Translate this page into:
Effects of Crystalloid Preloading (20 ml/kg) on Hemodynamics in Relation to Postural Changes in Patients Undergoing Neurosurgical Procedures in Sitting Position
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Hemodynamic disturbances are common during positioning the patients from supine to sitting for neurosurgical procedures. The reported incidence of hypotension varies from 5% to 32%. The aim of the study was to study the effect of crystalloid preloading on hemodynamic parameters during positioning the patient from supine to sitting position.
Materials and Methods:
In this prospective observational trial, 20 patients were enrolled. Two patients had a patent foramen ovale on transesophageal echocardiography and were excluded from the study. All the patients received 20 ml/kg of crystalloid (Ringer's lactate) before initiation of positioning. Physiological hemodynamic parameters such as heart rate, mean arterial pressure, central venous pressure, cardiac output (CO), stroke volume variation (SVV), cardiac index (CI), stroke volume (SV), and maximum and minimum inferior vena caval diameter (IVCD) were recorded after induction, during positioning at 30°, 60° inclination of the operating table and after the final sitting position.
Results:
Hemodynamic parameters were well maintained during positioning of the patients from supine to sitting position. Crystalloid preloading prevented the hypotension during positioning. There were no significant changes in hemodynamic parameters such as CO, SVR, SVV, CI, and SV. We did not find any correlation with changes in IVCD with changes in CO.
Conclusion:
A volume of 20 ml/kg of crystalloid preloading before positioning the patient from supine to sitting position maintains the hemodynamic stability and avoids the vasopressor requirement.
Keywords
Crystalloid preloading
inferior vena caval diameter
mean arterial pressure
patent foramen ovale
sitting craniotomy
INTRODUCTION
Sitting position for posterior fossa and cervical spine surgeries pose challenges to anesthesiologists in terms of hemodynamic instability. Sitting position for neurosurgery has both pros and cons, and there has been a constant debate since its introduction by De Martel.[1] The benefits of sitting position to the surgeons include optimum access to posterior midline lesions, improved access to tentorial hiatus, improved visibility, clear surgical field due to gravity assisted drainage of the blood.[2] Whereas for anesthesiologists, it offers greater access to the endotracheal tube, intravenous (IV) lines, lower airway pressure, decreased the need for blood transfusion, and clear view to observe the cranial nerve response. However, sitting position has several disadvantages such as hemodynamic disturbances, venous air embolism (VAE), paradoxical air embolism, pneumocephalus, and postoperative quadriplegia and quadriparesis.[3]
Hemodynamic disturbances like hypotension are very common in neurosurgical procedures in sitting position. The reported incidence of hypotension in the literature varies from 5% to 32%.[4567] The resulting hypotension may cause cerebral and myocardial ischemia. The gravitational effect can sequester as much as 1500 ml of blood in the lower limbs in sitting position, thus reducing preload to the heart. The vasodilator properties of inhaled anesthetic agents and depression of myocardial contractility can further aggravate hypotension in sitting position craniotomy. Besides, the positive pressure ventilation can reduce the venous return further contributing to the hypotension. Moreover, the patient-related factors such as body mass index (BMI) and intravascular volume status can influence the hemodynamic status during sitting position craniotomy.
Several studies[8910] have shown a decrease in mean arterial pressure (MAP), stroke volume index (SVI), and cardiac index (CI) in patients undergoing neurosurgical procedures in sitting position. None of the studies have prospectively studied the effects of crystalloid preloading on hemodynamic changes during positioning from supine to sitting position. Hence, this pilot study was designed to study the effect of crystalloid preloading on hemodynamic parameters such as MAP, SV, cardiac output (CO), CI, and inferior vena cava diameter (IVCD) during positioning the patient from supine to sitting position.
