Translate this page into:
Differentiating colloid cyst from intraventricular cysticercus: Case of a ventricular cyst in a patient with neurocysticercosis
Address for correspondence: Dr. Dale Ding, Department of Neurological Surgery, University of Virginia, PO Box 800212, Charlottesville, Virginia - 22908, United States. E-mail: dmd7q@hscmail.mcc.virginia.edu
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
We present a patient with intraparenchymal neurocysticercosis and an anterior third ventricular mass believed to be a colloid cyst. We elected to surgically evacuate the parenchymal cysticercus lesion and conservatively follow the third ventricular cyst which remained stable on repeat neuroimaging at a time interval of 3 months.
A 22-year-old female immigrant from Honduras presented with headache and seizures. Brain CT and MRI [Figure 1a–f] demonstrated an enhancing right frontal lesion with perilesional edema and a non-enhancing lesion in the midline anterior third ventricle without evidence of hydrocephalus. Since we believed the intraparenchymal lesion was causing the patient's seizures, a craniotomy was performed to resect the right frontal lesion which was identified on histopathology to be neurocysticercosis. The patient was treated with an antiepileptic and a short course of steroids without antiparasitic therapy given the slight but undeniable risk of ventriculitis if the intraventricular lesion was a cysticercus. At 3 months follow-up the patient remained neurologically intact without further headaches or seizures and brain MRI showed unchanged appearance of the presumed colloid cyst without evidence of residual right frontal abscess [Figure 1g–j]. CSF and serum analysis for neurocysticercosis were negative at last follow-up. We are currently monitoring the patient with serial neuroimaging.
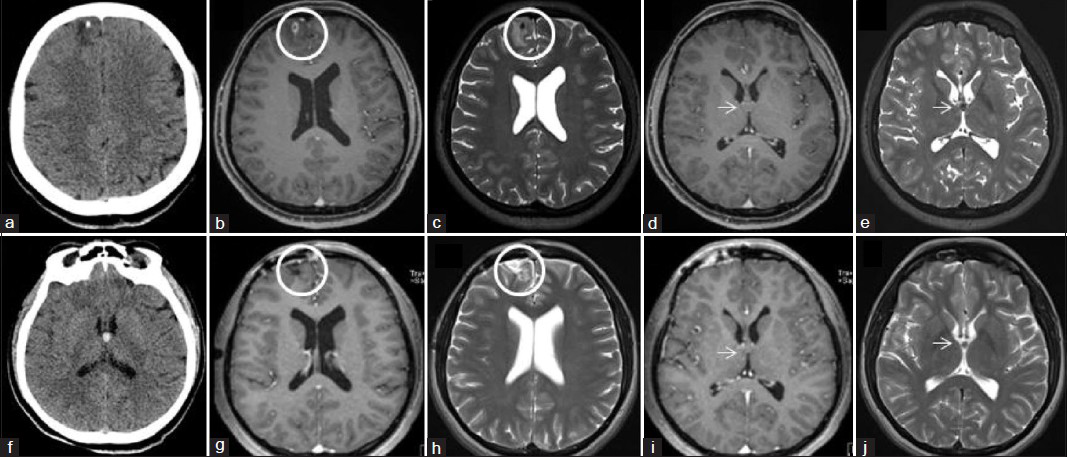
- (a) Non-contrast brain CT, axial section, showing a hypodense lesion with a small focus of calcification in the right frontal lobe. This is neurocysticercosis, and the calcified focus represents the scolex of the cysticercus. Brain MRI (b) T1-weighted post-contrast and (c) T2-weighted, axial sections at the level of the right frontal intraparenchymal neurocysticercosis lesion shows a ring-enhancing mass, measuring 6 × 7 mm in size, with perilesional edema in the surrounding anterior medial frontal lobe (circle). Brain MRI (d) T1-weighted post-contrast and (e) T2-weighted, axial sections at the level of the anterior third ventricular lesion shows a non-enhancing mass most consistent with a colloid cyst (arrow). (f) Non-contrast brain CT, axial section, showing a hyperdense lesion in the anterior third ventricle without evidence of obstructive hydrocephalus. This is the typical appearance of a colloid cyst on CT. Post-operative brain MRI performed 3 months following craniotomy for resection of the right frontal cysticercus. (g) T1-weighted post-contrast and (h) T2-weighted axial sections at the level of the evacuated neurocysticercosis lesion shows post-operative changes of a craniotomy without evidence of residual or recurrent infection (circle). (i) T1-weighted post-contrast and (j) T2-weighted axial sections at the level of the third ventricular lesion shows unchanged appearance of the mass presumed to be a colloid cyst (arrow).
Neurocysticercosis is the most common parasitic infection of the central nervous system, affecting the ventricular system in 15-54% of cases.[1] Intraventricular neurocysticercosis of the third ventricle may be difficult to distinguish from a colloid cyst.[234] Medical treatment of intraventricular neurocysticercosis is dangerous without CSF diversion as treatment-induced cyst rupture may result in florid parasitic ventriculitis. While the third ventricular lesion in this case was most likely a colloid cyst based on its neuroimaging characteristics, we could not absolutely rule out neurocysticercosis without surgical extirpation. The lack of hydrocephalus would have favored a transcallosal over a neuroendoscopic approach.[5] We decided the risk of morbidity associated with a transcallosal cyst resection was too high given its likely incidental nature. This is the first reported case of a colloid cyst in the setting of neurocysticercosis.
References
- Intraventricular neurocysticercosis: A review of current status and management issues. Br J Neurosurg. 2012;26:305-9.
- [Google Scholar]
- Intraventricular neurocysticercosis mimicking colloid cyst. Case report. J Neurosurg. 2002;97:208-10.
- [Google Scholar]
- Third ventricular cysticercal cyst mimicking a colloid cyst: Case report. Neurosurgery. 1996;39:623.
- [Google Scholar]
- Migratory neurocysticercosis mimicking a third ventricular colloid cyst. Case report. J Neurosurg. 2001;95:122-3.
- [Google Scholar]
- Treatment options for third ventricular colloid cysts: Comparison of open microsurgical versus endoscopic resection. Neurosurgery. 2008;62(Suppl 3):1076-83.
- [Google Scholar]





