Translate this page into:
Effectiveness of 6D couch with daily cone beam computed tomography in reducing PTV margins for glioblastoma multiforme
*Corresponding author: Deep Shankar Pruthi, Department of Radiation Oncology, Action Cancer Hospital, New Delhi, India. dsp008@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pruthi DS, Nagpal P, Pandey M. Effectiveness of 6D couch with daily cone beam computed tomography in reducing PTV margins for glioblastoma multiforme. J Neurosci Rural Pract 2023;14:78-83.
Abstract
Objectives:
Image-guided radiotherapy maximizes therapeutic index of brain irradiation by reducing setup errors during treatment. The aim of study was to analyze setup errors in the radiation treatment of glioblastoma multiforme and if decrease in planning target volume (PTV), margin is feasible using daily cone beam CT (CBCT) and 6D couch correction.
Materials and Methods:
Twenty-one patients (630 fractions of radiotherapy) were studied in which corrections were made in 6° of freedom. We determined setup errors, impact of setup errors of initial three fractions CBCT versus rest of the treatment with daily CBCT, and mean difference in setup errors with or without application of 6D couch and volumetric benefit of reduction of PTV margin from 0.5 cm to 0.3 cm.
Results:
The mean shift in the conventional directions, namely, vertical, longitudinal, and lateral was 0.17 cm, 0.19 cm, and 0.11 cm. There was significant change in vertical shift when first three fractions were compared with rest of the treatment with daily CBCT. When the effect of 6D couch was nullified, all directions showed increased error with longitudinal shift being significant. The number of setup errors of magnitude >0.3 cm was more significant when only conventional shifts were applied as compared with 6D couch. There was significant decrease in volume of brain parenchyma irradiated when margin of PTV was reduced from 0.5 cm to 0.3 cm.
Conclusion:
Daily CBCT along with 6D couch correction can reduce setup error which allows reduction in PTV margin during radiotherapy planning in turn improving the therapeutic index.
Keywords
Image-guided radiotherapy
Cone beam CT
6D Couch
Planning target volume
Glioblastoma
INTRODUCTION
Gliomas are the most common brain tumor in adults.[1] Glioblastoma multiforme (GBM) (Grade IV) is associated with the worst overall prognosis among all the grades of gliomas. The standard universal treatment of GBM is complete or near total surgical resection followed by radiotherapy and concurrent chemotherapy with oral Temozolomide (TMZ).[2] This is then followed by adjuvant chemotherapy with TMZ for a period of six months.
The aim of radiotherapy in brain tumors is to maximize the dose delivered to tumor and avoiding dose to surrounding normal brain parenchyma. Long-term radiation toxicity manifests as late neurological sequelae with neurocognitive dysfunction which may be associated with tissue necrosis.[3,4] Techniques of radiotherapy have evolved from 3D conformal radiotherapy (3D-CRT) to intensity modulated radiotherapy and image-guided radiotherapy (IGRT). In advanced techniques, the radiation treatment field can be conformed to the tumor’s shape and the intensity of the beamlets can be modulated, hence, improving therapeutic ratio.[5] This has the implication of reducing the late side effects as well as significant improvement in the quality of life of the patient.
At the time of treatment on the couch, there may be presence of geometrical errors resulting either from patient setup or organ motion. This is why during radiotherapy contouring a setup margin (SM) is applied to clinical target volume (CTV) to form planning target volume (PTV). It is composed of: (1) Internal Margin which includes changes in position, volume and shape of CTV and (2) SM which accounts for errors in patient position on the couch.[6] With the result of this margin, portion of normal brain parenchyma surrounding the treatment volume is included in the study.
A major improvement in precision of radiation treatment was made with the development of image-guided radiation therapy (IGRT). In this technique, an image of the patient is taken on the treatment couch at the time of treatment.
