) which were the next most common types of seizures. However, specific seizures for epileptic patients were not reported in 21,574 patients (56.7%). The types of seizures identified are listed in Table 2.
| Types of seizure | Frequency (percentage) |
|---|---|
| Absence seizure | 8302 (21.82) |
| Partial focal | 3891 (10.23) |
| Generalized tonic-clonic | 3545 (9.32) |
| Partial secondarily generalized | 647 (1.68) |
| Mesial-temporal epilepsy | 87 (0.22) |
| Not precise | 21574 (56.7) |
| Total | 38046 |
LMICs: Low- and middle-income countries
Primary epilepsy was recorded for 582 patients (1.53%), and secondary epilepsy in 333 patients (0.87%). The precise etiology of secondary epilepsy was reported for 280 patients: TBI (n = 132, 47.1%), an intracranial suppurative collection such as empyema (n = 47, 16.8%), hippocampal sclerosis (n = 44, 15.7%), cavernomas (n = 39, 13.9%), and tumor (n = 18, 6.4%) [Table 3]. Other reported causes are cerebral developmental venous anomalies (11 patients), stroke (six patients), meningitis and cerebral cysts (five patients), cortical dysplasia (57 patients), developmental epilepsy encephalopathy (seven patients), and malaria (eight patients).
| Variables | Frequency (percentage) |
|---|---|
| Diagnosis modalities | |
| EEG | 2516 (6.61) |
| Video EEG | 484 (1.27) |
| CT-scan imaging | 1028 (2.70) |
| MRI imaging | 638 (1.67) |
| Primary epilepsy | 582 (1.53) |
| Secondary epilepsy | 333 (0.87) |
LMICs: Low- and middle-income countries, EEG: Electroencephalogram, MRI: Magnetic resonance imaging, CT: Computed tomography
Of 48 studies (38046 patients) which reported on diagnostic modality, EEGs were mostly used (n = 2516, 6.61%) when neuroimaging was required, a computed tomographic scan was mostly used (n = 1028, 2.70%) [Table 3].
Medical treatment was reported for 6503 patients (17.09%). Monotherapy anti-epileptic drug (AED) was the most used regimen (n = 4546, 11.95%), followed by bi-therapy AED (n = 1385, 3.64%) and tri-therapy (n = 543, 1.43%). The majority of patients with seizures (n = 31.532, 82.90%) were reported not to have been followed up and started on medical treatment [Table 4]. As AED was used, carbamazepine was the most commonly used (n = 2121, 5.57%), followed by phenytoin (n = 837, 2.20%), sodium valproate (n = 753, 1.97%), and diazepam (n = 563, 1.48%) [Table 4]. Only one study among the 48 studies reported 29 patients under clonazepam.
| Variables | Frequency (percentage) |
|---|---|
| Treatment | |
| Medical treatment | 6503 (17.09) |
| Monotherapy AED | 4546 (11.95) |
| Biotherapy AED | 1385 (3.64) |
| Tritherapy AED | 547 (1.43) |
| AED | |
| Carbamazepine | 2121 (5.57) |
| Phenytoin | 837 (2.20) |
| sodium valproate | 753 (1.97) |
| Lamotrigine | 235 (0.61) |
| Diazepam | 563 (1.48) |
| Phenobarbitone | 232 (0.60) |
| Levetiracetam | 129 (0.33) |
| Ethosuximide | 104 (0.27) |
| Surgical treatment | 465 (1.22) |
| Outcomes | |
| Symptoms resolved | 1783 (4.68) |
| Symptoms reduced | 823 (2.16) |
| Symptoms unchanged | 371 (0.97) |
| Symptoms worsened | 698 (1.83) |
| Died | 467 (1.22) |
| Survived | 2124 (5.58) |
LMICs: Low- and middle-income countries, AED: Antiepileptic drugs
Surgical treatment was required for 465 (1.22%) patients, among them 51 patients (11%) underwent temporal lobectomy while, for others (414 patients), the type of surgery was not precise.
Of the 48 studies (38046 patients), which reported on the outcome of interest, the symptoms resolved in 1783 patients (4.68%) [Table 4]. There was a reduction of symptoms in 823 patients (2.16%), no change in 371 patients (0.97%), and exacerbation in 698 patients (1.83%) [Table 4].
Among the 48 studies (38046 patients), which reported long-term follow-up, the mean length of follow-up was 21.91 (95% confidence interval [CI]: 13.4 [8.76, 35.05]) months and 2124 patients (5.58%) survived after being discharged [Table 4].
