Translate this page into:
Does indirect decompression by oblique lateral interbody fusion produce similar clinical and radiological outcomes to direct decompression by open transforaminal lumbar interbody fusion
*Corresponding author: Mantu Jain, Department of Orthopaedics, All India Institute of Medical Sciences, Sijua, Bhubaneswar, Odisha, India. montu_jn@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sahoo A, Jain M, Naik S, Das G, Kumar P, Tripathy SK, et al. Does indirect decompression by oblique lateral interbody fusion produce similar clinical and radiological outcomes to direct decompression by open transforaminal lumbar interbody fusion. J Neurosci Rural Pract. 2024;15:53-61. doi: 10.25259/JNRP_322_2023
Abstract
Objectives:
Open transforaminal lumbar interbody fusion (O-TLIF) remains the most popular and widely practiced lumbar fusion method even today, providing direct decompression. Oblique lateral interbody fusion (OLIF) is a novel retroperitoneal approach that allows placement of a large interbody cage which provides an indirect neural decompression, and screws can be placed minimal invasively or through the Wiltse OLIF (W-OLIF) approach. We aim to find out the short-term efficacy of W-OLIF to O-TLIF in terms of radiological and clinical outcomes in patients of lumbar degenerative diseases.
Materials and Methods:
Fifty-two patients were divided equally into two groups (group O-TLIF and group W-OLIF). Several parameters were measured, such as the spinal cord cross-sectional area (SC-CSA), foraminal cross-sectional area (F-CSA), disc height (DH), foraminal height (FH), Schizas grade for stenosis, and Meyerding’s grading for olisthesis. Functional scores were measured using the visual analog scale (VAS) for low back pain (LBP) and lower limbs, Oswestry Disability Index. All parameters were repeat measured at 3 months follow-up. Statistical analysis was done using SPSS software.
Results:
Both groups were similar in composition preoperatively. There was significant improvement in all clinical and radiological parameters post-surgery in either group. However, at 3 months, The DH, FH, FSA, and VAS (LBP) were better in the W-OLIF group than in O-TLIF. Procedure-related complications were seen in both groups (15% in the O-TLIF group and 19% in the W-TLIF group), but only one patient in O-TLIF required revision due to cage migration.
Conclusion:
Similar improvement occurs in most of the clinical and radiological parameters in the W-OLIF group compared to the O-TLIF group. Few radiological parameters such as the DH, FH, and F-CSA and the VAS (LBP) correction are superior in the W-OLIF group in the short-term follow-up. We conclude that indirect decompression by W-OLIF provides equivalent, if not better, results than the traditional O-TLIF lumbar fusion.
Keywords
Lumbar degenerative disease
Fusion
Transforaminal lumbar
INTRODUCTION
Lumbar degenerative disease (LDD) is one of the leading causes that affect the quality of life in an aging population.[1] It can manifest with features of lumbar canal stenosis, often accompanied by an olisthesis that forms part of the degenerative cascade. Symptoms may include intermittent neurogenic claudication, lumbar radiculopathy, and back pain.[2] The primary treatment is always non-surgical, but when this conservative method is exhausted, surgery can be considered. This would require a neural decompression often reinforced with stabilization to achieve a solid fusion.[3] A growing body of evidence consistently demonstrates improved clinical outcomes with lumbar fusions for patients who fail conservative care.[4]
Transforaminal lumbar interbody fusion (TLIF) is one of the most common, which allows direct neural decompression by inserting an interbody cage packed with bone graft through the transforaminal approach. Conventionally, it is done by the open TLIF (O-TLIF) method, and subsequently, it has been improved and improvised to a minimally invasive TLIF (MIS-TLIF) for practice. The outcome has been similar in reported studies.[5-7]
Oblique lateral interbody fusion (OLIF) was introduced in 2012, which allows direct access to the disc space through a retroperitoneal approach and facilitates the placement of a large interbody cage, which provides an indirect neural decompression. The approach is considered less surgical invasive.[8] The initial results have been compared with those of MIS-TLIF in published literature, with minor advantages of one over the other in a few parameters.[9-15]
In developing countries like ours, O-TLIF remains the most popular and widely practiced method of lumbar fusion. There has been no comparison of OLIF to O-TLIF, and one of the logical arguments could be comparing a minimally invasive method to an open one. Therefore, we altered the OLIF by adding the Wiltse approach for pedicle screw insertion rather than the percutaneous approach and called it a “W-OLIF” approach. In this prospective study design, we aimed to find out the short-term efficacy of W-OLIF to O-TLIF in terms of radiological and clinical outcomes in patients of LDDs interbody fusion and oblique lateral interbody fusion.
MATERIALS AND METHODS
Patient population
Patients who had undergone lumbar fusion surgery were included in our study after approval from our institutional human ethics committee (IEC/2020-21/81). The study was in accordance with Helsinki Declaration of 1975, as revised in 2000. This prospective comparative study was conducted from January 2021 to December 2022. Informed consent was obtained from all patients before participation in the study. Patients undergoing W-OLIF consented to a second surgery (direct decompression) after 3 months if their symptoms were not resolved and residual stenosis was observed in repeat magnetic response imaging (MRI).
The inclusion criterion was patients undergoing single or double-level lumbar fusion surgery due to degenerative conditions (stenosis ± olisthesis ≤ grade 2) or a symptomatic isthmic olisthesis ≤2 grades. Patients who had exhausted conservative treatment for at least 6 months were recruited. Patients with degenerative spondylolisthesis with grade >II, multi-segment lumbar fusion, history of previous spine surgery, or patients with a diagnosis of spinal tumor/spinal infections/vertebrae fractures/severe osteoporosis were excluded from our study. Patients with the previous abdominal surgery from the left retroperitoneal approach were excluded from W-OLIF.
