Translate this page into:
Delirium Research in India: A Systematic Review
Sandeep Grover, MD Department of Psychiatry, Postgraduate Institute of Medical Education and Research Chandigarh 160012 India drsandeepg2002@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Delirium is the most common psychiatric diagnoses encountered in patients with various medical-surgical illnesses, in all the treatment set-ups, with relatively higher incidence and prevalence in the intensive care units. As delirium is encountered in multiple specialties, it is important to understand the research on this diagnosis. This study aims to assess the research output involving patients of delirium from India. A comprehensive search was undertaken using Medline (PubMed) and other databases. Search words included were “delirium,” “delirious,” “delirium tremens” AND “India.” No filters were used. Internet and hand searches yielded 305 articles. Out of these articles, 151 had the terms “delirium,” “delirious,” “delirium tremens” in the title and these were included for the review. Additionally, 14 articles were included for the review, although these did not have these terms in the title, but delirium was one of the major outcome parameters in these studies. Majority of the papers were original articles (n = 81), and these were followed by, case reports (n = 58), review articles (n = 10), letter to the editor (not as case reports but as a communication; n = 13), editorials (n = 2) and one clinical practice guideline. Most of the original papers have either focused on epidemiology (incidence, prevalence, outcome, etc.), symptom profile, with occasional studies focusing on effectiveness of various pharmacological interventions. There is a dearth of research in the field of delirium from India. There is a lack of studies on biomarkers, evaluation of nonpharmacological interventions, and evaluation of prevention strategies. It is the need of the hour to carry out more studies to further our understanding of delirium in the Indian context.
Keywords
delirium
India
outcome
Introduction
Delirium is an acute medical emergency, with psychiatric manifestations, which is seen across different treatment settings, with higher prevalence in intensive care units (ICUs) and palliative care setting. It is characterized by poor attention, disturbances in other cognitive functions, motoric alteration, disturbance in sleep, and psychotic symptoms. The prevalence of delirium varies across different settings, with rates as high as 80% among patients admitted in intensive care units (ICUs) and palliative care setting.1 From an organ failure point of view, delirium represents acute brain failure, occurring due to various causes.2 3 The various contributing factors for delirium can be broadly categorized as risk or predisposing and the precipitating or etiological factors.4 It is the combination of the risk and the precipitating factors which determine the manifestation of delirium.5 Patients, who are at high risk, may require minor precipitating factors for the development of delirium, whereas those who have lower risk factors may require more or severe precipitating factors for the development of delirium.5 As a disorder, delirium is associated with significant negative consequences for the patients and their families in terms of increased mortality, longer duration of ICU and inpatient stay, higher treatment cost, long-term cognitive deficits, a higher risk of developing dementia, and high level of distress to the patients and caregivers.6
Although it is seen across all the medical-surgical settings, it is often underrecognized and undertreated. Some of the developed countries have recognized the importance of early identification and prevention of delirium in various treatment settings.7 8 Many authors have developed bedside assessment instruments to detect delirium at the earliest and have also developed various intervention packages, such as the Hospital Elder Life Program (HELP)9 and Assess, Prevent, and Manage Pain, Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT); choice of analgesia and sedation; and the Delirium: Assess, Prevent, and Manage Early mobility and Exercise, and Family engagement and empowerment (ABCDEF)10 bundle for early detection, prevention, and management of delirium.
Considering its ubiquitousness across all clinical specialties and underrecognition, it is important to understand awareness about delirium. One of the ways to address the issue is to look at the research outcome on the topic. Till today, there is no systematic review focusing on the research output on delirium from India. Evaluating the research output can help in understanding the current level of research and deficits in research. This can help in planning future research on the topic. Accordingly, this systematic review attempted to evaluate the research on delirium from India.
Methodology
For this systematic review, literature was searched in various search engines, that is, PubMed and Google Scholar, by using the following terms: “delirium,” “delirious,” “delirium tremens,” “India,” and “organic brain syndrome” in different combinations in December 2019. No filters were used. Additional searches were performed by doing hand searches of the reference list of the published articles to identify more articles. Additionally, the table of content of online issues of various psychiatric and anesthesia journals (irrespective of the indexing status) published from India, were specifically searched for studies focusing on delirium.
To be included in the review, the published papers were required to have the words “delirium,” “delirious,” or “delirium tremens” in the title. However, if the studies did not include these terms in the title but the primary focus of the study was delirium, then these papers were included in the review. Studies describing the psychiatric referral pattern, but which did not focus on the delirium, but in general described the prevalence of delirium in psychiatric referrals, were excluded. Data published only as abstracts of the national conferences were also excluded.
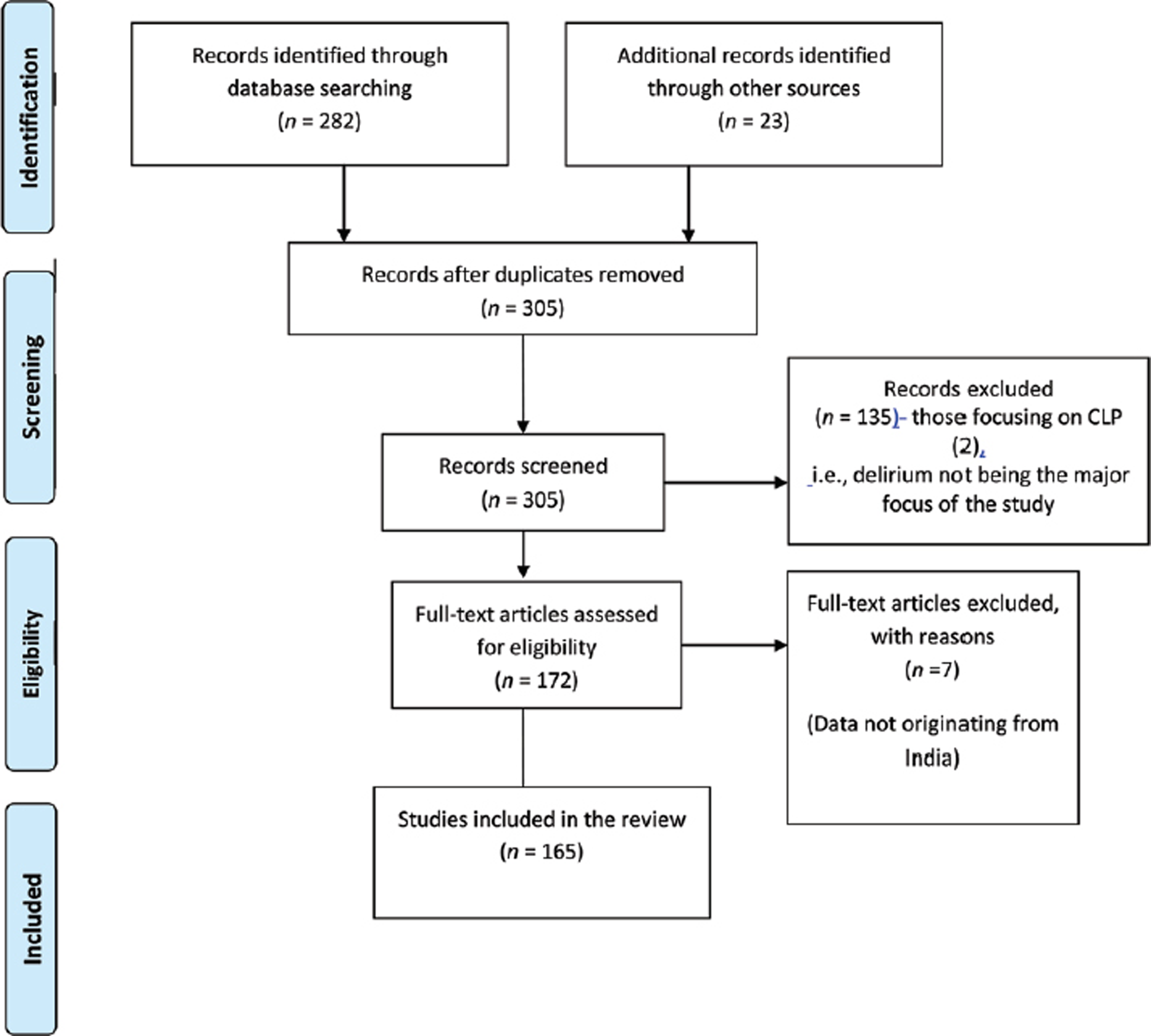
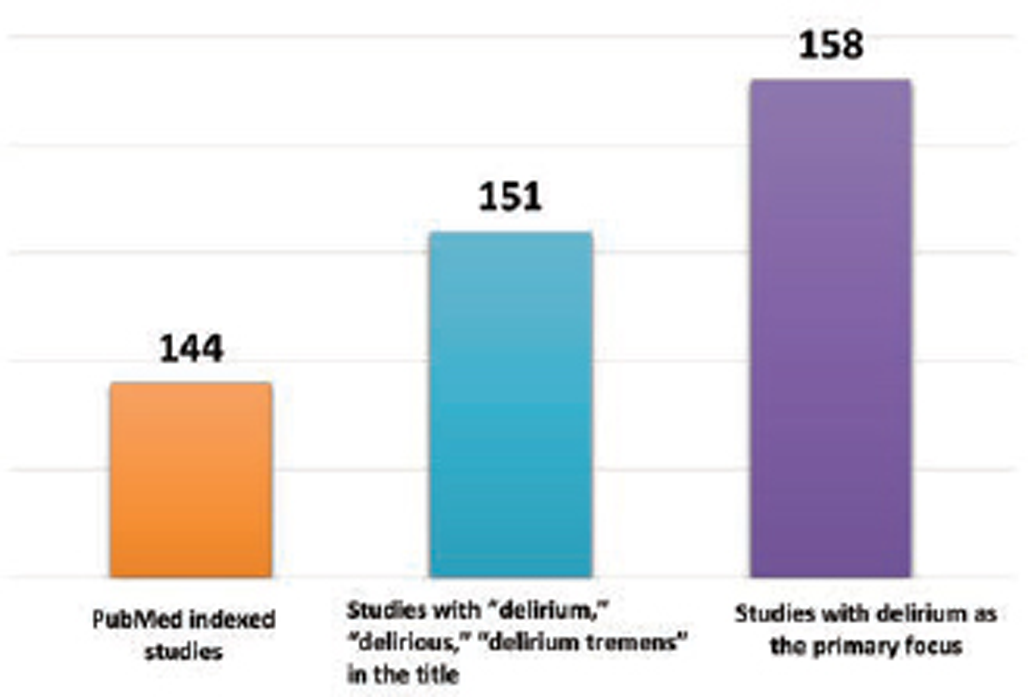
Internet and hand searches yielded 305 articles. Fig. 1 shows the selection of the articles. Full manuscripts of these articles were reviewed by D.D. and S.K. Out of these articles, 151 had the terms “delirium,” “delirious,” “delirium tremens” in the title and these were included for the review (Fig. 2). Additionally, 14 articles were included for the review, although these did not have these terms in the title but had delirium as one of the major outcome parameters. A majority (n = 144; 87.3%) of these articles were available in the PubMed search (Fig. 2).
-
Fig. 1 PRISMA diagram showing selection of studies. PRISMA, preferred reporting items for systematic reviews and meta-analyses.
Fig. 1 PRISMA diagram showing selection of studies. PRISMA, preferred reporting items for systematic reviews and meta-analyses.
-
Fig. 2 Number of articles in PubMed search, having the word delirium and related terms in the title, and studies with delirium being the primary focus of the study.
Fig. 2 Number of articles in PubMed search, having the word delirium and related terms in the title, and studies with delirium being the primary focus of the study.