MATERIALS AND METHODS
It is a prospective observational study conducted in the tertiary care center, after obtaining institutional ethical approval. The study was registered with clinical trial registry India (CTRI number-CTRI/2014/11/005221). Written informed consent was taken from 20 patients, aged between 18 and 60 years with the American Society of Anesthesiologist (ASA) physical Status I and II. Patients with severe cardiac and renal disease, orthodeoxia, patent foramen ovale (PFO), and intracardiac shunts were excluded from the study. Patient data such as age, sex, weight, height, BMI, ASA physical status were collected during the preoperative visit, a day before surgery. Baseline investigations such as complete hemogram, blood urea, serum creatinine, random blood sugar, electrocardiogram, and chest X-ray were noted.
Preoperatively, all the patients posted for craniotomy in sitting position were assessed for any cardiac defects (PFO and other intracardiac shunts) by transthoracic echocardiography (TTE).
Inside the operation theater, standard monitors, i.e., electrocardiograph, noninvasive blood pressure, pulse oximeter (SpO2) were attached. An 18-G IV cannula was secured, patients were anesthetized with standard induction protocol with fentanyl 2 μg/kg IV, propofol 1.5 mg/kg IV, and vecuronium 0.1 mg/kg IV and patients were intubated with the appropriate size endotracheal tube.
A volume of 20 ml/kg of normal saline was loaded until we began to position the patient. Following induction, the arterial line was secured using a 20G cannula in the radial artery and was connected to two BP transducer sets. One pressure transducer set was zeroed at the mastoid process to monitor Systolic BP, Diastolic BP and MAP. The second transducer was connected to FloTrac (Edward Lifesciences, LLC, Irvine, CA) sensor on Vigileo CO device (model no-MHM1E) for continuous monitoring of CO, CI, SV, SVI, and SV variation (SVV). A transesophageal echocardiography (TEE) probe was inserted (Esaote SpA) to rule out PFO by Color Doppler. A right subclavian vein was cannulated using a 7 Fr triple lumen central venous catheter. The tip of the catheter was placed at Superior vena cava (SVC) and right atrial junction using TEE and the presence of PFO was ruled out again with agitated saline technique. In patients in whom PFO was detected, the plan for sitting position was abandoned and surgery was continued in lateral or prone position.
The anesthesia was maintained with oxygen and air mixture (FiO2 of 40%), with 0.8–1 MAC of isoflurane titrated to entropy value of 40–60. An intermittent bolus of fentanyl and vecuronium were supplemented as and when required.
After the IV infusion of 20 ml/kg of saline, just before positioning, all the baseline parameters such as heart rate (HR), MAP, central venous pressure (CVP), CO, SVV, CI, and SV were noted. Maximum and minimum IVCD was noted 1 cm proximal to the IVC-portal vein junction using M-mode in TEE. These parameters were recorded again during positioning at 30°, 60° inclination of the operating table and after the final sitting position. Initially, a slight Trendelenburg position was given. Then, the head end of the table was given propped up position 20°–30°. by alternating Trendelenburg and propped up position, a standard 80°–90° sitting position was obtained after giving 10 min for stabilization with each degree of the position change.
Any fall in mean BP of >10% was considered as hypotension and was treated with intermittent boluses of 20 μg phenylephrine.
Statistical analysis
In this study, both descriptive and inferential statistical analysis was applied. Results on continuous measurements such as age, weight, height, and BMI are presented as Mean +/- SD. Student's t-test has been used to find the significance of study parameters on a continuous scale in each group. Pearson correlation has been used between study variables to find the degree of relationship. The linear relationship between the difference in parameters and difference in CO was carried output using correlation analysis. The normality of the data is tested by Kolmogorov Smirnov test. The Statistical software, namely, SAS 9.2, SPSS 15.0, were used for the analysis of the data. P < 0.05 is considered as statistically significant.
RESULTS
Twenty ASA I and II patients aged between 18 and 60 years were enrolled for the study. Eighteen patients were included in the final analysis. Two patients were excluded from the study after detection of PFO using TEE following induction of anesthesia. Twelve female and eight male patients were enrolled for the study [Table 1]. The mean age and body weight of the participants was 40.5 ± 6.9 years and 60.9 ± 7.3 kg, respectively.

