Translate this page into:
Dissecting aneurysm of the posterior cerebral artery: Defining the role of deliberate surgical proximal artery occlusion
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Posterior cerebral artery (PCA) aneurysms are rare and account for less than 1% among all intracranial aneurysms.[123] They may be either saccular or dissecting.[1] Dissecting aneurysms are more common in the posterior circulation.[4] A 36-year-old normotensive lady presented with exacerbation of headache (present over 1 month), vomiting and drowsiness over the last 24 hours. She was opening eyes on pain, was localizing with both upper limbs and was groaning. She had right sided hemiparesis with right extensor plantar. Computed tomography (CT) scan [Figure 1a] showed left PCA territory infarct with intraventricular hemorrhage and left medial temporal bleed with effaced cisterns, cortical sulci and ipsilateral lateral ventricle and a 5 mm midline shift. 3D CT angiography [Figure 2a] showed a large upwardly and posteriorly directed aneurysm from the left P2-P3 junction. The distal PCA was not seen. Left temporal decompressive craniotomy, subtemporal approach and deliberate surgical parent artery occlusion (PAO) i.e. clipping the PCA proximal to the aneurysm and distal to the recurrent brain stem and superiorly directed branches from the P2 in the ambient cistern was done with partial removal of the left temporal clot. Postoperative CT scan [Figure 1b] showed subgaleal CSF, near complete removal of clot and left PCA territory infarct. Postoperative period was uneventful except for right homonymous hemianopia. Six months later cranioplasty was done after a CT angiogram [Figure 2b] which showed no residual aneurysm.

- Axial CT (computed tomography) images showing (a) pre-operative left occipital infarct, intraventricular bleed, left medial temporal bleed, with effacement of the cisterns, cortical sulci and ipsilateral lateral ventricle and (b) postoperative established infarct, clip in situ and opening up of cisterns and ventricles and decrease of mass effect
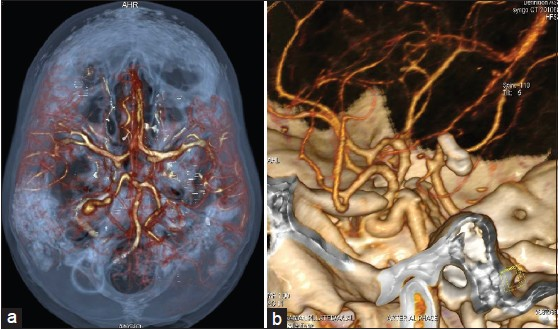
- CT angiogram showing (a) P2-P3 junction dissecting aneurysm projecting posterosuperiorly into the brain substance. The lesion is elongated and shows stenosis followed by dilatation and (b) postoperative successful vessel occlusion by the clip with no distal flow in the vessel and no proximal reformation of neck
Intracranial dissections occur between the intima and media as opposed to extracranial dissections occurring between the media and adventitia.[5] This results in the typical angiographic features of narrowing followed by ballooning (as in our case) or of complete stenosis. Though mostly idiopathic, predisposing factors like migraine, fibromuscular dysplasia, connective tissue disorders and trauma[235] (causing shearing of the PCA along the free margin of the tentorium[2] ) are associated with dissections. Unlike extracranial dissections, hypertension in not a risk factor.[5] Our patient, too, was normotensive. Further, like in our case, isolated PCA dissections have a female predilection[345] unlike vertebrobasilar dissections that are more common in males. The most common presenting symptom of PCA dissection is occipital headache. Aneurysm rupture can present with subarachnoid hemorrhage (SAH) and less commonly, cerebral ischemia or infarction.[3] Our patient had occipital lobe infarction, SAH and intracerebral and intraventricular hemorrhage as well. The natural history of ruptured intracranial dissecting aneurysms is reportedly unfavorable with rebleeding rates of 30%-71%,[4] hence necessitating treatment. While anticoagulation (as for extracranial dissections) has been advocated by some authors,[5] the majority favor occlusion via the endovascular route[123467] as this location is difficult to access surgically with numerous perforators in the vicinity.[12] When these aneurysms are located distally, embolization of the lesion alone sparing the vessel has been highlighted as being technically difficult[46] and PAO by coil or glue is well tolerated due to good collateral supply.[67] The possible surgical strategies that can be used to treat dissecting aneurysms of PCA are trapping, excision, clipping, wrapping and deliberate PAO as well. Honda et al.[8] mention that approximately 20% of PCA aneurysms may require trapping or PAO (especially larger ones and those in the P2-P3 regions of the PCA). Taqi et al.[3] have reported four cases of dissecting PCA aneurysms from three different authors three of which underwent proximal clipping with vessel occlusion and one underwent trapping. In this case, due to the configuration and distal location of the aneurysm in the posterior circulation, it was probable that dissection was the etiology. In our case, we opted to go for a surgical intervention since our patient presented with both infarct and intracerebral hematoma causing mass effect and midline shift decompression of which would not be achieved by the endovascular route alone . As the observed neck in dissecting aneurysms may not represent the point of maximal weakness of the vessel wall (which may be more proximal i.e. at the site of intimal tear), clipping the neck alone does not rule out reformation of another aneurysm proximally. Hence, deliberate surgical PAO distal to all brain stem feeders was chosen. Furthermore, our patient already had an established occipital infarct and hence fresh deficits would not develop even if collaterals failed to maintain supply to the PCA territory after PAO. To conclude, surgical PAO in dissecting posterior circulation aneurysms has a definite role if the aneurysm is distal, if done in patients with an established infarct and where reduction of raised intracranial pressure is a priority.
References
- Endovascular treatments for distal posterior artery aneurysms. Turk Neurosurg. 2012;22:141-7.
- [Google Scholar]
- Deliberate parent artery occlusion for non-saccular posterior cerebral artery aneurysms. Interv Neuroradiol. 2011;17:159-68.
- [Google Scholar]
- Dissecting aneurysms of posterior cerebral artery: Clinical presentation, angiographic findings, treatment, and outcome. Front Neurol. 2011;2:38.
- [Google Scholar]
- Ruptured dissecting aneurysms arising from non-vertebral arteries of the posterior circulation: Endovascular treatment perspective. Diagn Interv Radiol. 2009;15:159-65.
- [Google Scholar]
- Isolated posterior cerebral artery dissection: Report of three cases. AJNR Am J Neuroradiol. 2006;27:648-52.
- [Google Scholar]
- Parent artery occlusion for intracranial aneurysms. Interv Neuroradiol. 2009;15:309-15.
- [Google Scholar]
- Endovascular treatment of posterior cerebral artery aneurysms. AJNR Am J Neuroradiol. 2006;27:300-5.
- [Google Scholar]
- Aneurysms of the posterior cerebral artery; Retrospective review of surgical treatment. Neurol Med Chir (Tokyo). 2004;44:164-9.
- [Google Scholar]