Results
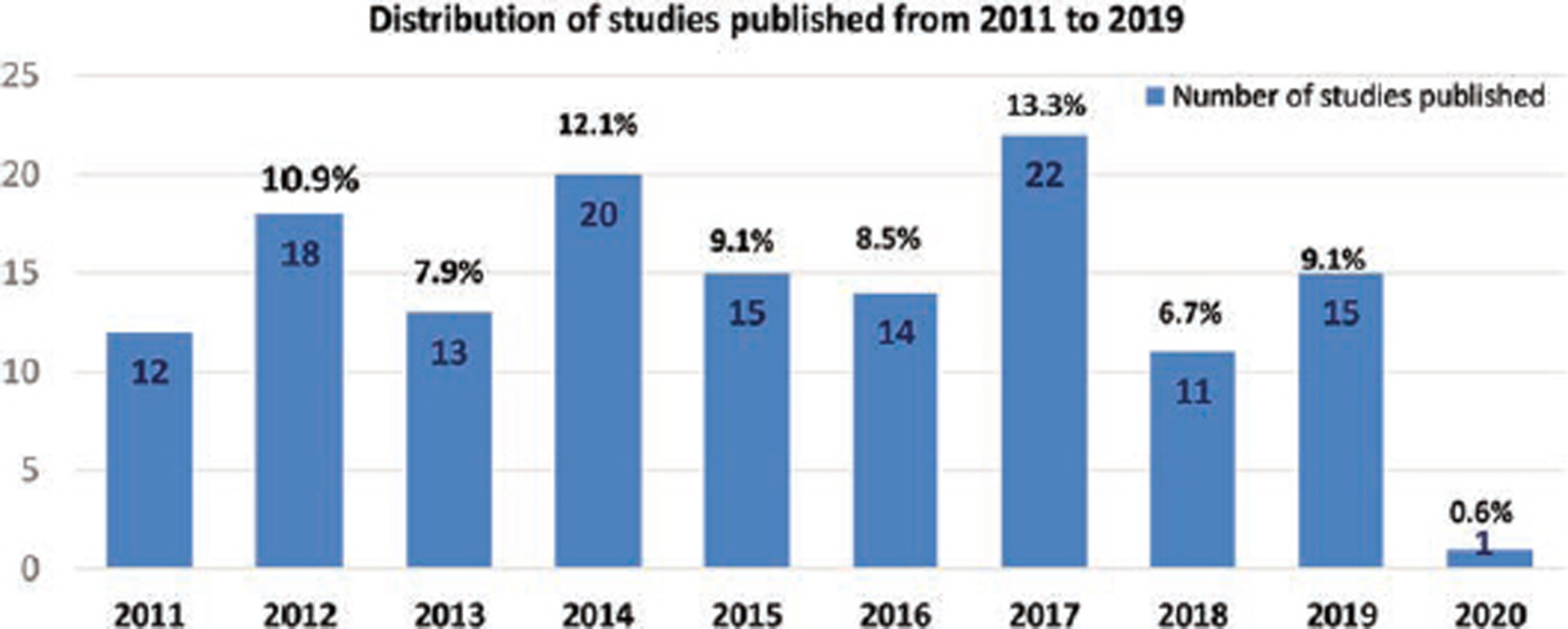
Out of the 165 articles, it was seen that the majority (85.5%, n = 141) of the papers were published in the last one decade (2011–2019), and this was followed by 23(13.9%) articles published during the year 2001 to 2010. There was only one article (0.6%) on delirium before 2001, arising from India. Again, in the years 2011 to 2019, there were at least 10 articles published every year (Fig. 3). A majority (87.3%) of the articles were published in the PubMed indexed journals and about one-third (31.5%) of these articles had nonpsychiatrist as an author. In terms of the type of papers, majority of the papers were original articles (n = 81, one of which was in the form of a letter to the editor),11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 and these were followed by, case reports (n = 58),92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 review articles (n = 10),4 150 151 152 153 154 155 156 157 158 letter to the editor (not as case reports but as a communication; n = 13),81 159 160 161 162 163 164 165 166 167 168 169 170 editorials (n = 2),171 172 and one clinical practice guideline.173 In terms of the institutes, most (37.6%, n = 62) of the articles were from the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, and this was followed by National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru (n = 6).
-
Fig. 3 Number of articles published in each year in last one decade.
Fig. 3 Number of articles published in each year in last one decade.
In terms of the original paper, out of the 81 papers, a majority (n = 50; 61.7%) of these were published in journals published from outside India. About two-fifths (n = 33; 40.7%) of the original articles had nonpsychiatrists as an author and about one-fourth (n = 19; 23.5%) of these studies focused on ICU patients or ICU health care workers.
As across the globe, the prevalence and incidence of delirium, in studies from India have also varied depending on the study setting (Table 1).11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 Majority of the studies have assessed the incidence and prevalence of delirium have relied on the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV)/DSM-IV text revision (TR) criteria.15 17 19 20 23 24 25 26 27 29 30 31 However, some of the studies have used confusion assessment method (CAM)/CAM-ICU.13 14 16 18 33 34 The prevalence rates in various ICUs have varied from 16.1 to 68.2%.15 16 17 19 20 23 Similarly, the incidence of delirium in various ICUs ranges from 8 to 59.6%.15 17 18 19 20 21 22
|
Study (year) |
Treatment setting |
Diagnostic system used |
Sample size |
Prevalence |
Incidence |
Inpatient mortality |
Mortality at follow-up |
|---|---|---|---|---|---|---|---|
|
Abbreviations: AWD, alcohol withdrawal delirium; CAM, confusion assessment method; CAP, children and adolescents; CLP, consultation liaison psychiatry; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, fourth edition; DSM-IV TR, DSM-IV text revision; F/U, follow-up; ICD, International Classification of Disease; ICU, intensive care unit; PAED, pediatric anesthesia emergency department. aPrevalence of delirium in psychiatric referrals. bInpatient mortality rate of patients not referred to CLP services for delirium. |
|||||||
|
Inpatient setting |
|||||||
|
Khurana et al (2002)11 |
General medical inpatients |
ICD-10 |
100, elderly |
19% |
8% |
||
|
Grover et al (2009)12 |
Inpatient |
ICD-10 |
238,777 3,092a |
0.44% 33.96%a |
6.6%a |
||
|
Rai et al (2014)13 |
Neurology inpatient |
CAM |
52 |
34.6% (1–3 months of F/U) |
|||
|
Khurana et al (2011)14 |
Inpatient, elderly |
CAM |
400 |
27.47% |
14.75% |
||
|
ICU setting |
|||||||
|
Grover et al (2018)15 |
ICU |
DSM-IVTR |
66 |
68.2% |
59.6% |
||
|
Kumar et al (2016)16 |
ICU |
CAM-ICU |
31 |
16.1% |
– |
– |
|
|
Grover et al (2014)17 |
CCU |
DSM-IVTR |
152 elderly |
24.34% |
13.4% |
19.2% |
|
|
Jayaswal et al (2019)18 |
Medical ICU |
CAM-ICU RASS |
280 |
31.4% |
9.9% |
15.9 (1-month F/U) |
|
|
Sharma et al (2012)19 |
RICU |
DSM-IV |
140 |
53.6% |
24.4% |
30.7% |
|
|
Lahariya et al (2014)20 |
CCU |
DSM-IV |
309 |
18.7% |
9.3% |
27% |
|
|
Bamalwa et al (2016)21 |
Cardiac ICU |
50 |
16% |
||||
|
Shyamsundar et al (2009)22 |
Medical/cardiac ICU |
120 |
10.3% |
||||
|
Barman et al (2018)23 |
Multidisciplinary ICU |
DSM-IVTR |
310 |
45% |
|||
|
Consultation liaison setting |
|||||||
|
Grover et al (2013)24 |
CLP |
DSM-IV TR |
331 |
– |
– |
12.4% |
|
|
Grover et al (2014)25 |
CLP |
DSM-IVTR |
49, CAP |
10% |
|||
|
Grover et al (2019)26 |
CLP |
DSM-IVTR |
103 |
10.7% |
|||
|
Grover et al (2012)27 |
CLP |
DSM-IVTR |
97 |
12.1% 6.79%b |
27.83% (6 months of F/U) |
||
|
Grover et al (2012)28 |
CLP |
ICD-10 |
109, elderly |
16.5% |
|||
|
Grover et al (2014)29 |
CLP |
DSM-IV TR |
321 |
10.3% |
|||
|
Grover et al (2013)30 |
CLP, AWD |
DSM-IVTR |
112 |
13.4% |
|||
|
Grover et al (2016)31 |
CLP, AWD |
DSM-IVTR |
112 |
13.4% |
|||
|
Surgery and postoperative setting |
|||||||
|
Dhakharia et al (2017)32 |
Postoperative setting |
824 |
4% |
||||
|
Kumar et al (2017)33 |
Postoperative (cardiac surgery) |
CAM-ICU |
17.5% |
||||
|
Chrispal et al (2010)34 |
Delirium in patient undergoing hip fractures surgery |
CAM |
81 |
21% |
|||
|
Miscellaneous |
|||||||
|
Khanna et al (2018)35 |
Pediatric patients undergoing ophthalmic examination under sevoflurane |
PAED scale |
100 |
24% |
|||
|
Sethi et al (2013)36 |
Pediatric patients undergoing cataract surgery under sevoflurane and desflurane |
PAED scale |
88 |
18.18% in the sevoflurane group 20.45% in the desflurane group |
|||
One of the studies evaluated delirium in general medical inpatients and reported the prevalence rate to be 19%,11 whereas another study that focused on postoperative patients reported a prevalence rate of 4%.32 One study reported a prevalence of delirium in referrals of consultation liaison psychiatry (CLP) setting and estimated the prevalence to be 33.96%.12 The same study extrapolated the prevalence to all the inpatients and estimated the prevalence to be 0.44%.12 However, this could be an underestimation, as many patients who develop delirium are not referred to the CLP services.
Studies have also reported the inpatient mortality rates for patients with delirium and the same has varied from 6.6 to 30.7%.12 14 17 18 19 20 24 25 26 27 28 29 30 31 However, only occasional studies have compared the mortality data with all the inpatients, who did not develop delirium. One of the studies reported that the inpatient mortality rate for patients with delirium was 12.1% and was higher compared with those patients who were not referred to the CLP services for delirium.27 Occasional studies have reported long-term mortality in patients of delirium, after 1 to 6 months of inpatient care and the rates have varied from 15.9 to 34.6%.13 18 27
A total of 23 studies (Table 2)15 24 25 26 27 28 29 31 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 have evaluated the symptom profile of delirium and most of these studies have relied on the Delirium Rating Scale Revised-1998 (DRS-R-98). The majority of these studies have focused on patients seen by CLP services, with occasional studies focusing on ICU patients. Some of the studies have also specifically focused on children,25 49 elderly,37 41 44 46 and those with alcohol-withdrawal delirium (AWD).31 In general, these studies suggest that disturbance in attention, disorientation, and other cognitive functions are present in a majority of the patients. In terms of specific items of DRS-R-98, studies that have been done in CLP setting, in general, report higher frequency of motor agitation, whereas studies in ICUs suggest a higher frequency of motor retardation. The studies which have compared people of different age groups suggest that there are minor variation in the symptom profile of delirium in children, adult, and elderly.25,37,41,44,46,49
|
Study (year) |
Sample size and setting |
Sleep–wake cycle disturbances |
Perceptual disturbance |
Delusions |
Lability of affect |
Language |
Thought process abnormality |
Motor agitation |
Motor retardation |
Disorientation |
Attention deficits |
Short-term memory |
Long-term memory |
Visuospatial ability |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Abbreviations: AWD, alcohol withdrawal delirium; CAP, children and adolescents; CCU, coronary care unit; CLP, consultation liaison psychiatry services; ICU, multispecialty intensive care unit; RICU, respiratory ICU. |
||||||||||||||
|
Grover et al (2012)28 |
151, CLP |
100 |
76.2 |
27.8 |
77.5 |
76.8 |
69.5 |
94 |
39.1 |
100 |
100 |
97.4 |
93.4 |
96.7 |
|
Grover et al (2011)37 |
109, CLP, elderly |
97.2 |
78.9 |
35.8 |
62.4 |
79.8 |
74.3 |
89.0 |
32.1 |
95.4 |
97.2 |
91.8 |
65.1 |
63.3 |
|
Jain et al (2011)38 |
86, CLP |
100 |
76.7 |
37.2 |
59.3 |
73.3 |
89.5 |
89.5 |
31.4 |
100 |
97.7 |
97.7 |
40.7 |
98.8 |
|
Mattoo et al (2012)39 |
100, CLP |
99 |
35 |
14 |
94 |
90 |
92 |
94 |
9 |
100 |
100 |
91 |
97 |
93 |
|
Arya et al (2013)40 |
84, CLP |
100 |
80.9 |
60.7 |
94 |
92.8 |
76.2 |
86.9 |
53.6 |
98.8 |
98.8 |
97.6 |
48.8 |
76.2 |
|
Grover et al (2012)27 |
97, CLP |
96.7 |
80 |
33.3 |
90 |
73.3 |
73.3 |
93.3 |
33.3 |
100 |
100 |
93.3 |
53.3 |
60 |
|
Grover et al (2014 and 2013)29,41 |
321 CLP, adult vs. elderly |
98.1 |
79.4 |
45.2 |
85.7 |
87.5 |
84.7 |
90.3 |
50.8 |
98.8 |
99.7 |
95.6 |
52.6 |
63.2 |
|
Grover et al (2016)31 |
112, CLP, AWD |
100 |
75 |
48.2 |
87 |
85.7 |
87 |
94.6 |
25 |
99.1 |
100 |
92.9 |
65.2 |
68.8 |
|
Sharma et al (2017)42 |
75, RICU |
94.7 |
5.3 |
0 |
73.3 |
90.6 |
100 |
46.6 |
53.3 |
81.3 |
100 |
73.3 |
57.3 |
58.6 |
|
Grover et al (2018)15 |
66, ICU |
100 |
48.9 |
37.8 |
64.4 |
42.2 |
53.3 |
73.3 |
80 |
84 |
97.8 |
64.4 |
40 |
33.3 |
|
Dhoble and Vankar (2009)43 |
100, CLP |
92 |
74 |
67 |
62 |
46 |
62 |
72 |
58 |
84 |
95 |
90 |
94 |
90 |
|
Grover et al (2014)44 |
98 CLP, elderly |
96.8 |
66.3 |
32.7 |
81.6 |
82.7 |
76.5 |
83.7 |
52 |
98 |
100 |
86.7 |
55.1 |
51 |
|
Grover et al (2014)25 |
49, CAP |
91.8 |
71.4 |
28.5 |
73.4 |
5 |
69.3 |
83.6 |
34.6 |
91.8 |
93.8 |
87.7 |
59.2 |
65.3 |
|
Grover et al (2013)24 |
331, CLP |
97.8 |
57.7 |
31.7 |
59.2 |
52.6 |
65.3 |
88.8 |
36.2 |
93.6 |
96.4 |
91.8 |
69.1 |
81.2 |
|
Grover et al (2014)45 |
255, CLP |
98 |
65.9 |
37.6 |
53.7 |
68.3 |
82.9 |
93.2 |
40 |
98.5 |
99.5 |
99.5 |
83.4 |
92.2 |
|
Grover et al (2015)46 |
107, CLP, elderly |
75.7 |
55.1 |
49.1 |
71 |
88.8 |
95.3 |
68.2 |
54.2 |
98.1 |
98.1 |
89.7 |
92.5 |
96.3 |
|
Grover et al (2012)47 |
53, CLP |
100 |
81.2 |
20.7 |
83 |
81.1 |
79.2 |
94.3 |
34 |
100 |
100 |
98.6 |
94.6 |
93.1 |
|
Grover et al (2014)48 |
461, CLP |
95.4 |
71.6 |
33 |
61.6 |
74.8 |
74 |
90.9 |
29.7 |
96.1 |
94.8 |
83.1 |
52.5 |
56.6 |
|
Grover et al (2012)49 |
30, CAP |
96.1 |
80.3 |
40.8 |
78.9 |
85.8 |
76.3 |
90.8 |
50.0 |
97.4 |
100 |
98.7 |
51.3 |
57.9 |
|
Grover et al (2016)50 |
76, CLP |