Vitals parameters during positioning of the patient
HR, MAP, and CVP were recorded at supine, 30°, 60°, final sitting position and 30 min after sitting position. There were no significant changes in the HR during positioning [Table 2].
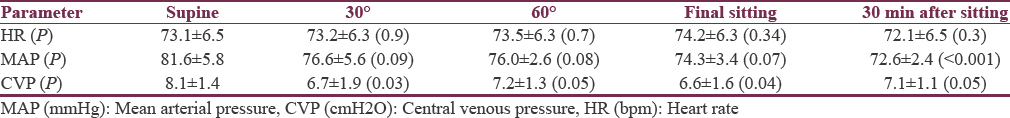
The MAP showed a declining trend, but the changes were not significant (P > 0.05). When compared to the supine position MAP decreased by 6% in 30°, 7% in 60°, 8.4% in final sitting position. None of the patients required vasopressor boluses during positioning. Thirty minutes after final positioning the MAP decreased by around 11%. A significant fall in CVP was observed at 30°, 60°, final sitting position as compared to the supine position [Table 2].
Advanced hemodynamic parameters
The advanced hemodynamic parameters such as SV, SVV, SVI, CO, CI, SVR, and SVR Index (SVRI) were noted during positioning using FloTrac Vigileo sensor [Table 3].
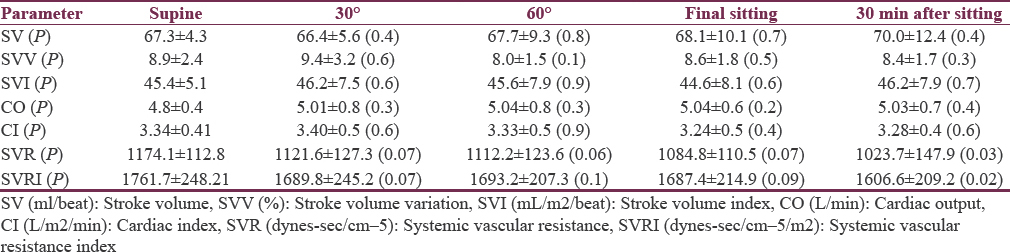
No significant changes in SV, SVV, CO, and CI were observed during positioning the patient from supine to final sitting position. The systemic vascular resistance and SVRI showed a declining trend with a significant reduction after 30 min of final position as compared to sitting position (P = 0.03 and 0.02, respectively).
Inferior vena cava diameter as a marker of preload and correlation with cardiac output
IVCD was measured as a marker of preload in patients during positioning. IVCD was measured during end inspiration and end expiration using M mode in TEE [Table 4]. IVC distensibility index was calculated using the parameters. There was no significant difference in IVCD and distensibility index during positioning the patient from supine to sitting position.
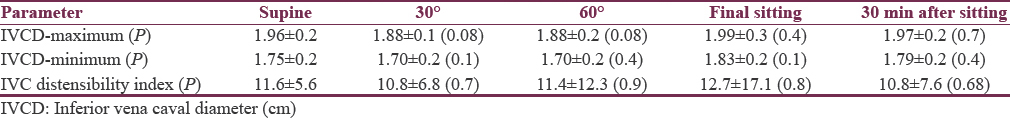
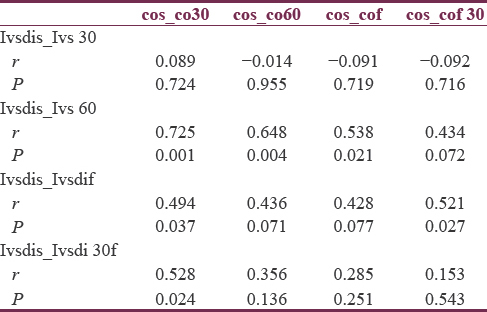
The linear relationship between the differences in IVC distensibility at different time points from baseline with the difference in CO is given in Table 5. It shows that the difference in IVC distensibility index is not correlating with the difference in CO, which indicates the change in CO, is not linearly related to the change in IVC distensibility.