Sample size
There were 52 patients divided equally into both groups (group O-TLIF and group W-OLIF). The sample size was calculated based on the assumption of a minimum difference of 25% of spinal canal cross-sectional area (SC-CSA) between OLIF with that of TLIF groups with a power of 80– 95% confidence interval using the www.powerandsamplesize.com calculator.
Outcome measurement
The demographic details of the patients were recorded. Pre-operative radiological evaluations included X-rays, non-contrast computed tomography, and MRIs of the spine. Several parameters were measured, such as the spinal cord cross-sectional area (SC-CSA), foraminal cross-sectional area (F-CSA), disc height (DH), foraminal height (FH), Schizas grade for stenosis, and Meyerding’s grading for olisthesis. Functional scores were measured using the visual analog scale (VAS) for low back pain (LBP) and lower limbs, and Oswestry Disability Index. All parameters were repeat measured at 3 months follow-up.
Surgical technique
O-TLIF
In the prone position, using a posterior midline incision, the paraspinal muscles were dissected [Figure 1a]. Pedicular screws were inserted in appropriate levels, confirmed with fluoroscopy [Figure 1b]. Direct decompression was done by doing hemilaminectomy and facetectomy of the affected side in case of unilateral affection [Figure 1c]. Over-the-top decompression was done on the contralateral side in bilateral affection. Then disc space was prepared, and an appropriate-sized TLIF cage was inserted with autologous locally harvested graft [Figure 1d, e and f]. Rods were connected and tightened after compression [Figure 1].
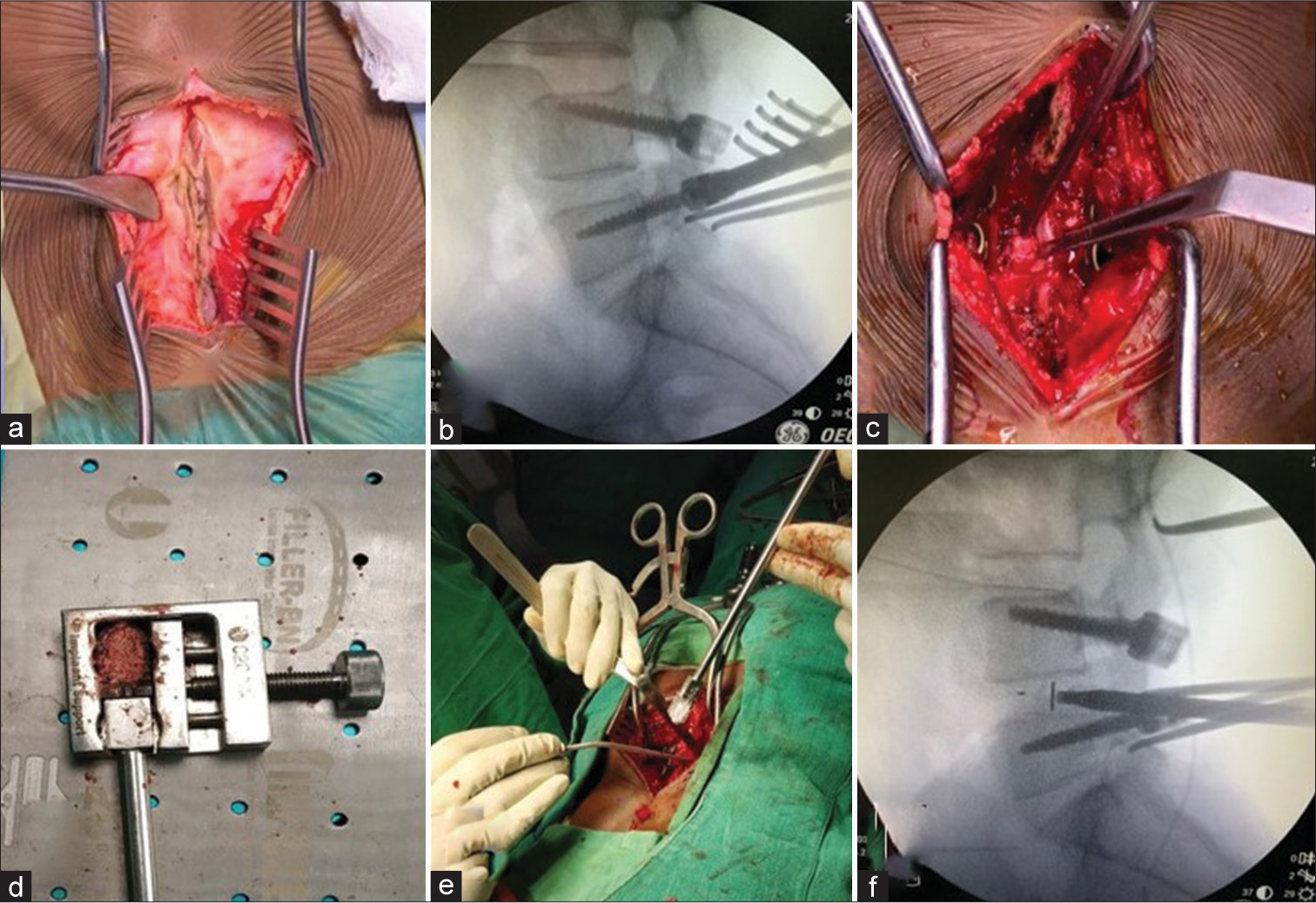
- Steps of open transforaminal lumbar interbody fusion. a- the posterior approach midline approach in a; b- pedicle screw insertion; c-decompression done; d, e, and f- insertion of the interbody cage.