100 |
73.7 |
34.2 |
82.9 |
96.1 |
96.1 |
98.7 |
1.3 |
96.1 |
97.4 |
97.4 |
93.4 |
94.7 |
|
Grover et al (2019)26 |
59, CLP |
100 |
50.5 |
62.1 |
98.1 |
98.1 |
100 |
97.1 |
73.8 |
100 |
99 |
98.1 |
88.3 |
85.4 |
|
Lahariya et al (2016)51 |
309, CCU |
100 |
70 |
22 |
100 |
59 |
90 |
73 |
40 |
94 |
100 |
100 |
86 |
66 |
|
Range |
75.7–100 |
5.3–81.2 |
0–67% |
59.2–100 |
5–98.1 |
53.3–100 |
46.6–98.7 |
1.3–80% |
81.3–100 |
93.8–100 |
64.4–100 |
40–97% |
40–97% |
|
Many studies have evaluated the factor structure of the symptom profile of delirium (Table 3).15 22 28 31 37 38 39 41 42 52 As with the symptom profile, most of these studies have again relied on DRS-R-98,15 28 31 37 39 41 52 with some of the studies using the Memorial Delirium Assessment Scale (MDAS)22 52 and Intensive Care Delirium Screening Checklist ICDSC scales.38 One study combined items of DRS-R98, CSE, and MDAS.52 Most of these studies have consistently recognized a three-factor solution,15 28 31 37 39 41 42 with some differences in the distribution of symptoms across different factors. In the majority of these studies, the cognitive symptoms load on one factor, the motoric and psychotic symptoms load on to the same factor, and the third factor consists of language and thought process abnormalities. The motoric- and psychotic-symptom factors more consistently load on to the same factor across different studies. One study which compared the patients of pure alcohol withdrawal and those with alcohol withdrawal along with some other etiologies contributing to delirium reported subtle differences in the factor structure between the two groups.31
|
Study (year) |
Sample size |
Treatment setting |
Scales used |
Percentage of variance explained (%) |
Factor structure |
|---|---|---|---|---|---|
|
Abbreviations: AWD, alcohol withdrawal delirium; CLP, consultation liaison psychiatry services; CSE, confusional state evaluation; DRS, delirium rating scale; DRS-R-98, DSR revised-1998; ICDSC, intensive care delirium screening checklist; ICU, intensive care unit; MDAS, memorial delirium assessment scale; RICU, RICU, respiratory ICU. |
|||||
|
Shyamsundar et al (2009)22 |
120 |
ICU |
MDAS |
62.7 |
Factor I (“cognitive disturbance”): impaired digit span, short-term memory impairment, disorientation, and inattention Factor II (“behavioral abnormality”): altered psychomotor activity, perceptual disturbances, delusions, disorganized thinking, sleep–wake cycle disturbances, and reduced awareness |
|
George et al (2011)52 |
53 |
ICU |
ICDSC |
56.2 |
Factor-I (altered sensorium/psychopathology): altered level of consciousness, inattention, disorientation, hallucination/delusion/psychosis, psychomotor agitation, and inappropriate speech or mood Factor-II (sleep–wake cycle problems): sleep–wake cycle disturbances and fluctuation of symptoms |
|
Jain et al (2011)38 |
86 |
CLP |
DRS-R-98 separately and DRS-R-98, MDAS, and CSE combined |
47.8 |
Factor I (“cognitive”): abnormalities of language, thought process, orientation, attention, short-term memory, long-term memory, visuospatial ability, reduced level of consciousness (awareness), and perseveration or prolonged latency Factor II (“behavioral”): sleep–wake cycle disturbances, delusions, perceptual disturbances including hallucinations, motor agitation, inverse of motor retardation, lability of affect, distractibility, irritability, and temporal onset of symptoms |
|
Grover et al (2011)37 |
151 |
CLP, drug naive |
DRS-R-98 |
47.32 |
Factor I (cognitive): attention, orientation, short-term memory, long-term memory, and visuospatial ability Factor II (sleep and motoric disturbances): sleep–wake cycle disturbances, delusions, perceptual disturbances, lability of affect, motor agitation, and inverse of motor retardation Factor III (thought, language, and fluctuations): language, thought process abnormality, temporal onset of symptoms, and fluctuations |
|
Grover et al (2012)28 |
109 |
CLP, elderly |
DRS-R-98 |
43.5 |
Factor I (cognitive): thought disturbance, short-term memory, long-term memory, and visuospatial disturbance Factor II (cognitive and diagnostic factor): disturbance of attention and concentration and the three items of diagnostic significance (temporal onset, fluctuation, and presence of physical disorder) Factor III (psychotic and motoric symptoms): perceptual disturbances, delusions, and the motoric disturbances |
|
Mattoo et al (2012)39 |
100 |
CLP, mixed adult and elderly |
DRS-R-98 |
48.5 59 |
2-factor model Factor I (cognition and thinking): delusions, language disturbances, thought process abnormality, attention, orientation, short-term memory, long-term memory, visuospatial ability, and temporal onset of symptoms Factor I (circadian): motoric disturbances and fluctuations 3-factor model Factor I (cognition): attention, orientation, short-term memory, long-term memory, visuospatial ability, and fluctuation Factor II (circadian and psychosis): sleep disturbances, delusions, hallucinations, and motoric disturbances Factor III (higher order thinking): language disturbances, thought process abnormality, and temporal onset of symptoms |
|
Grover et al (2013)41 |
321 |
CLP, mixed adult and elderly |
DRS-R-98 |
45.8 |
Factor I (psychotic and motoric disturbances): sleep–wake cycle disturbances, delusions, perceptual disturbances, lability of affect, motor agitation, inverse of motor retardation, and fluctuation Factor II (cognitive): language, thought process abnormality, short-term memory, long-term memory, and visuospatial ability Factor III (diagnostic factor): attention, orientation, temporal onset of symptoms, and physical disorder |
|
Grover et al (2013)41 |
245 |
CLP, adult |
DRS-R-98 |
46.75 |
Factor I (psychotic and motoric disturbances): sleep–wake cycle disturbances, delusions, perceptual disturbances, lability of affect, motor agitation, inverse of motor retardation, and fluctuation Factor II (cognitive): language, thought process abnormality, short-term memory, long-term memory, and visuospatial ability Factor III (diagnostic factor): attention, orientation, temporal onset of symptoms, and physical disorder |
|
Grover et al (2013)41 |
76 |
CLP, elderly |
DRS-R-98 |
48.53 |
Factor I (cognitive-1): delusions, language disturbance, thought process abnormality, long-term memory, and visuospatial ability Factor II (psychotic and motoric disturbances): sleep–wake cycle disturbances, perceptual disturbances, motor agitation, inverse of motor retardation, fluctuation, and physical disorder Factor III (cognitive-2): inverse of lability of affect, attention, orientation, short term memory, and temporal onset of symptoms |
|
Sharma et al (2017)42 |
75 |
RICU |
DRS-R-98 |
54.6–63.4 |
Factor I (cognitive factor): attention, orientation, short term memory, long-term memory, and visuospatial ability Factor II (motoric disturbances): motor agitation, inverse of motor retardation, and lability of affect Factor III (behavioral disturbances): language disturbance, thought process abnormality, temporal onset of symptoms, fluctuation |
|
Grover et al (2018)15 |
66 |
ICU |
DRS-R-98 and MDAS |
56.3 |
Factor I: perceptual disturbance, delusion, lability of affect, language, thought process abnormality, orientation, short-term memory, long-term memory, visuospatial ability, and impaired digit span Factor II: motor agitation and inverse of motor retardation Factor III: sleep wake cycle disturbances, reduced level of consciousness, and reduced ability to maintain and shift attention |
|
Grover et al (2016)31 |
112 |
CLP, AWD |
DRS-R98 |
50.09–56.59 |
Whole sample Factor I (cognitive factor): attention, orientation, short-term memory, long-term memory, visuospatial ability, language, and thought process abnormality Factor II (psychotic): perceptual disturbance, delusion, fluctuation of symptoms, and presence of physical disorder Factor III (motoric–circadian disturbance): sleep–wake cycle disturbance, lability of affect, motor agitation, and inverse of motor retardation Pure AWD Factor I (psychotic): perceptual disturbance, delusion, language, thought process abnormality, lability of affect, long-term memory, and visuospatial ability Factor II (cognitive factor): attention, orientation, short-term memory, and physical disorder Factor III (motoric–circadian disturbance): sleep–wake cycle disturbance, motor agitation, inverse of motor retardation, and fluctuation of symptoms AWD with associated etiologies Factor I (psychotic): perceptual disturbance, delusion, fluctuation of symptoms, and presence of physical disorder Factor II (cognitive factor): attention, orientation, short term memory, physical disorder, language, thought process abnormality, long-term memory, visuospatial ability, and acute onset of symptoms Factor III (motoric–circadian disturbance): sleep–wake cycle disturbance, lability of affect, motor agitation, and inverse of motor retardation |
Studies have also evaluated motoric subtypes of delirium and have come up with different prevalence rates, which are mostly influenced by the study setting and the assessment scales (Table 4).14 15 18 23 25 29 38 44 47 51 53 54 55 Most of the studies have relied upon the Delirium Motor Symptom Scale (DMSS)/amended DMSS.15 25 29 44 47 51 53 The prevalence rate of hypoactive delirium in ICUs15 18 23 51 has varied from 26 to 65%, for mixed subtype, ranges from 10.2 to 29%, and for hyperactive subtype, ranges from 15.7 to 56.8%. The prevalence rate of hyperactive delirium is significantly more in studies evaluating the patients in CLP services setting and medical-surgical wards with prevalence varying from 25 to 70% and the prevalence of hypoactive delirium range from 7.3 to 65%.14 25 29 38 44 47 53 54 55 Occasional studies have reported no subtype for approximately 5% of cases.29 51
|
Study (year) |
Treatment setting |
Diagnostic system used |
Sample size |
Assessment of motoric subtype |
Hypoactive (%) |
Mixed (%) |
Hyperactive (%) |
No subtype (%) |
|---|---|---|---|---|---|---|---|---|
|
Abbreviations: CAM-ICU, confusion assessment method for the intensive care unit; CAP, children and adolescents; CCU, coronary care unit; CLP, consultation liaison psychiatry; DMSS, delirium motor subtyping scale; DRS-R-98, delirium rating scale revised-1998; DSM IV TR, diagnostic and statistical manual of mental disorders, fourth edition, text revision; ICU, intensive care unit; MDAS, memorial delirium assessment scale; RASS, Richmond agitation-sedation scale. |
||||||||
|
Grover et al (2014)25 |
CLP |
DSM-IV TR |
98 |
DMSS |
23.5 |
21.4 |
45.9 |
8.2 |
|
Grover and Shah (2012)47 |
CLP |
DSM-IV |
53 |
DMSS |
17 |
18.9 |
58.5 |
5.6 |
|
Grover et al (2014)44 |
CLP, CAP |
DSM-IV TR |
49 |
DMSS |
16.3 |
26.5 |
53 |
4 |
|
Grover et al (2018)15 |
ICU |
DSM-IV TR |
66 |
DMSS |
47 |
29 |
24.5 |
– |
|
Jayaswal et al (2019)18 |
Medical ICU |
CAM-ICU |
280 |
RASS |
55.7 |
10.2 |
34.1 |
– |
|
Barman et al (2018)23 |