This image is then matched with the initial planning image taken at the time of CT simulation. This leads to accurate and precise patient setup. Such accurate treatment can allow reduction of planning margins. This will lead to a reduction in dose delivered to normal brain parenchyma.[7] At present, several online 2D and 3D imaging devices are directly integrated into the linear accelerator. These include kilovoltage and megavoltage x-ray imaging and kilovoltage and megavoltage cone beam computed tomography (kVCBCT). kV-CBCT utilizes a gantry mounted source with a flat panel detector to take a series of x-ray images and to reconstruct a final 3D image.[8]
Conventionally, couch corrections were applied in three directions, that is, vertical, longitudinal, or lateral. Rotational errors about the superoinferior axis (Roll), anteroposterior axis (Yaw), and mediolateral axis (Pitch) are also errors that can happen at the time of radiation treatment delivery. With newer machines, it is possible to correct the setup uncertainties using 6° of freedom couch which enables corrections in pitch, roll, and rotation along with vertical, longitudinal, and lateral directions. This leads to improvement in accuracy at the time of treatment. The improved accuracy with 6D couch has been described in various studies[9,10] especially in stereotactic radiotherapy treatment for the central nervous system lesions.[11]
The aim of the this study is to analyze the setup errors of patients with GBM treated with IGRT technique using 6D couch corrections, the benefit of applying corrections in 6° of freedom over the conventional three directions and whether any reduction in PTV margin can be done using daily CBCT and 6D couch correction which may help improve therapeutic index.
MATERIALS AND METHODS
After obtaining ethical clearance, we reviewed the treatment of 21 patients (630 radiotherapy sessions). These patients of GBM underwent complete/near total resection and were then taken up for concurrent chemoradiation after discussion in multidisciplinary tumor board.
Radiotherapy planning details
The patients were immobilized using hybrid 3-clamp thermoplastic cast (ORFIT) using standard base plate. CT scan was done using a slice thickness of 0.3 cm. An intravenous contrast was administered at the time of CT simulation. Scan images were taken simultaneously and after a 5-min delay period.
The CT images were then fused with the gadolinium-enhanced post-operative MRI for target delineation. The planning MRI scan was done just one day before radiotherapy planning. Contouring was done as per NRG oncology guidelines.[12] The GTV1 was delineated on T2 image or flair image of post-operative MRI scan which was then circumferentially expanded by 1.5 cm to form CTV1. This was further given a margin of 0.5 cm (as per departmental protocols) to form PTV1. GTV2 was delineated on contrast-enhanced T1C image of post-operative MRI scan which was then circumferentially expanded by 1.5 cm to form CTV2. This was further given a margin of 0.5 cm to form PTV2. The respective doses of PTV1 and PTV2 were 46Gy and 60Gy, respectively, given at 2Gy per fraction. Organ at risk (OAR) was contoured (eyes, eye lens, optic nerves, chiasm, brainstem, hippocampus, cochlea, hypothalamus, and pituitary gland) depending on the areas of brain involved and the constraints used were as defined by QUANTEC guidelines.[13]
Radiotherapy planning was done using Varian ECLIPSE Treatment Planning System Version 15.6. All patients were treated using IGRT technique on Linear Accelerator (True Beam STx – Varian Medical Systems, California).
CBCT analysis
All CBCTs were checked by a single observer (Radiation Oncologist). Six hundred and thirty treatments were delivered and online setup corrections were done. These were corrected and recorded in all six dimensions, that is, vertical, lateral, and longitudinal along with pitch, roll, and rotation. A representative line diagram showing all the 6 axis is shown in [Figure 1]. The three dimensional vector of uncertainty was calculated as square root of the sum of the squares of corrections of each axis which is given in Equation 1.
Equation 1: 3D shift = √ (Vert)2 + (Long)2 + (Lat)2

- Line diagram showing all 6° of freedom.
Analysis was done by calculating the mean shifts in all six dimensions. We determined whether setup errors obtained during the first three fractions could predict the setup errors for the rest of the treatment using daily CBCT (the remaining 27 fractions). We also found the effect of reduced PTV margin of 0.3 cm and analyzed the gain in normal brain sparing.
The benefit and effectiveness of 6D couch over traditional couch shifts (in three directions) were assessed. All the treatment fractions were re-evaluated and the effect of pitch, roll, and rotation was nullified. Based on acquisition position, only vertical, longitudinal, and lateral corrections were applied manually. The mean values of these shifts (with and without 6D couch benefit) were calculated.
