Translate this page into:
Distal vertebral artery pseudoaneurysm coiling using dual microcatheter “handshake” technique – A surgical challenge
*Corresponding author: Rohit Kamlesh Yadav, Department of Neurosurgery, IPGMER and SSKM Hospital, Kolkata, West Bengal, India. rohityadav1992@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yadav RK, Chaudhuri S, Sundara S, Multani PB. Distal vertebral artery pseudoaneurysm coiling using dual microcatheter “handshake” technique – A surgical challenge. J Neurosci Rural Pract. 2024;15:162-4. doi: 10.25259/JNRP_481_2023
Dear Editor,
The incidence of traumatic pseudoaneurysms of the vertebral artery and its branches is thought to be 0.01%. Trauma to the vertebral artery and its segments following head-and-neck injury may lead to pseudoaneurysm formation. These aneurysms can attain a large size causing symptoms due to compression of the adjacent neural structures or sometimes they may rupture spontaneously causing a local neck mass. They may also cause neurological symptoms due to microemboli in the posterior circulation. They may uncommonly present with neck pain and headache. These pseudoaneurysms carry a significant risk of embolic stroke and mortality.
We report one such intriguing case of a pseudoaneurysm of the left distal V4 segment of the vertebral artery that presented later than expected. Although uncommon, traumatic vertebral artery pseudoaneurysms can be fatal, thus prompt diagnosis and treatment are crucial.[1] With this case report, we would like to highlight the challenges in the coiling technique in a patient with distal vertebral artery pseudoaneurysms.[2] A woman in her 40s presented with a history of sudden onset headache and loss of consciousness 1 month ago. She also had a history of head trauma with a substantial impact across the left side of her neck, but she did not receive any treatment for it. Over a period of 1 month, she developed a progressive weakness in the left upper limb and slurring of speech. On examination, the patient was conscious and oriental with time, place, and person. There was no obvious facial asymmetry. The left shoulder and elbow weakness was noted with a power of 2/5. Power in the left wrist was 4/5. Deep tendon reflexes were mildly exaggerated in the left upper limb. Sensory examination in the left upper limb was normal. No sensorimotor deficit was noted in the right upper limb. Sensorimotor examination of bilateral lower limbs was normal. On investigations non-contrast computerized tomography brain revealed a posterior fossa bleed on radiological examination.
Magnetic resonance imaging (MRI) angiogram [Figure 1] showed a large lobulated soft-tissue mass of 25 mm × 40 mm × 31 mm on the left side of the craniovertebral (C-V) junction extending exophytically to the occipital region. The mass was strongly enhanced in the arterial phase and became dense in the post-venous phase suggestive of pseudoaneurysm. The diagnosis of a pseudoaneurysm originating from the V4 segment of the vertebral artery with a vertebrojugular fistula was confirmed by a digital subtraction angiography (DSA) [Figure 2] that was performed.[3] The distal left vertebral artery (LVA) pseudo aneurysm was verified by DSA [Figure 2a and b] after the patient was hospitalized in the neurocritical care unit and received promptly supportive therapy. Thereafter, the patient was taken for intervention, where the bilateral vertebral artery was accessed. The first microcatheter was placed in the LVA [Figure 3a] proximal to the left posterior inferior cerebellar artery and 2nd was placed past the aneurysm. Interlocking coils deployed by face-to-face dual microcatheter technique [Figure 3b] to close off the distal limb of the LVA. Thereafter the right vertebral microcatheter was removed and the left microcatheter was used to coil the pseudoaneurysm pouch and then the proximal LVA till total occlusion [Figure 4a and b]. One of the delayed catastrophic effects of head injury can be diagnosed and prevented by this method.[3] The procedure was successful without any complications. Follow-up DSA after 7 days showed good occlusion of the pseudoaneurysm.[3] A post-operative MRI of the brain with C-V junction [Figure 5] cuts was done after 8 weeks which showed complete occlusion with pseudomeningocele formation with total obliteration of the venous pouch and no infarct in the brain[3] and the patient showed clinical improvement.