Multidisciplinary ICU |
DSM-IV |
310 |
RASS |
65 |
19.3 |
15.7% |
– |
|
Lahariya et al (2016)51 |
CCU |
DSM-IV TR |
309 |
Amended DMSS |
26 |
11.1 |
56.8 |
5 |
|
Grover et al (2015)53 |
CLP |
DSM-IV TR |
203 |
Amended DMSS |
7.3 |
36.1 |
56.6 |
– |
|
Grover et al (2014)29 |
CLP |
DSM-IV TR |
321 |
Amended DMSS |
19.93 |
24.61 |
50.15 |
5.29 |
|
Jain et al (2011)38 |
CLP |
DSM-IV TR |
86 |
DRS-R-98 |
10 |
21 |
69 |
– |
|
Kumar et al (2015)54 |
General hospital |
DSM-IV TR |
80 |
MDAS |
30 |
0 |
70 |
– |
|
Khurana et al (2011)14 |
Inpatient elderly |
CAM |
400 |
Self-designed criteria |
65 |
10 |
25 |
– |
|
Mushtaq et al (2014)55 |
Medical-surgical wards |
DSM-IV TR |
80 |
Self-designed criteria |
30 |
0 |
70 |
– |
Studies Evaluating other Aspects of Delirium in ICU Patients
Besides focusing on the incidence, prevalence, symptom profile, factor structure, and mortality in patients with delirium, studies involving ICU patients have also evaluated the risk factors and have validated scales such as ICDSC, MDAS, and CAM-ICU (Table 5).18 19 20 22 23 52 56 57 These studies suggest that these scales have good psychometric properties in ICU patients for detecting delirium.22 23 52 The cut-off score of 3 or more for ICDSC and a cut-off score of 10 or more for MDAS have been found to have good psychometric properties for delirium.22 52 One study which compared CAM-ICU and ICSDC suggests that compared with ICDSC, CAM-ICU has higher sensitivity and diagnostic odds ratio (84%, 86.1).23 One of the studies evaluated the incidence and prevalence of delirium in patients admitted to ICU and compared these figures with the psychiatric referral rates and reported a wide gap in the actual incidence and prevalence of delirium in ICU patients and those referred to psychiatry CLP services.56 Studies that have evaluated the risk factors, have, in general, reported mechanical ventilation to be an important risk factor for delirium.18 19 Some of these studies also suggest that compared with those who do not develop delirium, those with delirium have higher mortality rate and significantly longer duration of ICU stay.18 19 20
|
Study (year) |
Setting |
Findings |
|---|---|---|
|
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; AWD, alcohol withdrawal delirium; CAM-ICU, confusion assessment method for the intensive care unit; CAP, children and adolescents; CCU, coronary care unit; CI, confidence interval; CLP, consultation liaison psychiatry; DMSS, delirium motor symptom scale; DRS-R-98, delirium rating scale revised-1998; ICDSC, intensive care delirium screening checklist; ICU, intensive care unit; MMSE, Mini Mental State Examination; MRI, magnetic resonance imaging; OR, odds ratio; PTSD, posttraumatic stress order; RICU, respiratory intensive care unit; ROC, receiver operating curve; SOFA, Sequential Organ Failure Assessment. |
||
|
Studies focusing on ICU patients |
||
|
Grover et al (2017)56 |
ICU n = 66 (prospective arm) |
|
|
Mohan et al (2015)57 |
Neuro ICU 30 patients divided into two groups |
|
|
Jayaswal et al (2019)18 |
Medical ICU n = 280 |
|
|
George et al (2011)52 |
Medical ICU n = 59 |
|
|
Sharma et al (2012)19 |
RICU n = 140 |
|
|
Barman et al (2018)23 |
ICU n = 310 |
|
|
Lahariya et al (2014)20 |
CCU n = 309 |
|
|
Shyamsundar et al (2009)22 |
Medical and cardiac ICU n = 120 |
|
|
Alcohol withdrawal delirium |
||
|
Sarkar et al (2017)58 |
Psychiatry setting n = 80 |
|
|
Baby et al (2017)59 |
Emergency and inpatient services Emergency (n = 111) Comprehensive inpatient addiction treatment (CIAT) (n = 107) |
|
|
Grover et al (2016)31 |
n= 112, AWD |
|
|
Grover et al (2013)30 |
CLP n= 112, AWD |
|
|
Malhotra et al (2018)60 |
n= 210 patients with alcohol dependence and 200 controls |
|
|
CLP setting |
||
|
Prinka and Sharma (2016)61 |
Emergency and CLP n = 100 |
|
|
Grover et al (2017)62 |
CLP n = 219 |
|
|
Grover et al (2013)24 |
CLP n = 331 |
|
|
Grover et al (2015)46 |
CLP n = 107 Elderly (≥60 years) |
|
|
Grover et al (2014)44 |
CLP n = 98 Elderly ≥60 years |
|
|
Grover et al (2016)50 |
CLP n = 76 |
|
|
Grover et al (2014)48 |
CLP n = 461 Retrospective |
|
|
Grover et al (2013)41 |
CLP n = 321 (adult sample 245; geriatric 76) |
|
|
Grover et al (2014)25 |
CLP n = 49, CAP |
|
|
Rajlakshmi et al (2013)40 |
CLP n = 84 |
|
|
Grover et al (2014)45 |
CLP n = 205 |
|
|
Grover et al (2012)49 |
CLP n = 30 CAP |
|
|
Grover et al (2009)63 |
CLP n = 46 (retrospective) CAP |
|
|
Grover et al (2009)12 |
n = 3,092 Retrospective |
|
|
Grover et al (2014)29 |
CLP n = 321 |
|
|
Grover et al (2013)64 |
CLP n = 100 (replication study) |
|
|
Meagher et al (2014)65 |
CLP n = 487 |
|
|
Gupta et al (2010)66 |
CLP n = 80 |
|
|
Meagher et al (2014)67 |
CLP n = 768 Retrospective |
|
|
Khurana et al (2002)68 |
Medical-surgical ward n = 100 |
|
|
Kumar et al (2015)54 |
n = 80 |
|
|
Rai et al (2014)13 |
Neurology inpatient setting n = 52 Mean age = 65 years |
|
|
Mushtaq et al (2014)55 |
Medical-surgical inpatients n = 40 (in the delirium group) |
|
|
Postoperative |
||
|
Dhakharia et al (2017)32 |
Postoperative stage after cancer surgery n = 824 |
|
|
Chrispal et al (2010)34 |
Delirium in patient undergoing hip fractures surgery n = 81 Elderly (≥ 60 years) |
|
|
Khanna et al, (2018)35 |
n = 100 |
|
|
Studies focusing on health professionals |
||
|
Chawla et al (2014)69 |
Survey of ICU clinicians n = 659 |
|
|
Morandi et al (2017)70 |
n = 1,521 clinicians |
|
|
Varghese et al (2014)71 |
n = 32 |
|
|
Patient’s experience of delirium |
||
|
Grover et al, (2019)26 |
CLP n = 103 |
|
|
Grover and Shah (2011)72 |
CLP n = 53, patients with delirium |
|
|
Grover et al (2015)53 |
CLP n = 203 |
|
|
Studies focusing on caregivers |
||
|
Grover and Shah (2013)73 |
n = 72 caregivers of 53 patients with delirium CLP |
|
|
Grover and Shah (2012)47 |
n = 72 caregivers CLP |
|
Studies Focusing on Patients with Alcohol-Withdrawal Delirium
Five studies have primarily focused on patients with AWD (Table 5).30 31 58 59 60 One study evaluated the service model for patients with AWD and reported that compared with the emergency services treatment group alone, emergency services plus comprehensive inpatient addiction treatment group had fewer relapses.59 Other studies have focused on risk factors associated with AWD,58 symptom profile of delirium,30 and factor structure of symptom profile.31 One study evaluated the genetic variations associated with the development of delirium tremens and reported that delirium tremens was significantly associated with presence of T allele (GT and TT; [rs1824024]) of muscarinic cholinergic receptor 2 (CHRM2).60
Studies Involving Patients Seen in Medical-Surgical Consultation Liaison Setting
Maximum numbers of studies done in the medical-surgical setting (Table 5)12 13 24 25 29 40 41 44 45 46 48 49 50 54 55 61 62 63 64 65 66 67 68 have not been limited to any one particular ward. Available data suggest that delirium is the most common diagnosis made by the CLP team,12 62 diagnostic concordance of delirium between psychiatrists and physicians is low,62 and mortality of patients with delirium is more than those without delirium. The most common reason for referral of patients with delirium to CLP teams is abnormal behavior or patient’s noncooperation for treatment.12
Factors that predict a delay in referral of patients with delirium include prevalent delirium at admission, sleep–wake disturbance, the specialty of referral, presence motor retardation, being admitted to medical ward/medical ICUs, and absence of comorbid axis-1 psychiatry diagnoses. In terms of symptom/clinical profile, available data suggest that there are subtle differences between patients seen in medical-surgical wards and emergency setting.61 Available data also suggest subtle differences in the symptom profile of patients with different subtypes of delirium,25 44 patients of different age groups (children, adult, and elderly),41 43 49 63 and those with and without premorbid cognitive deficits.46 In terms of symptom profile, available data also suggest that attention deficit is the core symptom of delirium.40 One study showed a prevalence of catatonic symptoms in about one-third of the patients with delirium. Inpatient mortality in patients with delirium is associated with lower age (<65 years) and more frequent use of restraining before the development of delirium.24 Many studies have focused on the risk factors of delirium, and these studies have come up with some of the common risk and etiological factors,13 54 63 68 and other factors specific to treatment setting.24 One study validated the DMSS64 and other amended the DMSS.65 Another study evaluated the concordance between DSM-IV and DSM-5 criteria and reported considerable variability depending on how the criteria are interpreted, with very strict adherence to the text detailing DSM-5, leading to a reduction in the number of cases diagnosed with delirium; however, when a more “relaxed” approach is used, DSM-5 criteria is comparable to DSM-IV criteria.66
Studies Focusing on Postoperative Patients
Studies that have focused on postoperative patients (Table 5)32 34 35 have mainly attempted to identify the risk factors for delirium in patients of cancers undergoing surgery,32 patients undergoing surgery for hip fracture,34 and children undergoing ophthalmic examination under general anesthesia with sevoflurane.35
Studies Focusing on the Health Care Professionals
Studies evaluating the opinion of the health care professionals (Table 5)69 70 71suggest that most of the ICU clinicians do not assess patients for delirium on regular basis, consider the prevalence rates of delirium, especially among those patients on mechanical ventilation to be lower than what is reported in the literature. In terms of assessment, those ICU clinicians, who assess patients for delirium, mostly rely on the CAM-ICU scale and use haloperidol for the management of delirium.69 Data also suggest that most of the ICU clinicians are aware of the importance of early mobilization of ICU patients but are not able to practice the same due to lack of support staff and safety concerns. One study, which evaluated the practice of ABCDEF bundle across the globe and included the opinion of clinicians from India too, although did not provide India specific data, suggests that in Asia, 80% of the clinicians implement delirium monitoring, with CAM-ICU being the most common scale for assessment.70 However, in terms of the prevalence of delirium, again the awareness was low, with only 2% of the clinicians from Asia believed that >60% of the patients in the ICU have delirium. One of the studies specifically focused on nurses.71 In this study, the authors assessed the knowledge of the nurses before an education program for delirium and showed that providing knowledge about delirium to the nurses was associated with significant improvement in the knowledge and practice of nurses toward delirium.