Statistical analysis was done using SPSS software version 22 (IBM, Corp, Armonk, NY, USA). Any difference between the two groups was analyzed using Pair t test and an alpha value of <0.05 was considered statistically significant.
RESULTS
A total number of 21 patients of GBM and 630 sessions of radiotherapy treatment were analyzed. Online corrections were made and recorded on 6D treatment couch. These included vertical, longitudinal, and lateral axis corrections along with pitch, roll, and rotation. The average values of the six dimensions are mentioned in [Table 1]. The average 3D shift value during the entire treatment (lateral, longitudinal, and vertical shift) was 0.285. The average values of pitch, roll, and rotation corrections were 1.1, 1.04, and 0.78°.
| Shift | Value |
|---|---|
| Lateral (x) | 0.17 cm±0.09 cm |
| Longitudinal (y) | 0.19 cm±0.15 cm |
| Vertical (z) | 0.11 cm±0.13 cm |
| Pitch | 1.1°±0.84° |
| Roll | 1.04°±0.84° |
| Rotation | 0.78°±0.69° |
The mean shifts obtained during first three sessions were compared with rest of the treatment using daily CBCT (remaining 27 fractions) for all dimensions as shown in [Table 2]. We found out that vertical shift had a statistically different change for the rest of the fractions as compared to first three fractions.
Out of 630 fractions analyzed, only 20 (3.17%) had any shift ≥0.5 cm in either vertical, longitudinal, or lateral direction.
| Shift | First three fractions | Rest of the fractions | P-value |
|---|---|---|---|
| Lateral (x) (cm) | 0.15±0.07 | 0.17±006 | 0.053 |
| Longitudinal (y) (cm) | 0.16±0.06 | 0.17±0.06 | 0.358 |
| Vertical (z) (cm) | 0.08±0.04 | 0.10±0.04 | 0.004 |
| Pitch (degrees) | 1.03±0.61 | 1.18±0.44 | 0.226 |
| Roll (degrees) | 0.93±0.45 | 1.00±0.43 | 0.597 |
| Rotation (degrees) | 0.70±0.48 | 0.76±0.33 | 0.572 |
The central tumors had less setup uncertainty as compared to peripheral tumors. The difference was observed in lateral direction as well as rotational shift; however, it was not statistically different.
In all the patients, the PTV was redrawn with a margin of 0.3 cm. The difference in the volumes of PTV 60Gy and PTV 46Gy is shown in [Table 3]. The average total brain volume was 1288.8 cc.
| PTV | Mean Volume (0.5 cm margin) | Mean Volume (0.3 cm margin) | Mean difference | Significance |
|---|---|---|---|---|
| PTV 60Gy | 310.67 cc±95.14 | 264.90 cc±83.52 | 45.77 cc | Significant |
| PTV 46Gy | 464.98 cc±99.04 | 403.51 cc±86.49 | 61.47 cc | Significant |
All the 630 fractions were reanalyzed in which the effect of 6D couch (pitch, roll, and rotation) was nullified. The CBCTs were manually matched to the acquisition position by a single radiation oncologist in vertical, longitudinal, and lateral directions only without the application of pitch, roll, and rotation. [Table 4] shows the mean difference between the shifts (vertical, longitudinal, and lateral) with or without application of 6D couch. All the shifts showed an increase in value out of which longitudinal shift was statistically different highlighting the benefit of using 6D couch.
| Shift | Shift with 6D couch |
Shift without 6D couch |
P-value |
|---|---|---|---|
| Vertical | 0.17 cm±0.07 | 0.18 cm±0.08 | 0.922 |
| Longitudinal | 0.19 cm±0.13 | 0.27 cm±0.15 | 0.001 |
| Lateral | 0.11 cm±0.13 | 0.13 cm±0.13 | 0.265 |
The average number of sessions per patient that had a correctional shift of >0.3 cm using 6D couch in vertical, longitudinal, and lateral direction was 5. However, when the effect of 6D couch was nullified, the average number of sessions per patient having a shift >0.3 cm was 12 with a significant p value of 0.001 as shown in [Table 5 and Figure 2] that show CBCT analysis at the time of radiation treatment delivery in which unmatched, matched, and with rotational errors despite adequate matching.