W-OLIF
The patient was first positioned in a right-lateral position and secured with the help of straps [Figure 2]. The level of our interest was marked under fluoroscopy [Figure 3]. A 5 cm skin incision was followed by splitting of successive muscles and retroperitoneal space was reached. The interval between the great vessels and psoas muscle was exploited to expose the disc space. It was confirmed under fluoroscopy, and a tubular retractor system was applied [Figure 2]. A discectomy was done, and an endplate was prepared [Figure 3]. An autologous bone graft was taken from the adjacent iliac crest through the same incision, and an appropriate-sized intervertebral cage-packed graft was inserted [Figures 2 and 3]. This wound was closed, and the patient was turned prone on the operating table. A muscle- splitting Wiltse approach was undertaken, pedicle screws were inserted after being verified under fluoroscopy, and final rods were connected and tightened [Figures 2 and 3].[16] The wound was closed and dressed.
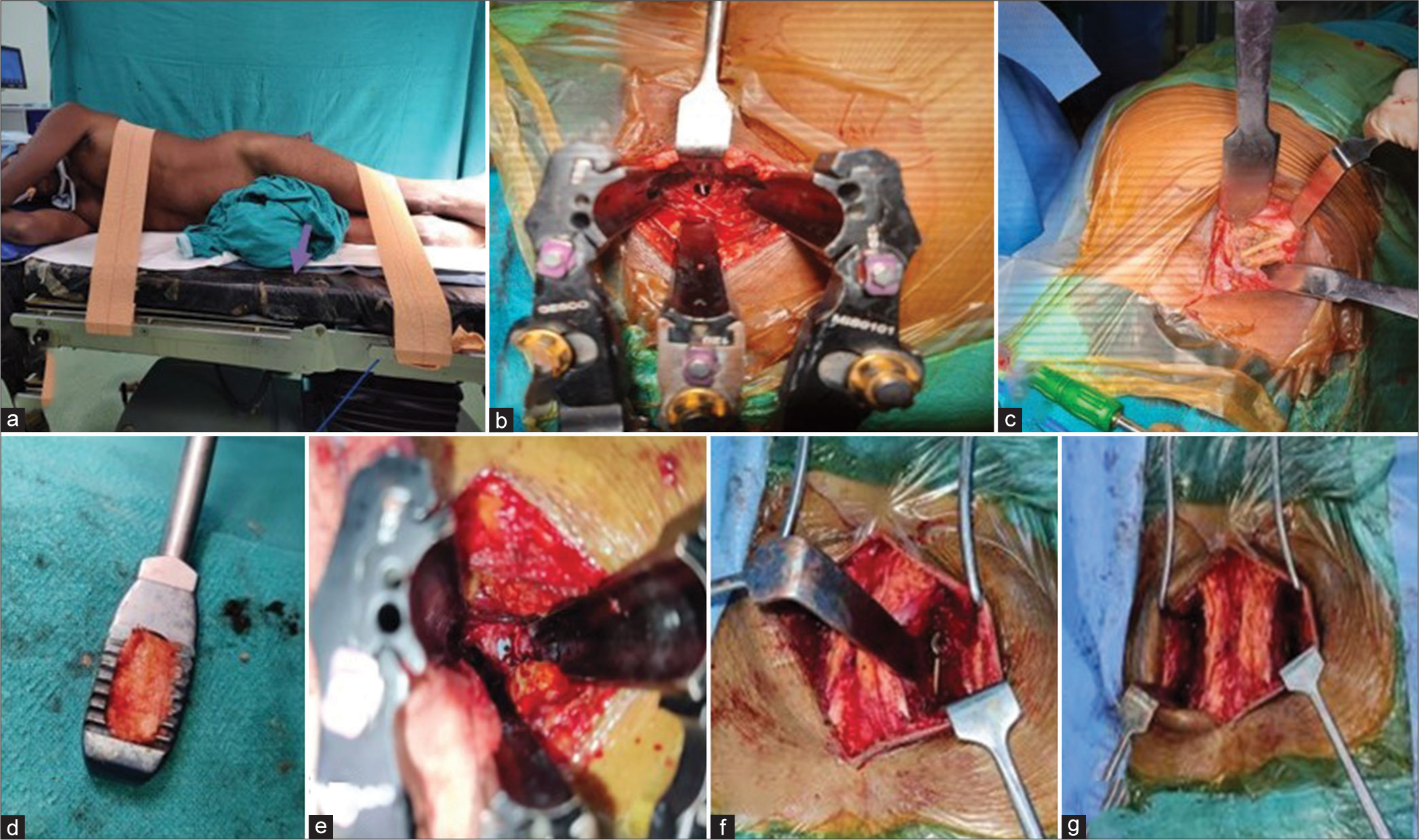
- Steps of the Wiltse oblique lateral inetrbody fusion. a-the right lateral positioning; b-self-retaining retractors showing the disc space; c-the harvest of iliac crest graft;d-e-preparation and insertion of cage, f and g- insertion of pedicle screws by Wiltse approach).