Studies Focusing on the Experience of Patients with Delirium
Three studies (Table 5)26 53 72 have evaluated the patients’ experience and distress after the resolution of symptoms of delirium. These studies suggest that about one-fourth (28.3%)72 to one-third (35%)53 of patients remember their experience of delirium. Those who could remember their experience reported moderate-to-severe levels of distress. Those who remembered their experience, in general, described it as a state of fearfulness, anxiety, confusion, and feeling strange.72 One of the studies reported that the most common distressing themes which were recollected were fear and visual hallucination.53 In terms of symptom profile, recall of delirium experience was associated with a higher prevalence of perceptual and language disturbances, and a higher severity of delirium. Those who could not remember their delirium experience also were distressed and more often reported moderate-to-severe distress. One of the studies evaluated the patient experience in terms of posttraumatic stress disorder (PTSD) and reported that 30.5% of the patients had substantial symptoms of PTSD, 22% (n = 13) had probable symptoms of PTSD, and 15.3% were considered to have partial symptoms of PTSD after the resolution of delirium. Again, the experience of PTSD was associated with higher severity of delirium and in terms of specific symptoms, it was associated with higher mean scores for the items of motor agitation and attentional deficits.26
Studies Focusing on Caregivers of Patients with Delirium
Two studies have focused on family caregivers.47 73 According to one of the studies, symptoms of delirium are attributed to the nonorganic causes by about one-third of the caregivers.47 Other paper based on the same cohort reported severe or very severe distress in about two-thirds of the caregivers.73
Effectiveness of Medications in the Treatment of Delirium
Few studies (Table 6)74 75 76 77 78 have evaluated the effectiveness of various antipsychotic medications in the management of delirium in CLP setting.74 75 76 77 Three of these studies74 75 76 suggest that the atypical antipsychotics like olanzapine, risperidone, and quetiapine are equally effective as haloperidol. One retrospective study also showed the effectiveness of risperidone.77 One double-blind randomized controlled trial (DBRCT) compared the beneficial effect of melatonin with placebo in patients admitted to ICU with organophosphorus poisoning.78 This study showed that the use of melatonin is associated with a lower prevalence of delirium after 3 days and patients receiving melatonin spend lower time in delirium when compared with a placebo group.
|
Study (year) |
Medications compared |
Sample size |
Diagnostic measure |
Trial design |
Setting |
Outcome measure |
Outcome |
|---|---|---|---|---|---|---|---|
|
Abbreviations: ≈ No statistically significant difference; CAM-ICU, confusion assessment method for the intensive care unit; CLP, consultation liaison psychiatry; DBRCT, double-blind randomized controlled trial; DRS-R-98, delirium rating scale revised-1998; DSM IV, diagnostic and statistical manual of mental disorders, fourth edition; MDAS, memorial delirium rating scale; MMSE, mini metal state examination; |
|||||||
|
Jain et al (2017)74 |
Haloperidol (1–4 mg/day) vs. olanzapine (2.5–10 mg/day) |
Haloperidol (n = 53) Olanzapine (n = 47) |
DSM-IV |
Open-label RCT |
CLP |
MDAS |
|
|
Grover et al (2016)75 |
Haloperidol (0.25–1.25 mg/day) vs. quetiapine (12.5–75 mg/day) |
Haloperidol (n = 32) Quetiapine (n = 31) |
DSM-IV |
Single-blind RCT |
CLP |
DRS-R-98 MMSE |
|
|
Grover et al (2011)76 |
Haloperidol (0.25–10 mg/day) vs. olanzapine (1.25–20 mg/day) vs. risperidone (0.25–4 mg/day) |
Haloperidol (n = 21) Olanzapine (n = 23) Risperidone (n = 20) |
DSM-IV |
Single-blind RCT |
CLP |
DRS-R-98 MMSE |
|
|
Gupta et al (2005)77 |
Risperidone (0.5–2 mg/day) |
Risperidone (n = 7) |
– |
Retrospective study |
CLP |
– |
|
|
Vijaykumar et al (2016)78 |
Melatonin (3 mg/day) vs. placebo |
Melatonin (n = 26) Placebo (n = 26) |
– |
DBRCT |
ICU Delirium in patients with organophosphorus poisoning |
CAM-ICU |
|
Prevention of Postoperative Emergence Delirium
It is well known that the use of flurane in anesthesia among children and adolescents is associated with a higher rate of emergent delirium and agitation. Given the same, many studies (Table 7)79 80 81 82 83 84 85 86 87 88 89 90 91 have evaluated the beneficial effects of additional use of agents, like ketamine (low and high doses),79 midazolam,80 82 83 85 dexmedetomidine,81 82 83 86 87 89 90 propofol,81 glycopyrrolate,82 and bupivacaine84 in reducing the incidence of delirium. Some of the studies have also evaluated different doses of the same medications,79 87 whereas others have evaluated the different techniques of administration of these drugs86 and some of the studies have evaluated the different timing of giving these medications.80 In general, available data suggest that the incidence of emergent delirium is lower with dexmedetomidine when compared with other agents (ketamine, midazolam, and clonidine) and placebo.81 82 83 86 87 89 90 Compared with the use of bupivacaine only, the use of adjuvant ketamine along with bupivacaine is protective against emergence delirium in children.84 It has been reported that the incidence of emergence agitation is comparable across the use of most flurane anesthetic agents.91
|
Study (year) |
Medications compared |
Sample size |
Trial design |
Setting |
Outcome measure |
Outcome |
|---|---|---|---|---|---|---|
|
Abbreviations: CAM, confusion assessment method; CAM-ICU, confusion assessment method for the intensive care unit; DBRCT, double blind randomized controlled trial; EA, emergence agitation; Inj., injection; MDAS, memorial delirium assessment scale; PAED, pediatric anesthesia emergency department; RASS, Richmond agitation-sedation scale; TAP, transversus abdominis plane. |
||||||
|
Avidan et al (2017)79 |
Placebo (normal saline) vs. low-dose ketamine (0·5 mg/kg) vs. high dose ketamine (1·0 mg/kg) |
Placebo (n = 222) Low-dose ketamine (n = 227); High-dose ketamine (n = 223) |
Multicentric DBRCT |
Postsurgical |
CAM, CAM-ICU |
|
|
Gonsalvez et al (2018)80 |
Midazolam at the induction (0.03 mg/kg) vs. midazolam (0.03 mg/kg) administered 10 minutes before the end of surgery |
At Induction (n = 40) and 10 minutes before the end of surgery (n = 40) |
DBRCT |
Pediatric surgery |
PAED scale |
|
|
Makkar et al (2015)81 |
Dexmedetomidine (0.3 μg/kg) vs. propofol (1 mg/kg) vs. saline 0.9% |
Dexmedetomidine (n = 32) Propofol (n = 36) Saline (n = 32) |
RCT |
Pediatric surgery (infraumbilical surgery) |
PAED scale |
|
|
Trivedi et al (2016)82 |
Group K: premedication with inj. glycopyrrolate 0.01 mg/kg, inj. ketamine 2 mg/kg Group M: premedication with inj. glycopyrrolate 0.01 mg/kg and inj. midazolam 0.05 mg/kg, inj. ketamine 2 mg/kg, Group D: after premedication with inj. glycopyrrolate 0.01 mg/kg and inj. dexmedetomidine 0.5 μg/kg, ketamine 2 mg/kg |
Group K (n = 30) Group M (n = 30) Group D (n = 30) |
DBRCT |
Surgical setting (patients undergoing laparoscopic ligation, skin grafting, dilatation and curettage, endoscopic procedures, and excision of small swelling) |
MDAS |
|
|
Prabhu and Mehandale (2017)83 |
Comparison of oral dexmedetomidine (4 μg/kg) vs. oral midazolam (0.5 mg/kg) as premedication to prevent emergence agitation after sevoflurane anesthesia in pediatric patients |
Midazolam (n = 45) Dexmedetomidine (n = 45) |
DBRCT |
Postoperative |
PAED scale |
|
|
Sinha and Sood (2012)84 |
Comparison of caudal block with bupivacaine (0.25% 0.5 mL/kg) vs. bupivacaine (0.25% 0.5 mL/kg) and ketamine(0.5 mL/kg) and no caudal block in pediatric anesthesia with sevoflurane |
n = 150 Children |
DBRCT |
Postoperative |
PAED scale |
|
|
Perumal et al (2015)85 |
Midazolam premedication (0.02 mg/kg iv) for ketamine-induced (1 mg/kg) emergence |
n = 30 Adult |
Observational study |
Postoperative |
Self-designed criteria (presence of purposeless and hallucinatory behavior) |
|
|
Mukherjee et al (2015)86 |
Intranasal dexmedetomidine (1 μg/kg) and clonidine (4 μg/kg) in patients receiving sevoflurane-based general anesthesia |
n = 80 |
Double-blind parallel group study |
Postoperative |
PAED scale |
|
|
Begum et al (2019)87 |
Bolus dexmedetomidine (0.4 µg/kg) vs. low-dose Infusion (0.4 µg/kg/h) in children undergoing sevoflurane anesthesia |
n = 48 |
DBRCT |
Postoperative |
PAED scale |
|
|
Shenoy et al (2018)88 |
Transversus abdominis plane block supplementation during iliac crest bone graft harvesting Additional TAP block along with local infiltration Vs. wound infiltration only |
n = 143 |
Simple random sampling |
Postoperative |
Watch a scale score of >2 |
|
|
Priye et al (2015)89 |
Dexmedetomidine as an adjunct in postoperative analgesia following cardiac surgery: 12-hour infusion of normal saline and group-B received a 12-hour infusion of dexmedetomidine 0.4 μg/kg/h |
n = 64 |
Double-blind study |
Postoperative |
RASS |
|
|
Sharma et al (2019)90 |
Single dose of dexmedetomidine 1 μg/kg vs. volume matched saline for intraoperative hemodynamic and postoperative recovery profile in children undergoing adenotonsillectomy |
n = 60 Children |
Placebo-controlled study |
Intra- and postoperative |
PAED scale |
|
|
Singh et al (2012)91 |
EA in pediatric patients under isoflurane, sevoflurane or desflurane anesthesia |
n = 75 (3 groups of 25 each) Children |
DBRCT |
Postoperative |
PAED scale |
|
Case Reports focusing on Delirium
A total of 58 case reports/series have focused on delirium as the primary outcome/issue (Table 8).92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138 139 140 141 142 143 144 145 146 147 148 149 Some of these case reports have reported association of delirium with medications such as levetiracetam,92 levofloxacin,93 94 fluoroquinolones,95 zoledronate,96 a combination of albendazole and ivermectin,97 and use of cyclopentolate eye drops.98 One report presented information about delirium associated with bath salts.99 In terms of psychotropics, delirium has been reported with discontinuation of sertraline,100 use of olanzapine,101 valproate associated hyperammonemia,102 103 104 restarting of clozapine,105 mirtazapine associated hyponatremia,106 use of a combination of clozapine and electroconvulsive therapy (ECT),107 108 use of a combination of lithium and ECT,109 110 and postinjection delirium/sedation syndrome associated with olanzapine depot injection.111 112 113 114 115 Some of the case reports/case series focus on substance-related delirium,116 117 118 119 120 121 122 123 124 125 126 127 128 either during the withdrawal phase or intoxication phase. The case reports also cover topics like refractory delirium tremens,116 delayed onset delirium tremens,119 delirium tremens with hollow viscus perforation,120 genital self-mutilation in alcohol withdrawal state complicated with delirium,116 delirium during opioid withdrawal,122 naltrexone precipitating delirium,121 delirium due to use of parental tramadol,125 varenicline-induced delirium,126 and delirium associated with zolpidem withdrawal127 or intoxication.128 Delirium has also been reported in association with various physical illnesses such as nephrotic syndrome,129 chronic lymphocytic leukemia,130 Parkinson’s disease,131 pancreatic pseudocyst,132 hypopituitarism,133 postoperative state,134 sepsis,135 tuberculous meningitis,136 137 and thalamic infarcts.138 One case report has focused on long-standing delirium secondary to hypoxic–ischemic encephalopathy following complete hanging.139 Some of the reports have primarily focused on persistent140 or prolonged141 or protracted delirium142 and delirious mania.143 144 145 Only four reports146 147 148 149 talked about interventions for delirium, with one focusing on the use of oxazepam in the treatment of delirium tremens,149 the use of olanzapine for delirium in Parkinsonism,146 use of propofol as adjuvant therapy in refractory delirium tremens,147 and ECT for management of delirious mania.148
|
Study (year) |
Findings |
|
|---|---|---|
|
Abbreviation: ECT, electroconvulsive therapy. |
||
|
Medication associated delirium |
||
|
1 |
Kasim et al (2019)92 |
Levetiracetam associated delirium in an elderly |
|
2 |
Ghoshal et al (2015)93 |
Levofloxacin induced anaphylaxis and acute delirium |
|
3 |
Raj and Murthy (2013)94 |
Levofloxacin induced delirium |
|
4 |
Chowdhry et al (2015)95 |
Fluoroquinolones: an underrecognized cause for delirium |
|
5 |
Nasiruddin et al (2014)96 |
Acute delirium in an elderly woman following zoledronate administration |
|
6 |
Kaur et al (2017)97 |
Delirium induced by albendazole–ivermectin combination |
|
7 |
Mane and Angane (2019)98 |
Cyclopentolate 1% eye drops induced delirium in a Child |
|
8 |
Sharma et al (2012)99 |
Bath salts-induced delirium |
|
Delirium associated with psychotropics |
||
|
9 |
Das et al (2019)100 |
Delirium associated with discontinuation of sertraline in an elderly |
|
10 |
Sharma and Aggarwal (2010)101 |