DISCUSSION
This review identified and analyzed data from 48 studies (38,046 cases) on epilepsy across 25 LMICs. India was the country that reported the most studies regarding the management and the outcomes (25%) of epilepsy. The most common type of seizures were absence seizures (n = 8302, 21.82%). Mesiotemporal epilepsy was reported in a minority of participants (n = 87, 0.22%). Primary epilepsy was identified in 582 patients (1.53%), whereas secondary epilepsy was diagnosed in 333 patients (0.87%). TBI (n = 132, 47.1%), intracranial suppurative collection (n = 47, 16.8%), hippocampal sclerosis (n = 44, 15.7%), cavernomas (n = 39, 13.9%), and tumor (n = 18, 6.4%) were identified as other presentations discussing then etiology for epilepsy. Carbamazepine was the most commonly used (n = 2121, 5.57%) as AED. Surgery of epilepsy was reported only on 465 patients (1.22%). Epilepsy resolved in 4.68%, reduced in 2.16%, unchanged in 0.97%, and unfortunately worsened in 1.83%. The mean length follow-up of was 21.91 months (95% CI: 8.76, 35.05) for only 241 patients (0.63%).
Most of the studies on epilepsy were conducted in Asia, which reflects the greater disease burden in this continent.[15] However, Africa as a continent is thoroughly underrepresented in research done to establish diagnostic and treatment modalities available for patients. This may be because many epileptic citizens in Africa sought help from traditional healers rather than healthcare professionals. More recent studies confirm that a similar stigma persists – particularly within rural settings.[16,17] Recently, authors reported that epilepsy could reveal cavernomas in 47% of cases in their series.[18] At present, many epilepsy clinics across Africa are managed by non-physician healthcare personnel, and good seizure control is reported in only two-thirds of treated patients.[19] Financial constraint is an important consideration, and rural epilepsy clinics are commonly funded by external donor agencies.[19] These factors represent a crucial barrier to adequate investigation and treatment of epilepsy across Africa.[4]
Our study highlighted that epilepsy diagnosis in LMICs is complex, and many centers rely on a few modalities. The patient’s history and neurologic examination remain the cornerstones of the diagnosis of epilepsy in LMICs whereas EEGs and neuroimaging seemingly serve as adjunctive tests. Although this is appropriate in most cases,[20] it can lead to under-treatment of those with absence seizures and prevent pre-operative planning for patients for whom surgical management could be curative.
Epilepsy surgery has repeatedly shown itself to be both cheaper than medical management and to result in a better quality of life for patients, who have a surgical cause for their epilepsy.[21-23] This is especially true for patients with medically resistant seizures; defined as failure of enough trials of two tolerated, well-selected AEDs. Many patients in LMICs pay for their AEDs out-of-pocket -with only partial coverage from the public sector.[24] Surgery may be a more viable solution for their long-term finances. These surgical procedures can be divided into three primary categories: Ablative procedures, therapeutic devices, and surgical resection or disconnection.[25] Nevertheless, despite the benefits of these treatments, they are underutilized in LMICs where 80% of emerging centers lack epilepsy surgery centers.[26] Although there is a current deficit in the number of surgeons in LMICs able to provide epilepsy surgery,[27] medical management should not be the sole treatment offered, especially when AEDs in LMICs are in limited supply and can be of poor quality.[28,29] In a study evaluating AED affordability in India, data suggested a whole month’s stock of AEDs required over a month’s wages for the lowest paid daily wages worker.[30] Similarly, an analysis of 46 countries showed generic carbamazepine to cost the lowest-paid government workers 2.7 and 5.2 days’ wages in public and private sectors, respectively, compared to 10.3 and 16.2 days’ wages for originator brands.[31] Physician consultation fees, transport, and additional healthcare costs are not factored into this pricing making treatment less affordable.[31]
However, AEDs are likely to remain the first-line treatment for most epilepsy patients, especially those without a surgical cause. It is established that inadequate and unreliable AED supplies represent a key challenge to the management of epilepsy across LMICs.[32] However, our study showed that sizable numbers of patients in LMICs were being started on a single AED or multiple AEDs. Free drug supply schemes such as that seen in Rajasthan, India can prove helpful in optimizing the number of patients who can access adequate and affordable treatment for their epilepsy.[33]
The WHO recently released evidence-based, epilepsy-care guidelines[34,35] appropriate for use in LMICs notably advocating using phenobarbital as a first-line drug in resource-poor settings due to its affordability, cost-effectiveness, and once-daily dosing regime.[36] In contrast, high-income regions commonly use alternative AEDs as first-line treatment. Guidelines developed in high-income countries are likely inappropriate for use in LMICs.[37] In general, the transferability of evidence derived from studies conducted in high-income countries to LMICs is difficult.[37-39] Differences in patient populations and healthcare systems are so prominent that the evidence may not be valid; hence, the development of guidelines specifically crafted for resource-limited settings is the best strategy.[36,39] With newer AEDs increasingly being used in LMICs, it is important to summarize the important characteristics of these drugs and their interaction with other classes of medication[40-43] to produce adequate guidelines for effective usage.