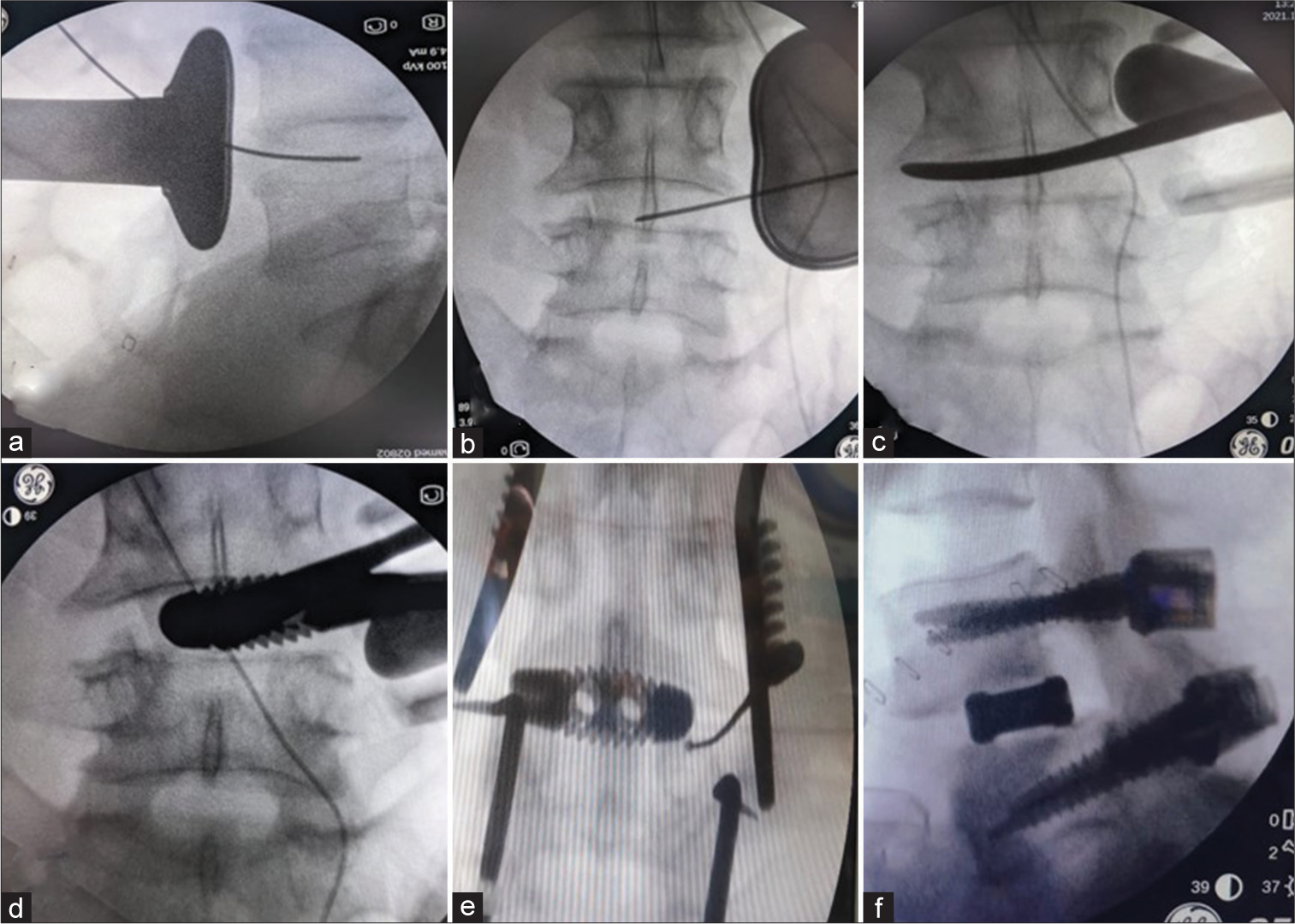
- Intra-operative steps of the Wiltse oblique lateral interbody fusion. a-b-The confirmation of level and also the location of guide wire in the part of disc; c-the release of opposite annulus as part of disc space preparation;d- insertion of cage (d);e and f- insertion of pedicle screws.
Postoperatively, the patients were mobilized with a walker as soon as they could tolerate the pain.
Statistical analysis
The data were entered into a computer-based spreadsheet and analyzed using SPSS 26.0. The Shapiro–Wilk test was used to check for the normality of data. Categorical data were analyzed using the Chi-square test. Data were analyzed using an independent t-test and paired t-test for comparing pre-and post-values graphs were made using Microsoft Excel 2016.
RESULTS
A summary of baseline demographic characteristics and pre-operative radiological and clinical data has been presented in [Tables 1 and 2]. Both groups were similar in composition. Post-operative data for clinical and radiological parameters are displayed in [Table 2]. There was a significant improvement in all the parameters in both groups compared to their pre-operative values. The changes in the parameters were also analyzed between the groups, and we found that FH, F-CSA, DH, and VAS-LBP were better in the W-OLIF group as compared to the O-TLIF group, as seen in [Table 3].