Delirium associated with olanzapine therapy in an elderly male with bipolar affective disorder |
|
11 |
Dixit et al (2015)102 |
Valproate induced delirium due to hyperammonemia in a case of acute mania |
|
12 |
Muraleedharan et al (2015)103 |
Valproate induced hyperammonemic delirium |
|
13 |
Pradeep (2008)104 |
Valproate monotherapy induced-delirium due to hyperammonemia |
|
14 |
Khanra et al (2016)105 |
Unusual case of delirium after restarting clozapine |
|
15 |
Ghosh et al (2014)106 |
Mirtazapine-associated hyponatremia presenting as delirium |
|
16 |
Manjunatha et al (2011)107 |
Delayed onset, protracted delirium and aspiration pneumonitis associated with use of a combination of clozapine and ECT |
|
17 |
Kumar et al (2003)108 |
Delirium associated with combination of clozapine and ECT |
|
18 |
Sadananda et al (2013)109 |
Delirium during the course of electroconvulsive therapy in a patient on lithium carbonate treatment |
|
19 |
Selvaraj and Praharaj (2012)110 |
Delayed onset and prolonged interictal delirium following electroconvulsive therapy |
|
20 |
Sarangula et al (2016)111 |
Post injection delirium/sedation syndrome associated with olanzapine depot injection |
|
21 |
Garg et al (2019)112 |
Delayed onset post injection delirium/sedation syndrome associated with olanzapine pamoate a case report |
|
22 |
Punnoose et al (2017)113 |
Low body mass index a risk factor for post-injection delirium/sedation syndrome with depot olanzapine |
|
23 |
Upadhyay et al (2017)114 |
Post injection delirium/sedation syndrome with long-acting olanzapine pamoate |
|
24 |
Venkatesan et al (2019)115 |
Post-injection delirium/sedation syndrome after 31st long-acting olanzapine depot injection |
|
Delirium associated with alcohol or opioid withdrawal |
||
|
25 |
Mattoo et al (2012)116 |
Refractory delirium tremens |
|
26 |
Ram et al (2017)117 |
Lorazepam precipitated alcohol withdrawal delirium |
|
27 |
Charan et al (2011)118 |
Genital self-mutilation in alcohol withdrawal state complicated with delirium |
|
28 |
Saddichha et al (2008)119 |
Delayed-onset delirium tremens |
|
29 |
Talikoti et al (2012)120 |
Delirium tremens with hollow viscus perforation |
|
30 |
Das et al (2005)121 |
Naltrexone precipitating delirium in a patient with opioid dependence |
|
31 |
Das et al (2017)122 |
Opioid withdrawal presenting as delirium |
|
32 |
Sharma et al (2017)123 |
Opium withdrawal delirium |
|
33 |
Raj et al (2017)124 |
Complicated opioid withdrawal in delirium without convulsions |
|
34 |
Ghosh et al (2013)125 |
Acute delirium due to parenteral tramadol |
|
35 |
Narayan et al (2015)126 |
Varenicline induced delirium in an alcohol and nicotine dependent patient |
|
36 |
Mattoo et al (2011)127 |
Zolpidem withdrawal delirium |
|
37 |
Sharan et al (2007)128 |
Intoxication delirium associated with zolpidem |
|
Delirium associated with specific physical illnesses |
||
|
38 |
Padhy et al (2008)129 |
Delirium in a child with nephrotic syndrome |
|
39 |
Manamohan et al (2017)130 |
Delirium in an elderly with chronic lymphocytic leukemia |
|
40 |
Manappallil (2016)131 |
Delirium in a patient with Parkinson’s disease |
|
41 |
Singh (2017)132 |
Pancreatic pseudocyst with delirium in an alcohol dependent male |
|
42 |
Khanna (1988)133 |
Hypopituitarism presenting as delirium |
|
43 |
Pappachan and Agrawal (2019)134 |
Postoperative delirium |
|
44 |
Nag et al (2016)135 |
Sepsis associated delirium mimicking postoperative delirium as the initial presenting symptom of urosepsis in a patient who underwent nephrolithotomy |
|
45 |
Jebaraj et al (2005)136 |
Tuberculous meningitis masked by delirium in an alcohol-dependent patient |
|
46 |
Upadhyaya et al (2011)137 |
Delirium and catatonia in a person with alcohol dependence with tubercular meningoencephalitis |
|
47 |
Raina et al (2019)138 |
Hyperactive delirium and bilateral ptosis: bilateral thalamic infarcts due to artery of Percheron occlusion |
|
Prolonged or persistent delirium |
||
|
48 |
Sireesha et al (2013)139 |
Prolonged delirium secondary to hypoxic–ischemic encephalopathy following complete hanging |
|
49 |
Grover et al (2014)140 |
Persistent delirium |
|
50 |
Thukral et al (2013)141 |
Conundrum of prolonged delirium |
|
51 |
Achalia et al (2018)142 |
Protracted delirium tremens |
|
Delirious mania |
||
|
52 |
Soni et al (2015)143 |
Delirious mania in elderly |
|
53 |
Chawla et al (2018)144 |
Identification and management of “delirious mania”: a rare clinical entity |
|
54 |
Bipeta and Khan (2012)145 |
Delirious mania |
|
Management of delirium |
||
|
55 |
Gupta et al (2004)146 |
Olanzapine for delirium in Parkinsonism |
|
56 |
Mahajan et al (2010)147 |
Use of propofol as an adjuvant therapy in refractory delirium tremens |
|
57 |
Danivas et al (2010)148 |
Electroconvulsive therapy in the treatment of delirious mania |
|
58 |
Narayanaswamy et al (2012)149 |
Successful use of oxazepam in the treatment of delirium tremens |
Discussion
This systematic review suggests that there is a limited research on delirium from India. However, a good thing is that in recent times, delirium has received more research attention, compared with about a decade back. This review further suggests that although psychiatrists have performed the majority of research in the area of delirium, in the recent years, other specialists too, especially, anesthetists have also shown interest in delirium and some of the studies have focused on incidence/prevalence of delirium in ICUs, postoperative delirium,32 33 and emergent delirium.35 36 Another important aspect that is evident from the available literature is that most of the studies have been based on standard evaluation instruments.
Although there are methodological differences across different studies, available data from India suggest that the prevalence and incidence of delirium in various ICUs have varied from 16.1 to 68.2 and 8 to 59.6%, respectively. In terms of specific non-ICU setting, the prevalence rates vary, depending on the study setting. When one compares the incidence and prevalence figures with the available western literature,174 it can be said that these figures from India are comparable to those reported from other parts of the globe. Although, no much information is available in terms of the practices to assess delirium and the knowledge about delirium of clinicians from various specialties, few studies which involved clinicians from India, suggest that most of the ICU clinicians do not assess patients for delirium on regular basis and consider the prevalence rates of delirium, especially among those patients on mechanical ventilation to be lower than what is reported in the literature.175 Data also suggest that there is a low concordance rate between the diagnosis made by the psychiatrist and other clinicians67 and most of the ICU clinicians are aware of the importance of early mobilization of ICU patients but are not able to practice the same due to lack of support staff and safety concerns.69 A study, which focused on improving the knowledge of the nurses, showed that it was associated with significant improvement in the knowledge and practice of nurses toward delirium.71 Taken together, it can be said that the incidence and prevalence of delirium in various treatment settings in India are high and comparable to the rest of the world. However, many times, clinicians do not focus on this entity due to lack of awareness and do not screen patients for delirium regularly. Accordingly, it can be said that there is a need to improve the knowledge base, awareness, and change in clinical practice to identify delirium and manage the same in the Indian context to reduce the negative impact of the same on the patients and their caregivers. In India, ICU facilities and ventilators are also a scarcity. Accordingly, prevention and early identification of delirium can reduce the duration of ICU stay and the number of days on ventilators. This would help more patients to utilize these scarce resources. Mental health professionals need to play an important role in improving the awareness of other clinicians about delirium. Mental health professionals can train the clinicians and nurses to identify the patients who are at higher risk of delirium, screen patients, if not all inpatients, then patients at high risk for delirium on day-to-day basis, institute reorientation cues, other behavioral measures, and environmental measures to improve the outcome of patients with delirium.
In terms of mortality, data from India suggest inpatient mortality in patients with delirium is 6.6 to 30.7%12 14 17 18 19 20 24 25 26 27 28 29 30 31 and some data suggest that this mortality rate is more than that seen in patients without delirium. Postdischarge, over 1 to 6 months after discharge, the mortality increases to approximately 15.9 to 34.6%.13 18 27 Considering these, it can be said that there is a need to improve the awareness of clinicians and other medical professionals about the negative impact of delirium on mortality rates. This may be an important motivating factor for clinicians to manage delirium in their patients.
One of the major areas of research on delirium from India is symptom profile and the factor structure of the symptoms. In general, studies involving the patients in the CLP setting suggest that the majority of the patients of delirium have symptoms of attention deficits, disorientation, sleep–wake cycle disturbances, and motor agitation. Studies that have focused on different subgroups suggest that there are minor differences in the symptom profile of patients belonging to different age groups25 37 41 44 49 (elderly, adult, and children), different motoric subtypes,29 and those with AWD.31 Further, when one compares the symptom profile of those reported for patients in CLP setting and the ICUs, it is evident that patients in the CLP setting have a higher frequency of motor agitation, whereas studies in ICUs suggest a higher frequency of motor retardation.15 42 51 These differences possibly actually reflect the differences in the study design than the actual difference in the symptom profile. Studies that have evaluated patients in ICUs have focused on all the patients in the ICUs and hence, they are more often able to include hypoactive patients too, which form a small proportion of patients referred to the CLP setting. When one compares the data from India, the findings from India align with studies from other parts of the world.176
Studies that have evaluated the factor structure of symptoms of delirium suggest that symptoms cluster on to two to three factors. In the majority of these studies, various cognitive symptoms load onto the same factor, the motoric and psychotic symptoms load together, and the third factor consists of language and thought process abnormalities. In general, data suggest that the motoric and psychotic symptoms more consistently load on to the same factor across different studies. These findings are also supported by the existing literature from other parts of the world.177
In terms of other research endeavors, occasional studies from India have attempted to validate various instruments used for screening and diagnosing delirium.22 23 52 The instruments which have been validated and evaluated for some psychometric properties in studies from India include ICDSC, MDAS, CAM-ICU, DMSS, and development of DMSS-4 item version. Accordingly, this area of research requires a major boost in the form of development of new instruments and validation of other existing instruments. This will possibly help to study delirium in a much better way.
Although alcohol dependence is reported to be one of the major substances of abuse in India, AWD has received limited research attention. In terms of AWD, available data suggest that compared with emergency services treatment only, emergency services plus comprehensive inpatient addiction treatment is associated with fewer relapses.59 Based on this, it can be said that there is a need to develop service models, which will have the mechanism of transferring patients of AWD from emergency settings to inpatient settings after initial stabilization.
Available data also suggest that delirium is the most common diagnosis made by the CLP team.62 Other studies from India, which have focused on the prevalence of various psychiatric disorders among patients seen in CLP setting, suggest that the prevalence of delirium ranges from 0.2 to 0.53% in all the admitted patients.178 These findings suggest that delirium should form a major focus for CLP training. Further, it can be said that focusing on delirium in undergraduate training can lead to a reduction in stigma associated with psychiatry, in medical professionals.
Some of the available data from India suggest that symptoms of delirium are associated with significant distress in patients and their caregivers. Accordingly, there is a need to develop supportive intervention programs for these patients to minimize the negative impact of delirium on the sufferers and their caregivers.