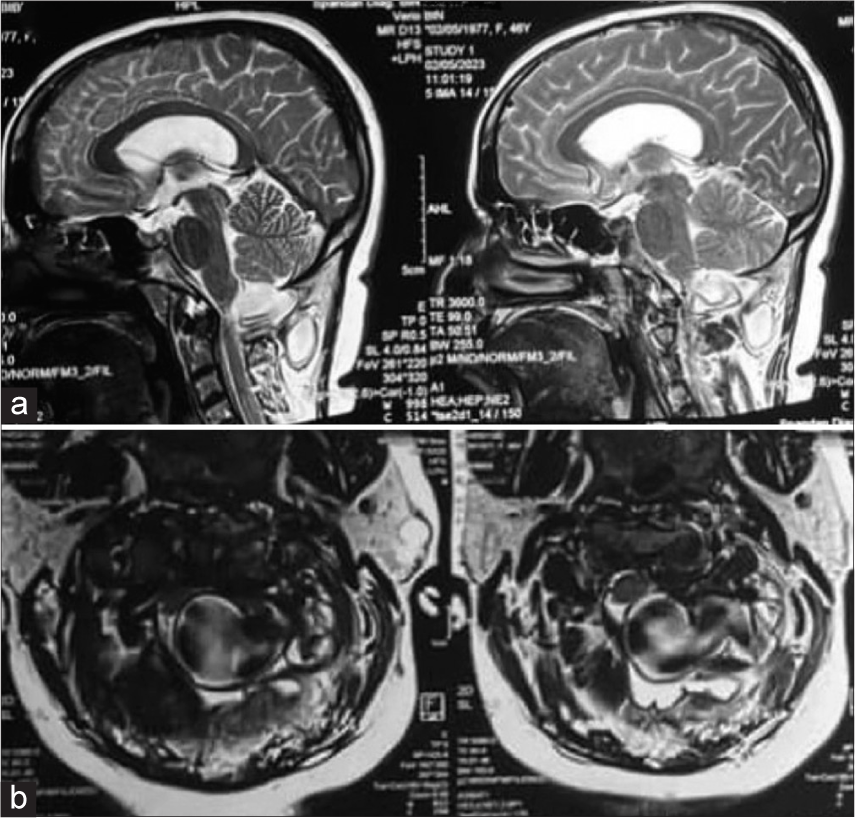
- (a and b) Pre-op T2W2 magnetic resonance imaging brain and cervical spine axial and sagittal cuts s/o large isointense lobulated mass (25 × 40 × 31 mm) seen in the left side craniovertebral junction extending exophytically to occipital scalp, Mass strongly enhances in the arterial phase and becomes dense in post venous phase.
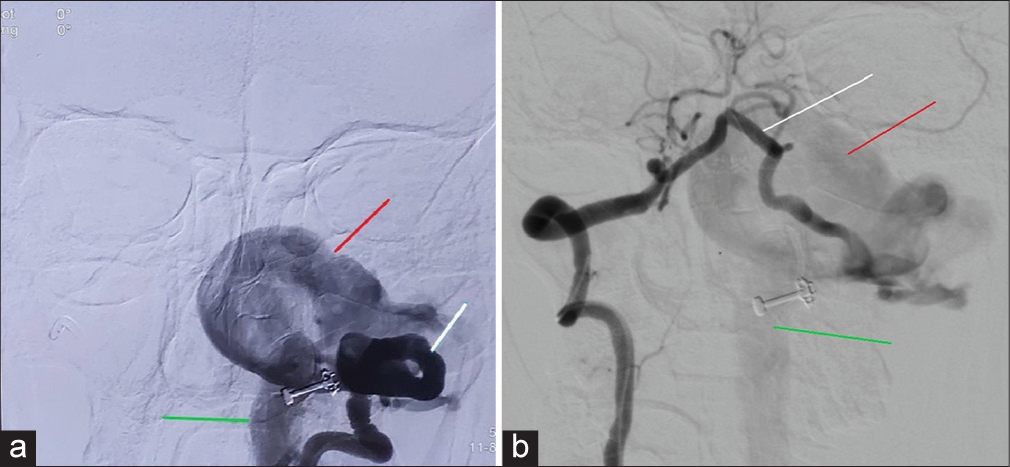
- (a and b) Pre-operative digital subtraction angiography (AP and lateral) – white line (left v4 segment artery), red line (pseudoaneurysm), green line (left draining IJV).