| Variables | TLIF n (%) | OLIF n (%) | P-value |
|---|---|---|---|
| Age (in years) (mean±SD) | 50.38±12.20 | 47.31±10.11 | 0.33 |
| Gender | |||
| Male | 12 (46.1) | 8 (30.8) | 0.25 |
| Female | 14 (53.9) | 18 (69.2) | |
| Level of surgery | |||
| Single level | 23 (88.5) | 22 (84.6) | 0.19 |
| Double level | 03 (11.5) | 04 (15.4) | |
| Mayerding’s grading | |||
| No olisthesis | 03 (11.5) | 01 (3.8) | 0.72 |
| Grade 1 (0–25%) | 14 (53.9) | 17 (65.5) | |
| Grade 2 (25–50%) | 09 (34.6) | 08 (30.7) | |
| Schizas grading | |||
| Grade A | 02 (7.7) | 06 (23.1) | 0.05 |
| Grade B | 07 (26.9) | 13 (50.0) | |
| Grade C | 15 (57.7) | 06 (23.1) | |
| Grade D | 02 (7.7) | 01 (3.8) | |
SD: Standard deviation, TLIF: Transforaminal lumbar interbody fusion, OLIF: Oblique lateral interbody fusion
| Variables | TLIF (mean±SD) | OLIF (mean±SD) | P-value | TLIF group (mean±SD) | OLIF group (mean±SD) | P-value |
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | |||||
| SC-CSA (in cm2) | 0.77±0.37 | 0.79±0.35 | 0.72 | 1.32±0.40 | 1.31±0.50 | 0.64 |
| Right F-CSA (in cm2) | 0.46±0.16 | 0.43±0.12 | 0.71 | 0.71±0.15 | 0.79±0.23 | 0.15 |
| Left F-CSA (in cm2) | 0.46±0.12 | 0.42±0.12 | 0.23 | 0.70±0.12 | 0.80±0.28 | 0.14 |
| DH (in mm) | 6.70±1.43 | 6.48±1.47 | 0.59 | 9.42±1.97 | 10.28±2.42 | 0.18 |
| Right FH (in mm) | 12.44±2.39 | 12.31±2.39 | 0.84 | 14.77±2.25 | 17.09±2.81 | 0.002 |
| Left FH (in mm) | 12.62±2.22 | 12.20±2.65 | 0.54 | 15.29±2.70 | 16.98±2.56 | 0.02 |
| ODI (in %) | 64.38±8.75 | 67.00±6.15 | 0.22 | 29.62±6.3 | 31.69±7.28 | 0.27 |
| VAS score (low back pain) | 7.92±0.89 | 8.23±0.65 | 0.15 | 3.58±1.03 | 2.88±0.77 | 0.01 |
| VAS score (lower limb pain) | 7.50±1.03 | 7.85±1.08 | 0.26 | 3.00±0.89 | 3.15±0.88 | 0.42 |