In terms of intervention, almost all the studies have focused on one or the other pharmacological agents in the prevention and management of delirium.74 75 76 77 78 These studies suggest that atypical antipsychotics, like olanzapine, risperidone, and quetiapine, are not inferior to haloperidol in the management of delirium. Data from other countries also support the same.179 However, it is important to note that the trials evaluating these molecules are of small sample size and short duration. In terms of prevention, most of the studies have focused on reduction in the incidence of emergent delirium in children receiving flurane anesthesia and these studies suggest that additional use of agents, like ketamine (low and high doses), midazolam, dexmedetomidine, propofol, glycopyrrolate, and bupivacaine are of some benefit.
Limitations of the Literature and Future Directions
If one looks at the available literature, it is evident that although delirium occurs at the interface of psychiatry and other clinical specialties, in general, there is a lack of interdisciplinary research in this area. Further, there is a lack of multicentric studies on delirium and there are only occasional attempts at collaboration with researchers from other parts of the globe.174 Further, only the Indian Psychiatric Society has come up with the management guidelines for delirium,173 with none of the other professional associations from India, coming up with any other recommendations on the subject. Keeping this in mind, there is a need to develop collaborations at the institutional level to start multidisciplinary research and also develop collaboration across various institutes. This will not only lead to an improvement in the research output on the subject but will also help in developing intervention models which can be implemented in resource-constrained countries like India. Further, these collaborations will also help to develop instruments that may be more suitable for the Indian setting. Further, forming a multidisciplinary professional society for delirium, like the American Delirium Society and European Delirium Society, can provide a platform for further exchange of ideas and collaborative research.
If one closely examines the available literature from India, except for a few studies, most of the studies have been limited to approximately 100 participants or less. Accordingly, these studies can be considered as underpowered and collaborative research can address this issue further. One of the important examples of delirium research comes from Italy, in which like-minded researchers joined together for the “Delirium Day” research, which focused on point prevalence of delirium in 1,867 elderly patients across 108 acute and 12 rehabilitation wards.180 In this study, delirium was assessed across all the centers on the same day. If researchers from India can take a lead from this, doing this kind of research can help in improving the data and understanding about delirium.
Across the globe, nonpharmacological measures are considered to be the first-line management for delirium and a lot of efforts have been made to evaluate various nonpharmacological treatment bundles, such as HELP program and ABCDEF bundle.9 10 Available data suggest that these programs are very useful in the prevention, early identification, and management of delirium.7 8 However, none of the studies have evaluated the various nonpharmacological measures for the prevention and management of delirium in the Indian setting. This area requires a major boost if we need to improve the outcome of delirium.
One of the major strengths of India is family system.181 Whenever a person from the family falls ill, their family is always available to support the person. However, except for the occasional study, there is no research from India, as to how we can utilize this asset to improve the outcome of patients with delirium.
One of the major areas of research, which has not caught the attention of researchers from India, is an evaluation of biomarkers of delirium. One of the major risk factors for delirium is dementia. However, this group of patients has also not received any major attention. As the elderly population is on the rise and India is already an aging country, we need to focus on understanding delirium in this group of patients.
Conclusion
To conclude, this systematic review suggests that although there is limited research on delirium from India, in recent years there is an increase in research output concerning delirium. Available data suggest that most of the studies have focused on the incidence, prevalence, and symptom profile of patients of delirium.
Conflict of Interest
None declared.
References
- 2019. Assessment and management of delirium in medical practice. In: Hemanshu Prabhakar, ed. Neurointensive Care. New Delhi, India: Oxford University Press India
- Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am J Geriatr Psychiatry. 2013;21(12):1190-1222.
- [Google Scholar]
- Delirium pathophysiology: an updated hypothesis of the etiology of acute brain failure. Int J Geriatr Psychiatry. 2018;33(11):1428-1457.
- [Google Scholar]
- Delirium superimposed on dementia precipitated by an unexpected bladder tumour. BMJ Case Rep. 2019;12(9):12.
- [Google Scholar]
- 2015. Kate N. Developments in psychiatry in India. In: Malhotra S, Chakrabarti S, eds. Developments in Psychiatry in India: Clinical, Research and Policy Perspectives. New Delhi, India: Springer India
- Improving hospital survival and reducing brain dysfunction at seven california community hospitals: implementing pad guidelines via the ABCDEF bundle in 6,064 patients. Crit Care Med. 2017;45(2):171-178.
- [Google Scholar]
- Hospital elder life program: systematic review and meta-analysis of effectiveness. Am J Geriatr Psychiatry. 2018;26(10):1015-1033.
- [Google Scholar]
- The hospital elder life program: a model of care to prevent cognitive and functional decline in older hospitalized patients. J Am Geriatr Soc. 2000;48(12):1697-1706.
- [Google Scholar]
- Sedation, delirium and mechanical ventilation: the ‘ABCDE’ approach. Curr Opin Crit Care. 2011;17(1):43-49.
- [Google Scholar]
- Prevalence of delirium in geriatric hospitalized general medical population. Indian J Psychiatry. 2002;44(1):41-46.
- [Google Scholar]
- Prevalence and clinical profile of delirium: a study from a tertiary-care hospital in north India. Gen Hosp Psychiatry. 2009;31(1):25-29.
- [Google Scholar]
- Acute confusional state/delirium: An etiological and prognostic evaluation. Ann Indian Acad Neurol. 2014;17(1):30-34.
- [Google Scholar]
- Evaluation of delirium in elderly: a hospital-based study. Geriatr Gerontol Int. 2011;11(4):467-473.
- [Google Scholar]
- Delirium in intensive care unit: phenomenology, subtypes, and factor structure of symptoms. Indian J Psychol Med. 2018;40(2):169-177.
- [Google Scholar]
- ICU delirium and clinical parameters - An observational survey. Indian Journal of Psychiatric Nursing.. 2016;11:10.
- [Google Scholar]
- Incidence, prevalence and risk factors for delirium in elderly admitted to a coronary care unit. Journal of Geriatric Mental Health.. 2014;1:45.
- [Google Scholar]
- Delirium in medical intensive care units: Incidence, subtypes, risk factors, and outcome. Indian J Psychiatry. 2019;61(4):352-358.
- [Google Scholar]
- Incidence, prevalence, risk factor and outcome of delirium in intensive care unit: a study from India. Gen Hosp Psychiatry. 2012;34(6):639-646.
- [Google Scholar]
- Delirium in patients admitted to a cardiac intensive care unit with cardiac emergencies in a developing country: incidence, prevalence, risk factor and outcome. Gen Hosp Psychiatry. 2014;36(2):156-164.
- [Google Scholar]
- Diagnostic accuracy of delirium assessment methods in critical care patients. J Crit Care. 2018;44:82-86.
- [Google Scholar]
- Risk factors for delirium and inpatient mortality with delirium. J Postgrad Med. 2013;59(4):263-270.
- [Google Scholar]
- Do motor subtypes of delirium in child and adolescent have a different clinical and phenomenological profile? Gen Hosp Psychiatry. 2014;36(2):187-191.
- [Google Scholar]
- Post-traumatic stress disorder (PTSD) related symptoms following an experience of delirium. J Psychosom Res. 2019;123:109725.
- [Google Scholar]
- [The mortality rate among patients with delirium 6 months after diagnosis by a consultation-liaison psychiatric team] (in Turkish) Turk Psikiyatr Derg. 2012;23(3):189-192.
- [Google Scholar]
- Delirium in elderly people: a study of a psychiatric liaison service in north India. Int Psychogeriatr. 2012;24(1):117-127.
- [Google Scholar]
- Comparison of symptoms of delirium across various motoric subtypes. Psychiatry Clin Neurosci. 2014;68(4):283-291.
- [Google Scholar]
- Symptom profile and outcome of delirium associated with alcohol withdrawal syndrome: a study from India. Am J Addict. 2013;22(5):503-509.
- [Google Scholar]
- Symptom profile of alcohol withdrawal delirium: factor analysis of Delirium Rating Scale-Revised-98 version. Am J Drug Alcohol Abuse. 2016;42(2):196-202.
- [Google Scholar]
- Postoperative delirium in Indian patients following major abdominal surgery for cancer: risk factors and associations. Indian J Surg Oncol. 2017;8(4):567-572.
- [Google Scholar]
- Delirium after cardiac surgery: a pilot study from a single tertiary referral center. Ann Card Anaesth. 2017;20(1):76-82.
- [Google Scholar]
- The clinical profile and association of delirium in geriatric patients with hip fractures in a tertiary care hospital in India. J Assoc Physicians India. 2010;58:15-19.
- [Google Scholar]
- Correlation between duration of preoperative fasting and emergence delirium in pediatric patients undergoing ophthalmic examination under anesthesia: a prospective observational study. Paediatr Anaesth. 2018;28(6):547-551.
- [Google Scholar]
- Postoperative emergence delirium in pediatric patients undergoing cataract surgery–a comparison of desflurane and sevoflurane. Paediatr Anaesth. 2013;23(12):1131-1137.
- [Google Scholar]
- A factor analytic study of the Delirium Rating Scale-Revised-98 in untreated patients with delirium. J Psychosom Res. 2011;70(5):473-478.
- [Google Scholar]
- Symptoms of delirium: an exploratory factor analytic study among referred patients. Gen Hosp Psychiatry. 2011;33(4):377-385.
- [Google Scholar]
- Symptom profile and etiology of delirium in a referral population in northern india: factor analysis of the DRS-R98. J Neuropsychiatry Clin Neurosci. 2012;24(1):95-101.
- [Google Scholar]
- Relationship between cognitive and non-cognitive symptoms of delirium. Asian J Psychiatr. 2013;6(2):106-112.
- [Google Scholar]
- Symptoms and aetiology of delirium: a comparison of elderly and adult patients. East Asian Arch Psychiatry. 2013;23(2):56-64.
- [Google Scholar]
- Symptom profile as assessed on delirium rating scale-revised-98 of delirium in respiratory intensive care unit: A study from India. Lung India. 2017;34(5):434-440.
- [Google Scholar]
- Motoric subtypes of delirium in geriatric patients. J Geriatr Ment Health.. 2014;1:14.
- [Google Scholar]
- Do patients of delirium have catatonic features? An exploratory study. Psychiatry Clin Neurosci. 2014;68(8):644-651.
- [Google Scholar]
- Influence of preexisting cognitive deficits on symptom profile and motoric subtypes of delirium. J Geriatr Ment Health.. 2015;2:83.
- [Google Scholar]
- Perceptions among primary caregivers about the etiology of delirium: a study from a tertiary care centre in India. Afr J Psychiatry (Johannesbg). 2012;15(3):193-195.
- [Google Scholar]
- Delirium: predictors of delay in referral to consultation liaison psychiatry services. Indian J Psychiatry. 2014;56(2):171-175.
- [Google Scholar]
- Symptom profile of delirium in children and adolescent–does it differ from adults and elderly? Gen Hosp Psychiatry. 2012;34(6):626-632.
- [Google Scholar]
- Association of cognitive and noncognitive symptoms of delirium: a study from consultation-liaison psychiatry set-up. J Neurosci Rural Pract. 2016;7(01):S7-S12.
- [Google Scholar]
- Phenomenology of delirium among patients admitted to a coronary care unit. Nord J Psychiatry. 2016;70(8):626-632.
- [Google Scholar]
- Validation of the intensive care delirium screening checklist in nonintubated intensive care unit patients in a resource-poor medical intensive care setting in South India. J Crit Care. 2011;26(2):138-143.
- [Google Scholar]
- Experience in delirium: is it distressing? J Neuropsychiatry Clin Neurosci. 2015;27(2):139-146.
- [Google Scholar]
- Etiologic and cognitive differences in hyperactive and hypoactive delirium. Prim Care Companion CNS Disord. 2015;17(6):17.
- [Google Scholar]
- Recognizing changes in cognition in sub types of acute confusional state. J Clin Diagn Res. 2014;8(7):MC01-MC03.
- [Google Scholar]
- Intensive care unit delirium: a wide gap between actual prevalence and psychiatric referral. J Anaesthesiol Clin Pharmacol. 2017;33(4):480-486.
- [Google Scholar]
- A study of phenomenology of delirium in patients with and without neuroimaging changes. Archives of Mental Health.. 2015;16:129.
- [Google Scholar]
- Risk factors for the development of delirium in alcohol dependence syndrome: clinical and neurobiological implications. Indian J Psychiatry. 2017;59(3):300-305.
- [Google Scholar]
- Comparative outcome in patients with delirium tremens receiving care in emergency services only versus those receiving comprehensive inpatient care. Indian J Psychiatry. 2017;59(3):293-299.
- [Google Scholar]
- An exploratory study of candidate gene(s) for delirium tremens: adding the new cholinergic dimension to the conundrum. Asian J Psychiatr. 2018;31:137-141.
- [Google Scholar]
- Comparative study of delirium in emergency and consultation liaison- a tertiary care hospital based study in Northern India. J Clin Diagn Res. 2016;10:VC01-VC05.