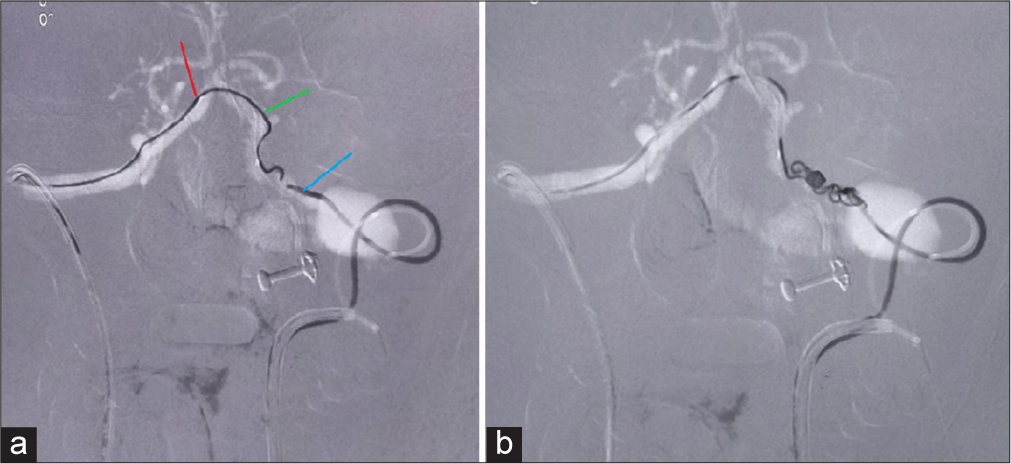
- (a and b) Intraoperative digital subtraction angiography – red (right microcatheter), green (coil from right microcatheter), and blue (left microcatheter).
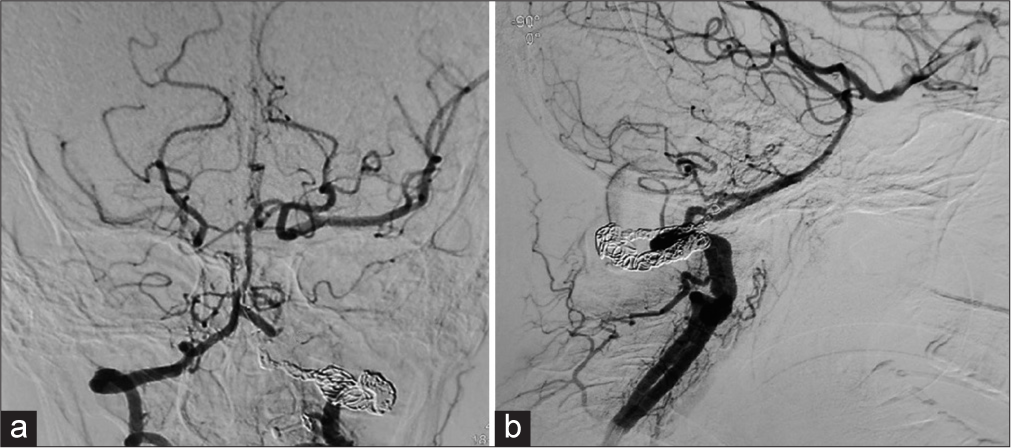
- (a and b) Bilateral simultaneous vertebral angiography s/o optimum proximal and distal occlusion of aneurysm and fistula.
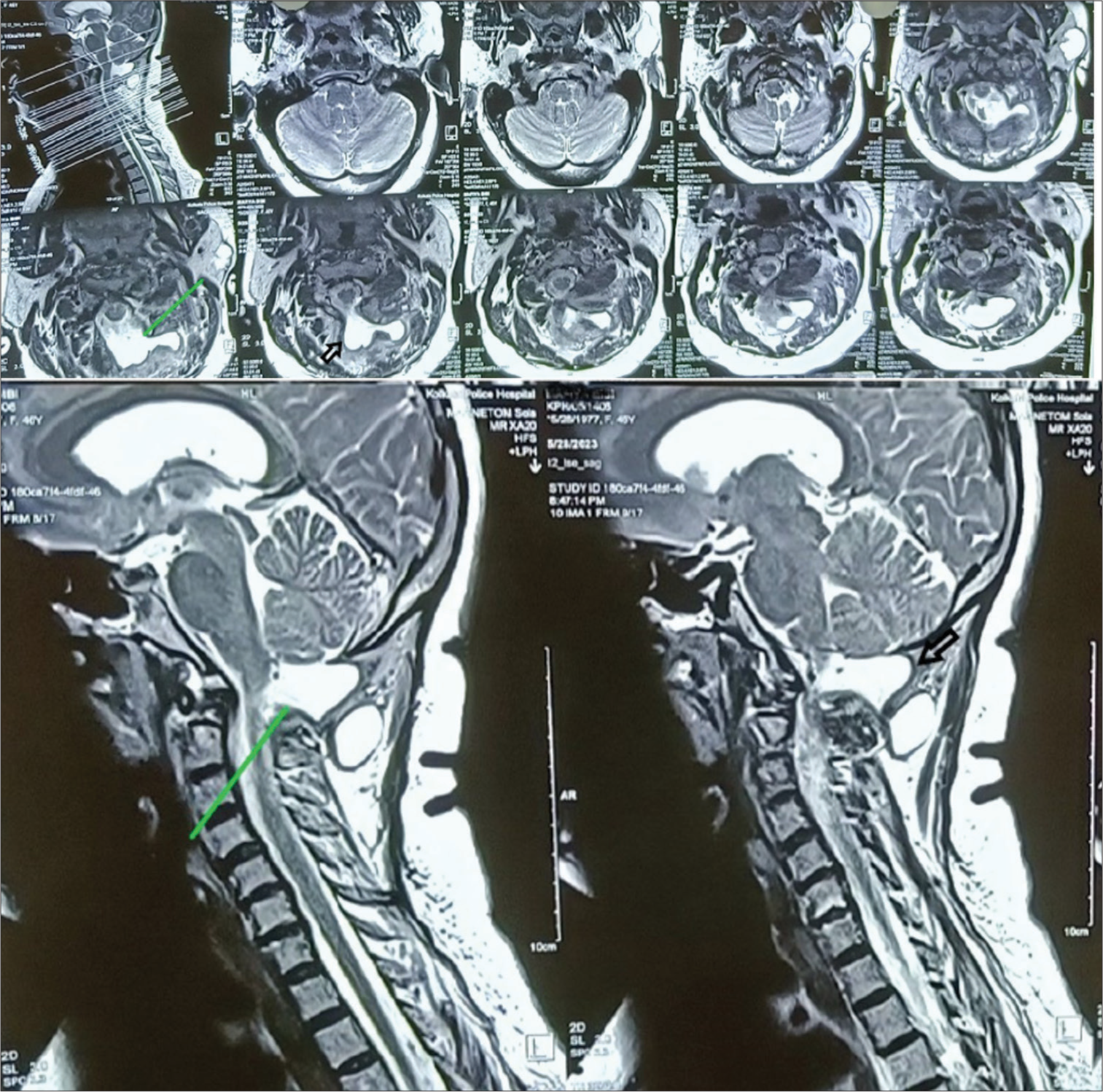
- Post-operative images (after 8 weeks) T2W2 axial and sagittal view of magnetic resonance imaging brain and cervical cuts s/o pseudomeningocele formation (green and black arrow) and complete obliteration of venous pouch.
Depending on the scope and severity of the initial artery wall injury, traumatic aneurysms can be true, false, mixed, or dissecting in nature.[4] The primary dynamic force is blunt or penetrating injury, and the mechanism is intimately tied to the anatomic location of the injured blood vessel and the complex structures around it. Anatomically, the vertebral artery may be split into the V1, V2, V3, and V4 segments. The proximal segment of the vertebral artery (V1, V2, and V3) is relatively accessible for surgical interventions. The V4 segment, which is intracerebral, is the most challenging to assess[5] and is typically managed using endovascular techniques. The vertebral artery pseudoaneurysm has a varied natural history. An aneurysm that has formed as a result of trauma often ruptures within 2–3 weeks. The mortality and morbidity rates for traumatic cerebral aneurysms are significant[6] Such lesions must have an early diagnosis and prompt intervention.