SD: Standard deviation, CSA: Cross-sectional area, SC: Spinal canal, F: Foremen, DH: Disc height, FH: Foramen height, ODI: Oswestry disability index, VAS: Visual analog scale, TLIF: Transforaminal lumbar interbody fusion, OLIF: Oblique lateral interbody fusion
| TLIF (mean±SD) | OLIF (mean±SD) | P-value | |
|---|---|---|---|
| SC-CSA (in cm2) | 0.56±0.30 | 0.51±0.41 | 0.32 |
| Right F-CSA (in cm2) | 0.24±0.11 | 0.36±0.19 | 0.03 |
| Left F-CSA (in cm2) | 0.24±0.11 | 0.38±0.15 | 0.04 |
| DH (in mm) | 2.73±2.40 | 3.80±2.10 | 0.025 |
| Right FH (in mm) | 2.33±2.01 | 4.78±2.68 | <0.001 |
| Left FH (in mm) | 2.66±2.19 | 4.77±2.22 | 0.001 |
| ODI (in %) | 35.13±10.41 | 35.39±10.73 | 0.85 |
| VAS score for LBA | 4.3±1.36 | 5.3±1.02 | 0.003 |
| VAS score for lower limb pain | 4.61±1.59 | 4.74±1.45 | 0.74 |
SD: Standard deviation, CSA: Cross-sectional area, SC: Spinal canal, F: Foremen, DH: Disc height, FH: Foramen height, VAS: Visual analog scale, TLIF: Transforaminal lumbar interbody fusion, OLIF: Oblique lateral interbody fusion, ODI: Oswestry disability index, LBP: Low back pain
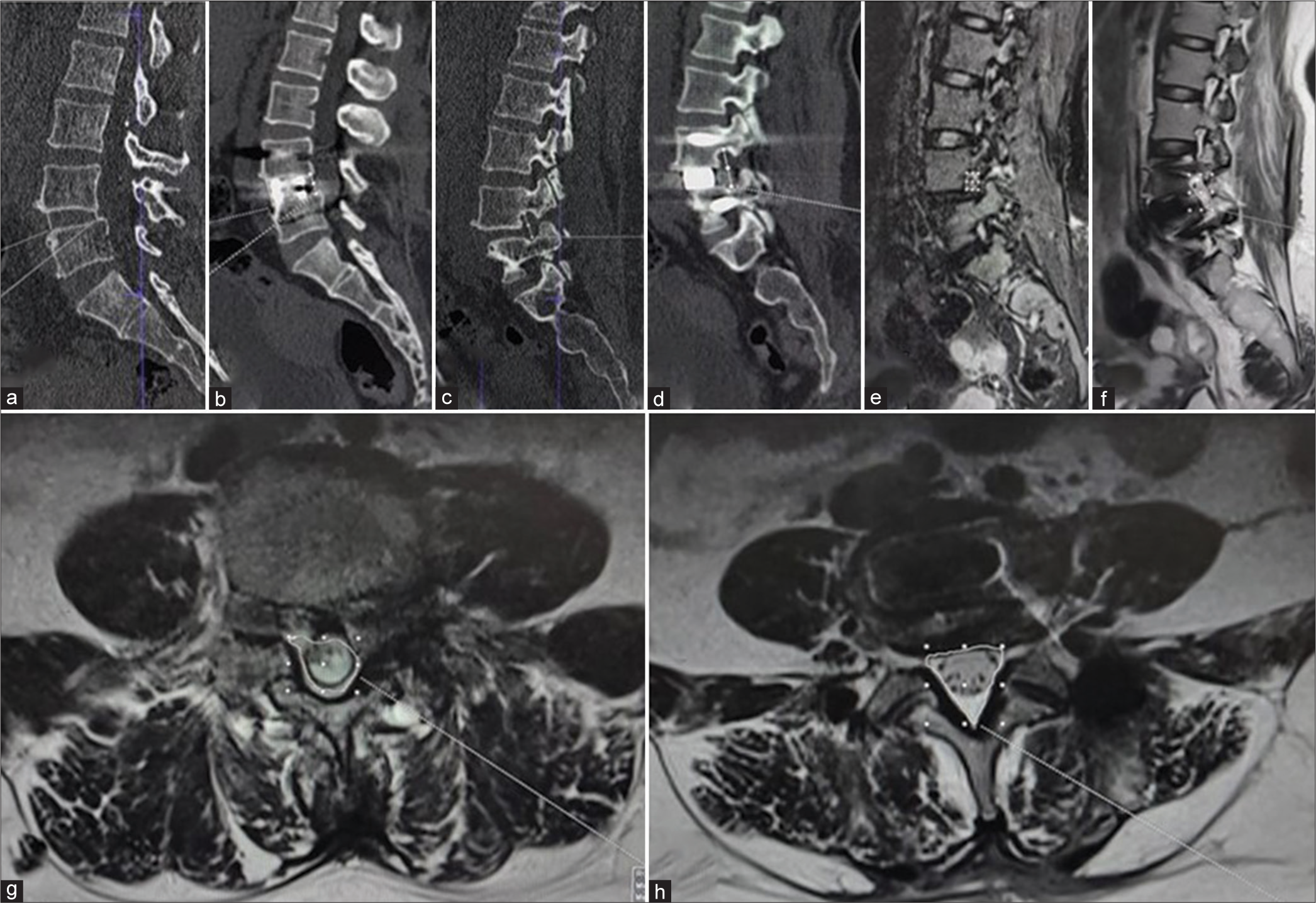
[Figures 4 and 5] illustrate the radiological measurement of a patient from each group. The mean duration of surgery was found to be significantly less in the case of O-TLIF (112.85 ± 29.13 min vs. 155.15 ± 27.41) and the mean intra-operative blood loss was less in the W-OLIF group (275 ± 37 vs. 458 ± 52.6 mL) in the O-TLIF group. The mean hospital stay was similar in both groups (5.5 ± 4 for the W-OLIF, 5.8 ± 7).
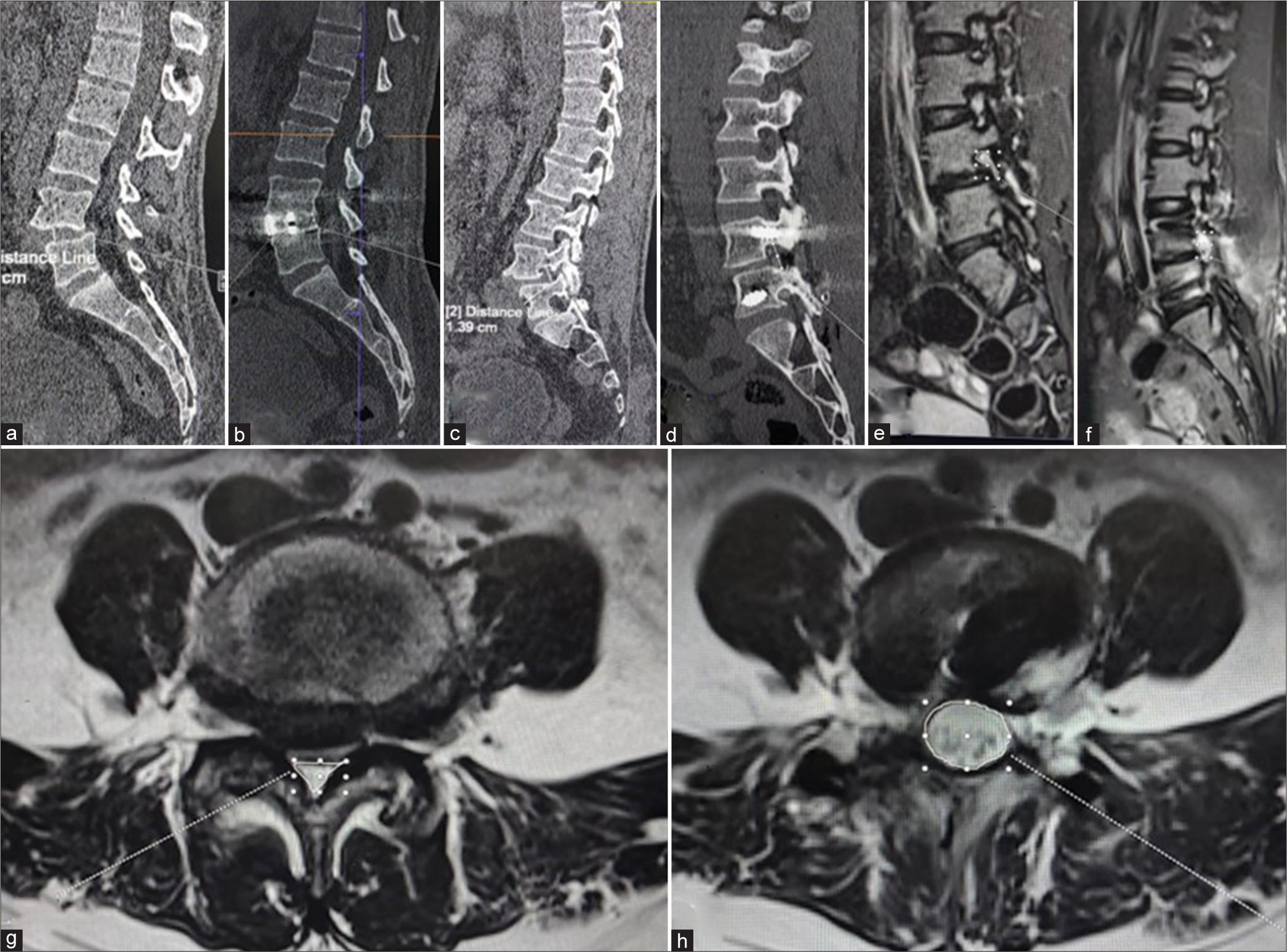
- Images demonstrating radiological parameters are measured in a patient who underwent open transforaminal lumbar interbody fusion. The measurement on the computed tomography scans (a and b)- disc height, (c and d)- foramen height; measurement on the magnetic resonance imaging (e and f)-the foramen cross sectional area, (g and h)- spinal cord cross sectional area.
