Translate this page into:
Diabetic striatopathy in a child with type 1 diabetes mellitus
*Corresponding author: Arvinder Wander, Department of Pediatrics, All India Institute of Medical Sciences, Bathinda, Punjab, India. wander1686@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh R, Roshwanth A, Gaddigoudar M, Anuhya CB, Wander A. Diabetic striatopathy in a child with type 1 diabetes mellitus. J Neurosci Rural Pract. 2025;16:139-40. doi: 10.25259/JNRP_369_2024
A 12-year-old girl, who was a diagnosed case of type 1 diabetes mellitus for the past two years, presented with irregular uncontrolled involuntary movements of her bilateral arms for the past two weeks [Video]. She was having poor compliance with the insulin therapy and often lost to follow-up. There was a history of previous admission due to diabetic ketoacidosis one year back. Her blood sugar level was 365 mg/dL, and HbA1c was 12 at presentation. Urine was positive for sugar but negative for ketones. Based on the clinical history and examination, the diagnosis of chorea was made, thus magnetic resonance imaging (MRI) brain was done to search for the possible cause. The MRI brain revealed asymmetrical T1 hyperintensity [Figure 1] in bilateral (left > right) basal ganglia. No blooming/diffusion restriction was seen. The MRI brain findings were consistent with diabetic striatopathy. Her symptoms resolved after normalization of the blood glucose confirming the diagnosis of diabetic striatopathy.
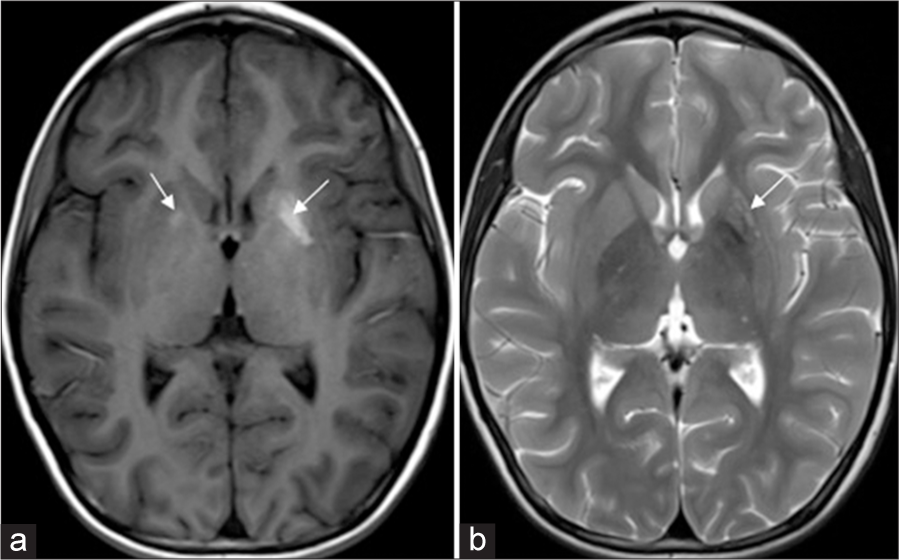
- (a) T1-weighted axial image showing hyperintensity in bilateral basal ganglia, more on the left side (arrows). (b) Corresponding T2-weighted axial image showing heterogeneous mixed signal in the left basal ganglia (arrow).
Diabetic striatopathy, also called hyperglycemic hemiballism/hemichorea, is most frequent in older individuals with type 2 diabetes and has been rarely reported in type 1 diabetic patients.[1,2] On non-contrast computed tomography (NCCT), these basal ganglia abnormalities appear as hyperdense, which could lead to false interpretation and mislead the clinician towards an erroneous diagnosis of cerebral hemorrhage. T1 hyperintensity, a hallmark radiological feature, has been attributed to gemistocyte accumulation and neuronal loss.[3] Clinical symptoms are reversible with timely management of hyperglycemia; however, some patients may require neuroleptic drugs for abnormal movements. In case of disabling involuntary movements, deep brain stimulation may be beneficial.[4] Cerebral microhemorrhages can also be seen in such patients, which are contributed by hyperglycemia-induced vasculopathy.[5] Imaging findings return to baseline more slowly than the clinical symptoms.
While movement disorders are not uncommon in the pediatric age group, treatable cases are rare. The condition described in the index case is seldom reported in children. Timely diagnosis of the underlying cause, along with managing the primary illness, not only treats the disorder but also prevents future complications.
Ethical approval:
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Diabetic striatopathy: A new challenge in type 1 pediatric diabetic patients. Oman Med J. 2022;37:e332.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic striatopathy in type 1 diabetes mellitus: A rare conundrum. BMJ Case Rep. 2023;16:e257448.
- [CrossRef] [PubMed] [Google Scholar]
- “Diabetic striatopathy”: Clinical presentations, controversy, pathogenesis, treatments, and outcomes. Sci Rep. 2020;10:1594.
- [CrossRef] [PubMed] [Google Scholar]
- Teaching neuroimage: Basal ganglia T1 hyperintensity and SWI signal diabetic striatopathy in an 18-year-old man with type 1 diabetes mellitus. Neurology. 2021;97:e2148-9.
- [CrossRef] [PubMed] [Google Scholar]
- Concepts and controversies in nonketotic hyperglycemia-induced hemichorea: Further evidence from susceptibility-weighted MR imaging. J Magn Reson Imaging. 2009;29:699-703.
- [CrossRef] [PubMed] [Google Scholar]