[7] The handshake technique was required because of the extremely high flow that kept displacing the coils away from either side or a balloon in the proximal vertebral artery failed to achieve flow arrest. Hence, both catheters crossed each other and repeated deployment of enmeshed coils from both catheters was required to keep the coil mass in place.[7] The anterior spinal artery and radiculomedullary with muscular branches of the vertebral artery were preserved.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as patients identity was not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Potentially fatal nature of traumatic vertebral artery pseudoaneurysms. J Vasc Med. 2022;10:123-36.
- [Google Scholar]
- Difficulties encountered during the coiling technique for distal vertebral artery pseudoaneurysms. J Interv Radiol. 2023;15:78-92.
- [Google Scholar]
- Pseudoaneurysm of the vertebral artery with V-J fistula: A rare presentation. J Clin Neurosci. 2019;68:1-3.
- [Google Scholar]
- Traumatic vertebral artery pseudoaneurysms: A review of the literature and proposal for a management algorithm. J Neurosurg Pediatr. 2019;33:264-73.
- [Google Scholar]
- Traumatic vertebral artery pseudoaneurysm: A review of management strategies. J Neurosurg Pediatr. 2021;37:25-31.
- [Google Scholar]
- Traumatic vertebral artery pseudoaneurysm: A comprehensive review of diagnosis and management. J Neurointerv Surg. 2020;12:1-12.
- [Google Scholar]
- Endovascular treatment of a giant basilar tip aneurysm with extremely high flow: A case report and review of the literature. Chin Med J. 2011;124:1737-42.
- [Google Scholar]