DISCUSSION
Although neurosurgical procedures in sitting position have been diminishing since decades, it is still practiced in some centers as the advantages outweigh its disadvantages in certain cases.[1112] The aim of this study was to assess the hemodynamic changes during positioning, and correlation of the changes in IVCD in relation to the changes in CO.
One of the major complications during positioning is hypotension.[48] Hypotension while positioning can be carefully avoided by optimal preloading of fluids and slow verticalization of the body with pauses to elevate the legs alternatively to minimize the drastic pooling of blood in the lower extremities.
Hypotension, a fall in MAP of >10 mmHg was defined in the study conducted by Young et al. in 255 patients to compare the surgical and anesthetic complications in neurosurgical patients experiencing VAE in the sitting position.[6] In this study, we considered the cutoff value of 10% decrease in MAP as significant. MAP showed a falling trend while positioning from supine to sitting position but the fall in MAP was insignificant until this point. This can be attributed to the preloading of crystalloids before positioning. Fall in MAP by 11.5% after 30 min of final sitting position may be due to mannitol infusion that was given for brain relaxation.
In a study conducted by Marshall et al., they studied the hemodynamic effects of the seated position using four different commonly used anesthetic regimens (enflurane-nitrous oxide, halothane-nitrous oxide, fentanyl-droperidol-nitrous oxide, and morphine-nitrous oxide). In all the four groups observed, CI and SVI reduced significantly in the sitting position compared to supine position. In our study, although some reductions were observed in the SV, SVI, and CO while positioning the patient from supine to sitting position, the changes observed were not significant. Hemodynamic stability in our study may be due to 20 ml/kg of crystalloid preloading before positioning. The preloading of crystalloids and maintenance of adequate anesthetic depth may be responsible for significant fall in SVR and SVRI 30 min after final sitting position. Anesthetic depth was monitored using Entropy and maintained using 0.8–1 MAC of isoflurane titrated to entropy value of 40–60. Besides, intermittent boluses of fentanyl and vecuronium were given given while positioning the patient.
Respiratory variation in IVCD and IVC distensibility index are considered to better predict fluid responsiveness better in patients on mechanical ventilation.[13] In our study, IVCD measured in end inspiration, and end expiration are used as a marker of preload in patients during positioning. IVC distensibility index (maximum D-minimum diameter)/minimum diameter was calculated using the parameters. In a study conducted by Panebianco et al., they found no significant difference in the IVCD in relation to supine or semi-upright position.[14] In this study, we found no significant difference in IVCD and distensibility index during positioning the patient from supine to sitting position. In this study, difference in IVC distensibility index is not correlating with the difference in CO. This may be due to two reasons, careful positioning with the legs at the level of heart and adequate preloading before positioning the patient.
CVP being a poor predictor for fluid responsiveness, it is difficult to decide clinical management based on CVP.[15] In our study, when compared to the supine position CVP decreased by 17% at 30°, 11% at 60°, 12% at a final sitting, and 11% at 30 min after final sitting position. The fall in CVP continuously as the patient is moved from a supine to sitting position may be due to fall in SVR in sitting position. Although there is a decrease in CVP from supine to sitting position, no intervention has been done based on CVP due to other stable hemodynamic parameters.
The risk of VAE and paradoxical air embolism are frequently associated with sitting craniotomy surgeries.[16171819] The presence of PFO increases the risk of paradoxical air embolism.[202122] Many surgeons consider the presence of a PFO as an absolute contraindication to neurosurgery in the sitting position.[2324] The incidence of detection of VAE varies depending upon the technique used. Transesophageal echocardiography and transthoracic Doppler echocardiography are sensitive techniques to detect as small as 0.02 ml/kg and 0.06 ml/kg, respectively.[2526] In our study, TTE and transesophageal echocardiography are used to rule out PFO in the pre- and intra-operative period, respectively. Two patients were detected to have PFO when TEE was used. The Incidence of VAE reported in several studies range from 1% to 76% in sitting craniotomy surgeries.[27] The incidence of VAE detected in our study is 11% which is in the range from other studies.