This scoping review identified the management regarding the diagnosis, the treatment, and the outcomes of epilepsy in LMICs. However, the published data is available from 25 countries in LMICs. Therefore, our results are unlikely to reflect the situation across the LMICs. Furthermore, the type of epilepsy was not reported in 56.7% of the patients, and fewer studies reported the management with long-term follow-up. The surgical management was not precise about the details; only one study was precise about the type of the procedure. Moreover, we were only able to include articles published in English or French. This means literature published in alternative languages such as Spanish and Arabic, which will have been omitted from our analysis. However, this scoping review gives a real overview of the management nowadays about epilepsy such as the clinical electrophysiology, imaging, AED, and surgical treatment for epilepsy. Nonetheless, studies need to be done in the future from the locoregional centers around the LMICs for reaching out to management protocol toward quick adequate management and long-term follow-up with access to quality of life for epilepsy patients. This will be relevant and helpful to improve the care of epilepsy in LMICs. Furthermore, given the high heterogeneity of the included studies, studies were unable to be pooled in a meta-analysis to generate true pooled statistics for all the data points mentioned above.
CONCLUSION
Epilepsy diseases represent a burden in LMICs. The young adult was more represented. The most common type of epilepsy was the absence type of epilepsy while mesiotemporal epilepsy was less reported. An EEG, CT scan, MRI, and Video EEG were used for the clinical electrophysiology and imaging correlation for the diagnosis. Primary epilepsy was retained more than secondary epilepsy. The TBI, intracranial suppurative collection, hippocampal sclerosis, cavernomas, and tumors were the common causes of epilepsy. Other causes such as cerebral developmental venous anomalies, stroke, meningitis, cortical dysplasia, developmental epilepsy, encephalopathy, and malaria were very less reported. Carbamazepine was the most commonly used AED. Surgery of epilepsy was less reported. Fewer studies reported on the outcomes of epilepsy.
Acknowledgments
We would like to address special thanks and gratitude to the Neurology and Neurosurgery Interest Group (NANSIG) in collaboration with the Association of Future African Neurosurgeons (AFAN), who made this research project possible. We would like to acknowledge also Dr Upamanyu Nath, and Dr Paix de Dieu Ngo for their contribution on the screening steps.
Authors’ contributions
Nourou Dine Adeniran Bankole: Conceptualization, project administration, methodology, data screening, data extraction, supervision, writing, review, and editing. Dokponou Yao Christian Hugues: Methodology, data curation, data analysis, validation, writing, review, and editing. Rosaline de Koning: Methodology, data extraction, writing, review, and editing. David Ulrich Dalle: Methodology, data screening, data extraction, writing, and reviewing. Setthasorn Zhi Yang Ooi: Data screening, data extraction, and writing. Emmanuel Mukambo: Data extraction, writing, review, and editing. Chinedu Egu: Data extraction and writing. Özgür Kesici: Data extraction and writing. Olaoluwa Ezekiel Dada: Data screening, data extraction, reviewing, and editing. Berjo Dongmo Takoutsing: Data screening, reviewing, and editing. Gideon Adegboyega: Data screening, data extraction, writing, review, and editing. Chibuikem Anthony Ikwuegbuenyie: Data screening, data extraction, and writing. Soham Bandyopadhyay: Data screening, data extraction, writing, review and editing, and supervision.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Appendix 1 and PRISMA guidelines available on:
Financial support and sponsorship
Nil.
References
- Global, regional, and national burden of epilepsy, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:357-75.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges in the management of epilepsy in resource-poor countries. Nat Rev Neurol. 2009;5:323-30.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy care challenges in developing countries. Curr Opin Neurol. 2012;25:179-86.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology, causes, and treatment of epilepsy in sub-Saharan Africa. Lancet Neurol. 2014;13:1029-44.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy. Available from: https://www.who.int/news-room/fact-sheets/detail/epilepsy [Last accessed on 2023 Oct 28]
- [Google Scholar]
- Estimation of the burden of active and life-time epilepsy: A meta-analytic approach. Epilepsia. 2010;51:883-90.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of active epilepsy, lifetime epilepsy prevalence, and burden of epilepsy in Sub-Saharan Africa from meta-analysis of door-to-door population-based surveys. Epilepsy Behav. 2020;103:106846.
- [CrossRef] [PubMed] [Google Scholar]
- An estimate of the prevalence of epilepsy in Sub-Saharan Africa: A systematic analysis. J Glob Health. 2012;2:20405.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy treatment gap in Sub-Saharan Africa: Meta-analysis of community-based studies. Acta Neurol Scand. 2020;142:3-13.