- Images demonstrating radiological parameters are measured in a patient who underwent Wiltse oblique lateral interbody fusion. The measurement on the computed tomography scans (a and b)- disc height, (c and d)- foramen height; measurement on the magnetic resonance imaging (e and f)-the foramen cross sectional area, (g and h)- spinal cord cross sectional area.
Few complications occurred in both groups. In the O-TLIF, two patients (8%) had an intra-operative dural tear that required suturing. One patient (4%) had superficial surgical site infections (that required prolonged antibiotics) and one patient (4%) had a cage back out that needed redo surgery. In the W-OLIF group, three patients (11.5%) developed paresthesia over the thigh, two (8%) had mild hip flexor weakness (4/5 on MRC grading), and one (4%) quadriceps weakness (4/5 on MRC grading). All of these completely recovered at 3-month follow-up period. No patient in the W-OLIF group complained of the persistence of symptoms warranting posterior decompression as informed pre-operatively. One patient each of O-TLIF [Figure 4] and W-OLIF [Figure 5] are illustrated.
DISCUSSION
O-TLIF is currently the gold standard for a lumbar fusion where spinal decompression is done by direct decompression. Nevertheless, this technique has chances of paraspinal muscle damage, dural tears, and post-operative nerve adhesions.[17] This has made surgeons improvise to MIS-TLIF. Unfortunately, MIS-TLIF has a learning curve, requires a lot more patience, is more time-consuming, needs a microscope/loop, and causes higher radiation exposures.[18,19] Alternative fusion approaches such as the OLIF have been introduced and practiced.[8] Several studies have compared the MIS-TLIF and OLIF used in minimally invasive ways and found them to have similar functional outcomes.[9,11,12,15,20] Despite this, OLIF has gained less popularity. The possible reasons are (1) percutaneous pedicle screw would need higher skills, radiation exposure, and implant cost, (2) surgeons well versed in this would be content to do a one-position MIS-TLIF, and (3) most surgeons like direct decompression and are not very sure about indirect decompression and hence would not venture to OLIF. Therefore, MIS-TLIF is restricted to fewer sophisticated centers, whereas O-TLIF is widely practiced. OLIF (minimally invasive) is further confined to a subset of these MIS-TLIF practicing surgeons.
Yet, the advantages of OLIF need consideration. It is a muscle-splitting, thus sparing approach, and allows the use of a wide cage augmented with posterior fixation. The large cage is mounted on the rigid epiphyseal ring around the vertebral body rather than a small-sized cage used in the relatively weak central zone of the endplate in TLIF. Consequently, the DH, FH, and F-CSA improved and were found to be better in our study’s W-OLIF group than the O-TLIF group. The SC-SCA also was improved and comparable to that achieved with the O-TLIF method. Other investigators have yet to study this parameter. Few other researchers also found that OLIF produced better disc height restoration.[15,21] The VAS for the back also scored better in our W-OLIF group in comparison to the O-TLIF group. Sheng et al. also found in their study that VAS back pain improvement was 71% in the OLIF in comparison to MIS-TLIF, which had a 62% improvement.[21] Such a finding was also reiterated by Han et al., who found VAS (LBP) was better at 3 months in the OLIF group, but subsequently, it was similar.[15] The VAS score is expected to be reduced once fusion has occurred.
In our study, we have got significantly less operative time in O-TLIF than in W-OLIF (112.85 ± 29.13 vs. 155.15 ± 27.41). Modi and Shrestha reported slightly higher operative time in the O-TLIF group (130.8 ± 15.2); in the MIS-TLIF group, it was even more (170.1 ± 18.8).[22] The W-OLIF operating time was higher, which can be explained by the time lost while turning the patient on the table from a lateral position to a prone position for the placement of pedicular screws through the Wiltse approach. In one study of W-OLIF, Zhu et al. recorded a lesser surgical time (110.5 ± 37.8) and lower blood loss as compared to ours (123.1 ± 39.8 mL vs. 275 ± 37).[11] Their patient was single level, unlike ours, where we had four patients in double level. This could also be differences in the expertise of the surgeons. However, since both approaches for our OLIF are muscle-splitting approaches, the blood loss is less compared to the O-TLIF method, which had a loss of 458 ± 52.6 mL. Still, our blood loss was higher than Modi and Shrestha, who reported 289.7 6 58.5 mL in the O-TLIF cohort.[22]
Four patients in O-TLIF (15.4%) had complications. Similar to Modi and Shrestha who reported a rate of 11.8%.[22] A few patients in our W-OLIF group complained of thigh pain, paresthesia, hip flexor, and quadriceps weakness. Xu et al. attributed this to the lumbar plexus retraction and psoas contusion.[23] In another study, Fujibayashi et al. reported transient leg weakness (7.1%) and numbness (21.4%).[2] Both this paresthesia and weakness recovered entirely in the 3-month follow-up period in our patients. In a meta-analysis, Zhang et al. found no differences in overall complication rates between OLIF and MIS-TLIF groups.[24] However, more recently, Zhu et al. MIS-TLIF outweighs OLIF in terms of complications.[11]
The present study is the first study to compare the O-TLIF with a W-OLIF. W-OLIF is a muscle-splitting approach on the lateral and posterior sides. This has made it possible to use conventional screws, which are cost-effective, technically easier to insert (than minimal invasive screws), and avoid radiation exposure. The essence of OLIF, that is, indirect decompression is preserved. However, we acknowledge there are a few limitations to our study. First, this is a single-center study and a small sample size. Our outcome measures are short-term (3 months). The surgeons were novices to the technique of OLIF. Therefore, they planned to review the patients at 3 months and do surgical decompression if needed due to the persistence of pre-operative complaints. This study did not include long-term outcomes in terms of patient relief, development of adjacent disk disease, and persistence of improving radiological parameters.