CONCLUSION
A volume of 20 ml/Kg of crystalloid preloading before positioning the patient from supine to sitting position maintains the hemodynamic stability and avoids the vasopressor requirement.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Surgical treatment of cerebellar tumors: Technical considerations. Surg Gynecol Obstet. 1930;52:381-5.
- [Google Scholar]
- Tumor surgery. In: Cucchiara RF, Michenfelder JD, eds. Clinical Neuroanesthesia. New York: Churchill Livingstone; 1990. p. :285-308.
- [Google Scholar]
- The sitting position in neurosurgery: A retrospective analysis of 488 cases. Neurosurgery. 1984;14:649-58.
- [Google Scholar]
- Anesthesia and surgery in the seated position: Analysis of 554 cases. Neurosurgery. 1985;17:695-702.
- [Google Scholar]
- Outcome following posterior fossa craniectomy in patients in the sitting or horizontal positions. Anesthesiology. 1988;69:49-56.
- [Google Scholar]
- Comparison of surgical and anesthetic complications in neurosurgical patients experiencing venous air embolism in the sitting position. Neurosurgery. 1986;18:157-61.
- [Google Scholar]
- Venous air embolism during radical retropubic prostatectomy. Anesth Analg. 1992;74:151-3.
- [Google Scholar]
- Anesthetic management of posterior fossa surgery in the sitting position. Acta Anaesthesiol Scand. 1976;20:117-28.
- [Google Scholar]
- Cardiovascular responses in the seated position – Impact of four anesthetic techniques. Anesth Analg. 1983;62:648-53.
- [Google Scholar]
- Posterior fossa surgery in the sitting position in a pregnant patient with cerebellopontine angle meningioma. Br J Anaesth. 1999;82:941-4.
- [Google Scholar]
- Emergency posterior fossa surgery in sitting position in a patient with pheochromocytoma. J Neurosurg Anesthesiol. 2016;28:83.
- [Google Scholar]
- Ultrasonographic measurement of the respiratory variation in the inferior vena cava diameter is predictive of fluid responsiveness in critically ill patients: Systematic review and meta-analysis. Ultrasound Med Biol. 2014;40:845-53.
- [Google Scholar]
- The effect of supine versus upright patient positioning on inferior vena cava metrics. Am J Emerg Med. 2014;32:1326-9.
- [Google Scholar]
- Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008;134:172-8.
- [Google Scholar]
- Incidences of venous air embolism and patent foramen ovale among patients undergoing selective peripheral denervation in the sitting position. Neurosurgery. 2003;53:316-9.
- [Google Scholar]
- Incidence of venous and paradoxical air embolism in neurosurgical patients in the sitting position: Detection by transesophageal echocardiography. Acta Anaesthesiol Scand. 1998;42:643-7.
- [Google Scholar]
- The sitting position in neurosurgery: A critical appraisal. Br J Anaesth. 1999;82:117-28.
- [Google Scholar]
- Paradoxical air embolism from patent foramen ovale in scoliosis surgery. Spine (Phila Pa 1976). 2002;27:E291-5.
- [Google Scholar]
- Neurologic manifestations of cerebral air embolism as a complication of central venous catheterization. Crit Care Med. 2000;28:1621-5.
- [Google Scholar]
- Anaesthesia for neurosurgery in the sitting position: A practical approach. Anaesth Intensive Care. 2005;33:323-31.
- [Google Scholar]
- Use of the sitting position in neurosurgery. Results of a 1998 survey in Germany. Anaesthesist. 2000;49:269-74.
- [Google Scholar]
- Anaesthesia for neurosurgery in the sitting position. J Clin Neurosci. 2004;11:693-6.
- [Google Scholar]
- Doppler sensory placement during neurosurgical procedures for children in prone position. J Neurosurg Anesthesiol. 1994;6:153-5.
- [Google Scholar]
- Epidural air injection associated with air embolism detected by transesophageal echocardiography. Reg Anesth. 1995;20:152-5.
- [Google Scholar]
- Patent foramen ovale and neurosurgery in sitting position: A systematic review. Br J Anaesth. 2009;102:588-96.
- [Google Scholar]