| Shift | With 6D couch | Without 6D couch |
|---|---|---|
| Vertical | 2 | 2 |
| Longitudinal | 2 | 8 |
| Lateral | 1 | 2 |
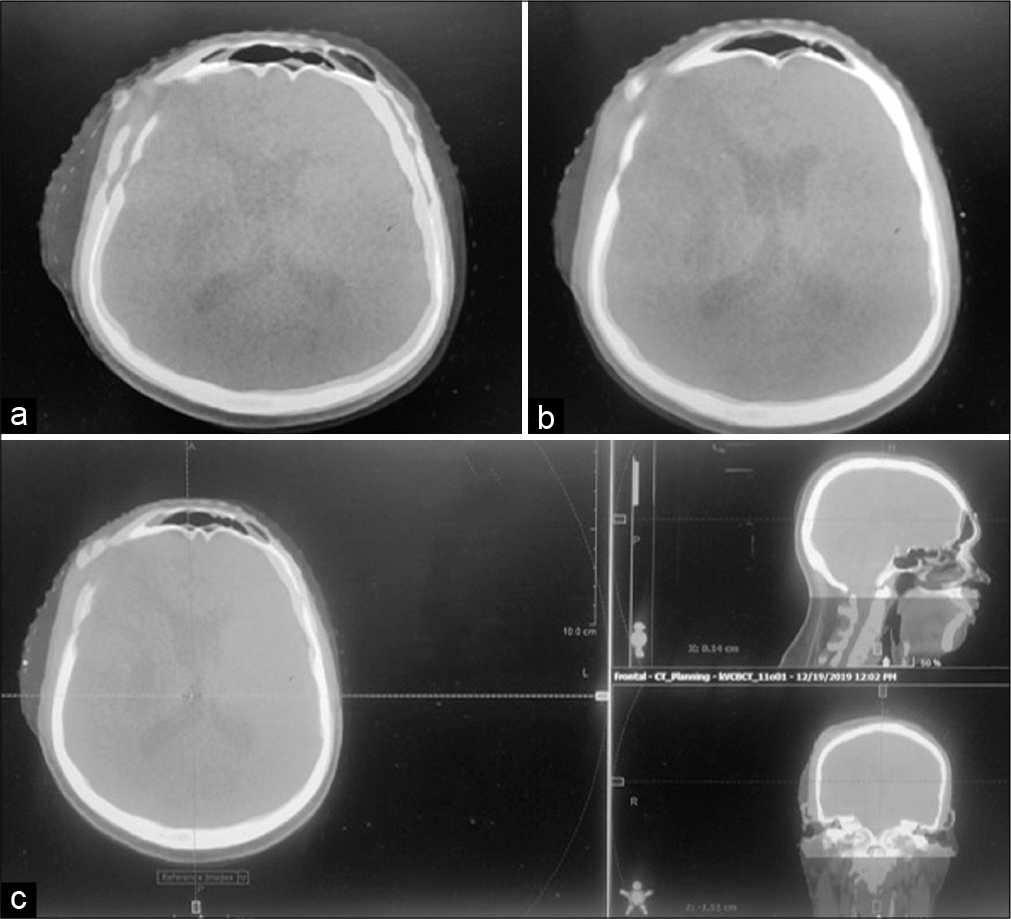
- CBCT analysis at the time of radiation treatment delivery; (a) non-matched superimposed acquisition treatment couch position with CT simulation position, (b) accurately matched acquisition treatment position with CT simulation position using 6D couch, and (c) despite accurate matching in the sagittal and coronal views, complete accurate matching is not possible in the axial view because of rotation error more than 1.5°.
DISCUSSION
The aim of radiotherapy for brain tumors is to deliver precise dose localized at the target area while sparing normal brain tissue as much as possible so as to reduce the long-term neurocognitive side effects. Daily setup variation at the time of treatment may have an adverse impact which includes target under dosage and normal structures receiving a higher dose.[14] With the advent of CBCT and online imaging, the setup and daily variations at the time of treatment have been reduced leading to more precise and accurate treatment. This, in turn, can help us reducing PTV margins during treatment planning so as to spare the normal brain parenchyma as much as possible.