- [CrossRef] [PubMed] [Google Scholar]
- Gaze deviation from contralateral pseudoperiodic lateralized epileptiform discharges (PLEDs) Epilepsia. 2005;46:977-9.
- [CrossRef] [Google Scholar]
- Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8:19-32.
- [CrossRef] [Google Scholar]
- PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467-73.
- [CrossRef] [PubMed] [Google Scholar]
- Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
- [CrossRef] [PubMed] [Google Scholar]
- A model for managing epilepsy in a rural community in Africa. Br Med J. 1989;298:805-7.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy-associated stigma in subSaharan Africa: The social landscape of a disease. Epilepsy Behav. 2005;7:68-73.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial cavernomas management and outcomes: A cross-sectional study from 20 years of experience at Speciality Hospital, Rabat, Morocco. PAMJ Clin Med. 2022;9:10.
- [CrossRef] [Google Scholar]
- Epilepsy surgery in low-and middle-income countries: A scoping review. Epilepsy Behav. 2019;92:311-26.
- [CrossRef] [PubMed] [Google Scholar]
- Seizures and epilepsy: An overview for neuroscientists. Cold Spring Harb Perspect Med. 2015;5:a022426.
- [CrossRef] [PubMed] [Google Scholar]
- Dollars and sense: Cost-effectiveness of epilepsy surgery. Epilepsy Curr. 2021;21:171-2.
- [CrossRef] [PubMed] [Google Scholar]
- Cost-effectiveness analysis of epilepsy surgery in a controlled cohort of adult patients with intractable partial epilepsy: A 5-year follow-up study. Epilepsia. 2016;57:1669-79.
- [CrossRef] [PubMed] [Google Scholar]
- Cost-effectiveness of surgery for drug-resistant temporal lobe epilepsy in the US. Neurology. 2020;95:e1404-16.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment gaps and challenges in epilepsy care in the Philippines. Epilepsy Behav. 2021;115:107491.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy surgery: Challenges for developing countries. Lancet Neurol. 2009;8:420-1.
- [CrossRef] [PubMed] [Google Scholar]
- Surgery for epilepsy: The need for global acceptance and access. Lancet Neurol. 2016;15:898-9.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of antiepileptic drugs in sub-Saharan Africa: A study in Gabon, Kenya, and Madagascar. Epilepsia. 2018;59:1351-61.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy in Africa: Can we end suffering and financial hardship due to lack of access to effective and affordable care? EClinicalMedicine. 2019;9:9-10.
- [CrossRef] [PubMed] [Google Scholar]
- Antiepileptic drug prices, availability and affordability in a resource-limited setting. Ann Indian Acad Neurol. 2020;23:674-80.
- [CrossRef] [PubMed] [Google Scholar]
- Mapping the availability, price, and affordability of antiepileptic drugs in 46 countries. Epilepsia. 2012;53:962-9.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy treatment in sub-Saharan Africa: Closing the gap. Afr Health Sci. 2012;12:186-92.
- [CrossRef] [PubMed] [Google Scholar]
- WHO and ILO call for new measures to tackle mental health issues at work Geneva, Switzerland: WHO; 2022.
- [Google Scholar]
- mhGAP: Mental health gap action programme: Scaling up care for mental, neurological and substance use disorders Geneva: World Health Organization; 2008.
- [Google Scholar]
- Phenobarbital: Missing in action. Bull World Health Organ. 2012;90:871a.
- [CrossRef] [PubMed] [Google Scholar]
- Transfer of evidence-based medical guidelines to low-and middle-income countries. Trop Med Int Health. 2012;17:144-6.
- [CrossRef] [PubMed] [Google Scholar]
- Is evidence-based medicine relevant to the developing world? PLoS Med. 2005;2:e107.
- [CrossRef] [PubMed] [Google Scholar]
- Improving the use of research evidence in guideline development: 13. Applicability, transferability and adaptation. Health Res Policy Syst. 2006;4:25.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364:2483-95.
- [CrossRef] [PubMed] [Google Scholar]
- Medical management of epileptic seizures: Challenges and solutions. Neuropsychiatr Dis Treat. 2016;12:467-85.
- [CrossRef] [PubMed] [Google Scholar]
- Epilepsy care cascade, treatment gap and its determinants in rural South Africa. Seizure. 2020;80:175-80.
- [CrossRef] [PubMed] [Google Scholar]
- Health service provision for people with epilepsy in sub-Saharan Africa: A situational review. Epilepsy Behav. 2017;70:24-32.
- [CrossRef] [PubMed] [Google Scholar]