Nevertheless, this gives a future direction for research with larger sample sizes, multicentric studies, and conducting randomized controlled trials to validate our findings. Another potential opportunity would be to compare the long-term outcomes. However, our study provides some hope to surgeons who are masters of O-TLIF but hesitate to adapt to OLIF procedures.
CONCLUSION
Similar improvement occurs in most of the clinical and radiological parameters in the W-OLIF group compared to the O-TLIF group. Few radiological parameters such as the DH, FH, and F-CSA and the VAS (LBP) corrections are superior in the W-OLIF group in the short-term follow-up. We conclude that indirect decompression by W-OLIF provides equivalent, if not better, results than the traditional O-TLIF lumbar fusion.
Ethical approval
The authors declare that they have taken the ethical approval from IRB/IEC.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 2015;40:E175-82.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical treatments for lumbar spine diseases (TLIF vs. Other Surgical Techniques): A systematic review and meta-analysis. Front Surg. 2022;9:829469.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of oblique lateral interbody fusion and transforaminal lumbar interbody fusion for lordosis correction in degenerative lumbar diseases. Zhonghua Yi Xue Za Zhi. 2018;98:1990-5.
- [Google Scholar]
- Comparison of perioperative and postoperative outcomes of minimally invasive and open TLIF in obese patients: A systematic review and metaanalysis. J Pain Res. 2022;15:41-52.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of minimally invasive and open TLIF outcomes with more than seven years of follow-up. North Am Spine Soc J. 2022;11:100131.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of minimally invasive versus open transforaminal interbody lumbar fusion. Glob Spine J. 2020;10:143S-50.
- [CrossRef] [PubMed] [Google Scholar]
- Oblique lumbar interbody fusion: Technical aspects, operative outcomes, and complications. World Neurosurg. 2017;98:113-23.
- [CrossRef] [PubMed] [Google Scholar]
- Transforaminal lumbar interbody fusion (TLIF) versus oblique lumbar interbody fusion (OLIF) in interbody fusion technique for degenerative spondylolisthesis: A systematic review and meta-analysis. Life (Basel). 2021;11:696.
- [CrossRef] [PubMed] [Google Scholar]
- OLIF versus MI-TLIF for patients with degenerative lumbar disease: Is one procedure superior to the other? A systematic review and meta-analysis. Front Surg. 2022;9:1014314.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for treatment of lumbar degeneration disease: A prospective cohort study. Spine (Phila Pa 1976). 2022;47:E233-42.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative analysis of the effects of OLIF and TLIF on adjacent segments after treatment of L4 degenerative lumbar spondylolisthesis. J Orthop Surg Res. 2022;17:203.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of outcomes between indirect decompression of oblique lumbar interbody fusion and MIS-TLIF in one single-level lumbar spondylosis. Sci Rep. 2021;11:12783.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between oblique lumbar interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MISTLIF) for lumbar spondylolisthesis. Neurol India. 2022;70:127-34.
- [CrossRef] [Google Scholar]
- Comparison of outcomes between robot-assisted minimally invasive transforaminal lumbar interbody fusion and oblique lumbar interbody fusion in single-level lumbar spondylolisthesis. Orthop Surg. 2021;13:2093-101.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the wiltse approach and percutaneous pedicle screw fixation under O-arm navigation for the treatment of thoracolumbar fractures. Orthop Surg. 2021;13:1618-27.
- [CrossRef] [PubMed] [Google Scholar]
- Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089-92.
- [CrossRef] [PubMed] [Google Scholar]
- Learning curve of MIS-TLIF using 22 mm-tubular retractor in degenerative spondylolisthesis (Grade 1-2)-a review over 100 cases. J Minim Invasive Spine Surg Tech. 2020;5:20-5.
- [CrossRef] [Google Scholar]
- Radiation exposure in minimally invasive transforaminal lumbar interbody fusion: The effect of the learning curve. Int J Spine Surg. 2019;13:39-45.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing oblique lumbar interbody fusion with lateral screw fixation and percutaneous endoscopic transforaminal discectomy (OLIF-PETD) and minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for the treatment of lumbar disc herniation complicated with lumbar instability. BMC Musculoskelet Disord. 2022;23:1104.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive surgery for degenerative spondylolisthesis: Transforaminal or oblique lumbar interbody fusion. J Comp Eff Res. 2020;9:45-51.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of clinical outcome and radiologic parameters in open TLIF versus MIS-TLIF in single-or double-level lumbar surgeries. Int J Spine Surg. 2021;15:962-70.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: A literature review. Ann Transl Med. 2018;6:104.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive transforaminal lumbar interbody fusion versus oblique lateral interbody fusion for lumbar degenerative disease: A meta-analysis. BMC Musculoskelet Disord. 2021;22:802.
- [CrossRef] [PubMed] [Google Scholar]