A study done by Beltran et al. has demonstrated that target volume of craniopharyngioma can have daily variation of −20.7% to +82% stressing the need of daily imaging and surveillance.[15] Daily imaging not only corrects the target volume but it gives the confidence to the treating physician of reducing the PTV margins. Beltran et al. have suggested daily setup verification which decreases the PTV margin and minimizes insufficient tumor coverage caused due to setup uncertainties.[16] Similarly, several studies in other organs have demonstrated daily setup variability, for example, Hong et al. demonstrated an absolute average daily setup error of 0.33 cm in any single dimension in head-and-neck cancer patients using conventional mask immobilization while other studies have reported a range of 0.3–0.5 cm in head-and-neck setup variation using weekly portal film measurements.[17] In our department, the standard practice was to apply a PTV margin of 0.5 cm over the CTV when the conventional couch was used and errors were corrected in three dimensions, namely, vertical, lateral, and longitudinal. In this study, we retrospectively reviewed and analyzed 630 fractions of radiotherapy delivered in patients with GBM. We proposed that daily setup verification using CBCT and 6 DOF couch corrections may allow us to reduce the PTV margin to 0.3 cm and hence decrease normal tissue exposure to radiation.
In a study, similar to our study, Lightstone et al. aimed to determine whether smaller PTV margins were feasible using CBCT image guidance system with 6 DOF robotic couch correction in 34 brain tumor patients. A total of 505 radiation fractions were studied to the 34 patients. The median 3D setup positioning error was 2.60 mm. Robotic couch corrections reduced the 3D median error from 2.6 mm to 0.53 mm. They concluded that CBCT image guidance along with a 6-DOF couch correction drastically improves the positional accuracy for patients.[18]
In our study, we found that with daily imaging and setup corrections using a 6D couch, a mean shift of 0.17 cm, 0.19 cm, and 0.11 cm was obtained in vertical, longitudinal, and lateral directions, respectively. The setup variation during first 3 days of IGRT is known to predict patient setup errors for the subsequent fractions. We analyzed separately the setup errors achieved during first three days and compared them with rest of the treatment. We found that vertical shift was increased which was statistically significant so we need to do daily imaging to be more accurate. A study done by Shields et al. showed that the first three days of CBCT predicted setup uncertainty for subsequent treatments and permitted customized CTV to PTV expansion although it was not statistically significant.[19]
CBCTs were reviewed to assess the added benefit of using a 6D couch over conventional couch (in which shifts are applied in three directions – vertical, longitudinal, and lateral). During CBCT analysis, the shifts which had been applied at the time of treatment were negated and position was set as acquisition position. Thereafter, the CBCT was matched to the treatment position (at the time of CT simulation) and the corrections were done only in three directions – vertical, longitudinal, and lateral. These were then compared with the shifts obtained when the errors were corrected in six dimensions. We found statistically significant increase in longitudinal shift when the effect of 6D couch was omitted with the value being 0.27 cm. The vertical and lateral shift also showed a trend to increase; however, it was not statistically significant. One possible reason for this can be attributed to the fact that if corrections are applied in pitch, roll, and rotation axis; it leads to more accurate setup and positioning hence reducing the vertical, lateral, and longitudinal shifts. We also found that accurate matching was not possible when the threshold of rotation was more than 1.5°. This clearly shows the benefit of 6D couch with daily imaging. We also saw that the average number of radiotherapy fractions per patient that had a shift of >0.3cm using 6D couch in vertical, longitudinal, and lateral direction was 5. However, when the effect of 6D couch was negated, the average number of fractions per patient having a shift >0.3cm was 12 with a significant P = 0.001. This clearly shows that when 6D couch is not used, we need to keep the PTV margin of over 0.3 cm.
The PTV margins of 0.5 cm were then redrawn with a PTV margin of 0.3 cm. There was a statistically significant difference between the volumes of normal brain irradiated between the two PTV margins. There was a difference of 45.77 cc and 61.47 cc in the 60Gy and 46Gy volume, respectively. This shows that such a significant amount of normal brain tissue can be spared using a smaller PTV margin. Shields et al. found out that a 0.3 cm margin was adequate for 88% of all the measured shifts using daily imaging. Minimizing CTV to PTV expansion leads to decreased dose to normal brain parenchyma in close proximity to radiation target area. Shields et al. concluded that daily imaging allows application of individualized CTV expansion which decreases dose to OAR and can lead to benefit in terms of neurocognition, learning, and neuroendocrine function.[19]
Limitations of the present study include that it is retrospective in nature. Furthermore, the study does not include long-term clinical follow-up of the patients.
CONCLUSION
We can safely conclude that if daily CBCT is done and setup corrections applied using 6D couch then the PTV margins can be reduced to 0.3 cm which will improve the therapeutic index.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- A clinical review of treatment outcomes in glioblastoma multiforme the validation in a non-trial population of the results of a randomised Phase III clinical trial: Has a more radical approach improved survival? Br J Radiol. 2012;85:e729-33.
- [CrossRef] [PubMed] [Google Scholar]
- Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987-96.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation response of the central nervous system. Int J Radiat Oncol Biol Phys. 1995;31:1093-112.
- [CrossRef] [Google Scholar]
- The radio response of the central nervous system: A dynamic process. Radiat Res. 2000;153:357-70.
- [CrossRef] [Google Scholar]
- Volumetric modulated arc therapy: A review of current literature and clinical use in practice. Br J Radiol. 2011;84:967-96.
- [CrossRef] [PubMed] [Google Scholar]
- The practicality of ICRU and considerations for future ICRU definitions. Semin Radiat Oncol. 2018;28:201-6.
- [CrossRef] [PubMed] [Google Scholar]
- Potential applications of imaging and image-guided radiotherapy for brain metastases and glioblastoma to improve patient quality of life. Front Oncol. 2013;3:284.
- [CrossRef] [PubMed] [Google Scholar]
- Image guidance in radiation therapy: Techniques and applications. Radiol Res Pract. 2014;2014:705604.
- [CrossRef] [PubMed] [Google Scholar]
- Geometric accuracy evaluation of a six-degree-of-freedom (6-DoF) couch with cone beam computed tomography (CBCT) using a phantom and correlation study of the position errors in pelvic tumor radiotherapy. Transl Cancer Res. 2020;9:6005-12.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of a six degrees of freedom couch and an individual head support in patient positioning in radiotherapy of head and neck cancer. Phys Imaging Radiat Oncol. 2019;11:30-3.
- [CrossRef] [PubMed] [Google Scholar]
- Six degrees of freedom CBCT-based positioning for intracranial targets treated with frameless stereotactic radiosurgery. J Appl Clin Med Phys. 2012;13:3916.
- [CrossRef] [PubMed] [Google Scholar]
- NRG brain tumor specialists consensus guidelines for glioblastoma contouring. J Neurooncol. 2019;143:157-66.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative analyses of normal tissue effects in the clinic (QUANTEC): An introduction to the scientific issues. Int J Radiat Oncol Biol Phys. 2010;76:S3-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment accuracy of fractionated stereotactic radiotherapy. Radiother Oncol. 2005;74:53-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dosimetric effect of target expansion and setup uncertainty during radiation therapy in pediatric craniopharyngioma. Radiother Oncol. 2010;97:399-403.
- [CrossRef] [PubMed] [Google Scholar]
- Dosimetric effect of setup motion and target volume margin reduction in pediatric ependymoma. Radiother Oncol. 2010;96:216-22.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of daily setup variations on head-and-neck intensity-modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2005;61:779-88.
- [CrossRef] [PubMed] [Google Scholar]
- Cone beam CT (CBCT) evaluation of inter-and intra-fraction motion for patients undergoing brain radiotherapy immobilized using a commercial thermoplastic mask on a robotic couch. Technol Cancer Res Treat. 2012;11:203-9.
- [CrossRef] [PubMed] [Google Scholar]
- Improvement of therapeutic index for brain tumors with daily image guidance. Radiat Oncol. 2013;8:283.
- [CrossRef] [PubMed] [Google Scholar]