- [Google Scholar]
- Reasons for referral and diagnostic concordance between physicians/surgeons and the consultation-liaison psychiatry team: An exploratory study from a tertiary care hospital in India. Indian J Psychiatry. 2017;59(2):170-175.
- [Google Scholar]
- Replication analysis for composition of the delirium motor subtype scale (DMSS) in a referral cohort from Northern India. Psychiatry Res. 2013;206(1):68-74.
- [Google Scholar]
- Development of an abbreviated version of the delirium motor subtyping scale (DMSS-4) Int Psychogeriatr. 2014;26(4):693-702.
- [Google Scholar]
- Predictors of delayed identification of delirium in a general hospital liaison psychiatry service: a study from North India. Asian J Psychiatr. 2010;3(1):31-32.
- [Google Scholar]
- Concordance between DSM-IV and DSM-5 criteria for delirium diagnosis in a pooled database of 768 prospectively evaluated patients using the delirium rating scale-revised-98. BMC Med. 2014;12:164.
- [Google Scholar]
- Risk factors in delirious geriatric general medical inpatients. Indian J Psychiatry. 2002;44(3):266-272.
- [Google Scholar]
- Current practices of mobilization, analgesia, relaxants and sedation in Indian ICUs: a survey conducted by the Indian Society of Critical Care Medicine. Indian J Crit Care Med. 2014;18(9):575-584.
- [Google Scholar]
- Worldwide survey of the “Assessing Pain, Both Spontaneous Awakening and Breathing Trials, Choice of Drugs, Delirium Monitoring/Management, Early Exercise/Mobility, and Family Empowerment” (ABCDEF) bundle. Crit Care Med. 2017;45(11):e1111-e1122.
- [Google Scholar]
- Delirium in older people in hospital: an education programme. Br J Nurs. 2014;23(13):704-709.
- [Google Scholar]
- Delirium-related distress in caregivers: a study from a tertiary care centre in India. Perspect Psychiatr Care. 2013;49(1):21-29.
- [Google Scholar]
- Comparison of efficacy of haloperidol and olanzapine in the treatment of delirium. Indian J Psychiatry. 2017;59(4):451-456.
- [Google Scholar]
- Comparative effectiveness of quetiapine and haloperidol in delirium: a single blind randomized controlled study. World J Psychiatry. 2016;6(3):365-371.
- [Google Scholar]
- Comparative efficacy study of haloperidol, olanzapine and risperidone in delirium. J Psychosom Res. 2011;71(4):277-281.
- [Google Scholar]
- Effect of melatonin on duration of delirium in organophosphorus compound poisoning patients: a double-blind randomised placebo controlled trial. Indian J Anaesth. 2016;60(11):814-820.
- [Google Scholar]
- PODCAST Research Group. Intraoperative ketamine for prevention of postoperative delirium or pain after major surgery in older adults: an international, multicentre, double-blind, randomised clinical trial. Lancet. 2017;390(10/091):267-275.
- [Google Scholar]
- Prevention of emergence delirium in children - a randomized study comparing two different timings of administration of midazolam. Anesth Essays Res. 2018;12(2):522-527.
- [Google Scholar]
- A comparative study of dexmedetomidine and midazolam in reducing delirium caused by ketamine. J Clin Diagn Res. 2016;10(8):UC01-UC04.
- [Google Scholar]
- Comparison of oral dexmedetomidine versus oral midazolam as premedication to prevent emergence agitation after sevoflurane anaesthesia in paediatric patients. Indian J Anaesth. 2017;61(2):131-136.
- [Google Scholar]
- Caudal block and emergence delirium in pediatric patients: Is it analgesia or sedation. Saudi J Anaesth. 2012;6(4):403-407. ?
- [Google Scholar]
- Midazolam premedication for Ketamine-induced emergence phenomenon: a prospective observational study. J Res Pharm Pract. 2015;4(2):89-93.
- [Google Scholar]
- Emergence agitation prevention in paediatric ambulatory surgery: a comparison between intranasal dexmedetomidine and clonidine. J Res Pharm Pract. 2015;4(1):24-30.
- [Google Scholar]
- Dexmedetomidine as bolus or low-dose infusion for the prevention of emergence agitation with sevoflurane anesthesia in pediatric patients. Anesth Essays Res. 2019;13(1):57-62.
- [Google Scholar]
- Transversus abdominis plane block supplementation during iliac crest bone graft harvesting - effect on postoperative pain. J Anaesthesiol Clin Pharmacol. 2018;34(4):472-477.
- [Google Scholar]
- Dexmedetomidine as an adjunct in postoperative analgesia following cardiac surgery: a randomized, double-blind study. Saudi J Anaesth. 2015;9(4):353-358.
- [Google Scholar]
- Effect of single-dose dexmedetomidine on intraoperative hemodynamics and postoperative recovery during pediatric adenotonsillectomy. Anesth Essays Res. 2019;13(1):63-67.
- [Google Scholar]
- Comparative evaluation of incidence of emergence agitation and post-operative recovery profile in paediatric patients after isoflurane, sevoflurane and desflurane anaesthesia. Indian J Anaesth. 2012;56(2):156-161.
- [Google Scholar]
- Levetiracetam as a cause of delirium in elderly patient: a case report. Kerala Journal of Psychiatry.. 2019;31:18-22.
- [Google Scholar]
- Management of levofloxacin induced anaphylaxis and acute delirium in a palliative care setting. Indian J Palliat Care. 2015;21(1):76-78.
- [Google Scholar]
- Levofloxacin induced delirium with psychotic features in a young patient. Med J Armed Forces India. 2013;69(4):404-405.
- [Google Scholar]
- Fluoroquinolones: An under-recognized cause for delirium. J Anaesthesiol Clin Pharmacol. 2015;31(3):410-411.
- [Google Scholar]
- Acute delirium in an elderly woman following zoledronate administration. J Pharmacol Pharmacother. 2014;5(3):217-219.
- [Google Scholar]
- Delirium induced by albendazole-ivermectin combination: report of the first case in an older patient. Geriatr Gerontol Int. 2017;17(12):2618-2620.
- [Google Scholar]
- Cycloplegic eye drop-induced delirium in a child. Ann Indian Psychiatry.. 2019;3:182.
- [Google Scholar]
- Bath salts-induced delirium and brief psychotic episode in an otherwise healthy young man. Prim Care Companion CNS Disord. 2012;14(2):14.
- [Google Scholar]
- Delirium associated with discontinuation of sertraline in an elderly. Indian J Psychiatry. 2019;61(6):660-661.
- [Google Scholar]
- Delirium associated with olanzapine therapy in an elderly male with bipolar affective disorder. Psychiatry Investig. 2010;7(2):153-154.
- [Google Scholar]
- Valproate induced delirium due to hyperammonemia in a case of acute mania: a diagnostic dilemma. J Clin Diagn Res. 2015;9(4):VD01-VD02.
- [Google Scholar]
- Valproate monotherapy induced-delirium due to hyperammonemia: A report of three adult cases with different types of presentation. Indian J Psychiatry. 2008;50(2):121-123.
- [Google Scholar]
- An unusual case of delirium after restarting clozapine. Clin Psychopharmacol Neurosci. 2016;14(1):107-108.
- [Google Scholar]
- Mirtazapine-associated hyponatremia presenting as delirium. Indian J Pharmacol. 2014;46(4):448-449.
- [Google Scholar]
- Delayed onset, protracted delirium and aspiration pneumonitis associated with a combination of clozapine and electroconvulsive therapy. Indian J Psychol Med. 2011;33(1):80-82.
- [Google Scholar]
- ECT and clozapine combination producing delirium : a case report. Indian J Psychiatry. 2003;45(3):193.
- [Google Scholar]
- Delirium during the course of electroconvulsive therapy in a patient on lithium carbonate treatment. Gen Hosp Psychiatry. 2013;35(6):678.e1-678.e2.
- [Google Scholar]
- Delayed onset and prolonged interictal delirium following electroconvulsive therapy. Psychogeriatrics. 2012;12(3):211-213.
- [Google Scholar]
- Postinjection delirium/sedation syndrome with olanzapine depot injection. Indian J Psychol Med. 2016;38(4):366-369.
- [Google Scholar]
- Delayed onset postinjection delirium/sedation syndrome associated with olanzapine pamoate: a case report. J Clin Psychopharmacol. 2019;39(5):523-524.
- [Google Scholar]
- Is low body mass index a risk factor for postinjection delirium/sedation syndrome? Indian J Psychol Med. 2017;39(3):380.
- [Google Scholar]
- Postinjection delirium/sedation syndrome with long-acting olanzapine pamoate in a middle-aged female. Indian J Psychiatry. 2017;59(4):517-519.
- [Google Scholar]
- Postinjection delirium/sedation syndrome after 31st long-acting olanzapine depot injection. Clin Neuropharmacol. 2019;42(2):64-65.
- [Google Scholar]
- Refractory delirium tremens: a case report and brief review. Innov Clin Neurosci. 2012;9(3):19-22.
- [Google Scholar]
- Lorazepam precipitated alcohol withdrawal delirium - two case report. Asian J Psychiatr. 2017;30:98-99.
- [Google Scholar]
- Genital self mutilation in alcohol withdrawal state complicated with delirium. Indian J Psychol Med. 2011;33(2):188-190.
- [Google Scholar]
- Delayed-onset delirium tremens - a diagnostic and management challenge. Acta Neuropsychiatr. 2008;20(3):152-156.
- [Google Scholar]
- Alcoholic delirium tremens with hollow viscus perforation scheduled for emergency laparotomy. Indian J Anaesth. 2012;56(2):189-192.
- [Google Scholar]
- Opioid withdrawal presenting as delirium and role of buprenorphine: a case series. Indian J Psychol Med. 2017;39(5):665-667.
- [Google Scholar]
- Opium withdrawal delirium: two case reports. Psychopharmacol Bull. 2017;47(1):48-51.
- [Google Scholar]
- A rare case of complicated opioid withdrawal in delirium without convulsions. Indian J Psychol Med. 2017;39(2):191-193.
- [Google Scholar]
- A case report on varenicline induced delirium in an alcohol and nicotine dependent patient. Indian J Psychol Med. 2015;37(3):355-357.
- [Google Scholar]
- Dependence syndrome and intoxication delirium associated with zolpidem. Natl Med J India. 2007;20(4):180-181.
- [Google Scholar]
- Identification and management of delirium in a preschooler with nephrotic syndrome. J Indian Assoc Child Adolesc Ment Health.. 2008;4:71-72.
- [Google Scholar]
- An unusual presentation of chronic lymphocytic leukaemia as delirium. Archives of Mental Health.. 2017;18:144. Pradeep J.
- [Google Scholar]
- Delirium in Parkinson’s disease: a cocktail diagnosis. J Clin Diagn Res. 2016;10(12):OD15-OD16.
- [Google Scholar]
- Pseudocyst pancreas with delirium in a married alcohol dependent male: a rare presentation. Indian J Psychol Med. 2017;39(2):196-198.
- [Google Scholar]
- Sepsis associated delirium mimicking postoperative delirium as the initial presenting symptom of urosepsis in a patient who underwent nephrolithotomy. World J Clin Cases. 2016;4(5):130-134.
- [Google Scholar]
- Tuberculous meningitis masked by delirium in an alcohol-dependent patient: a case report. Acta Psychiatr Scand. 2005;112(6):478-479, discussion 480.
- [Google Scholar]
- Multiple-etiology delirium and catatonia in an alcoholic with tubercular meningoencephalitis. Ind Psychiatry J. 2011;20(2):139-141.
- [Google Scholar]
- Hyperactive delirium and bilateral ptosis: bilateral thalamic infarcts due to artery of Percheron occlusion. J Assoc Physicians India. 2019;67(12):77-78.
- [Google Scholar]
- Prolonged delirium secondary to hypoxic ischemic encephalopathy following complete hanging. Archives of Mental Health.. 2013;14:174.
- [Google Scholar]
- Protracted delirium tremens and the forgotten cation: a case report. Asian J Psychiatr. 2018;38:29-30.
- [Google Scholar]
- Delirious mania in geriatric age: a rare presentation. J Geriatr Ment Health.. 2015;2:112.
- [Google Scholar]
- Identification and management of “delirious mania:” a rare clinical entity. Ind Psychiatry J. 2018;27(1):151-153.
- [Google Scholar]
- Delirious mania: can we get away with this concept? A case report and review of the literature. Case Rep Psychiatry. 2012;2012:720354.
- [Google Scholar]
- Olanzapine for delirium in parkinsonism: therapeutic benefits in lieu of adverse consequences. Neurol India. 2004;52(2):274-275.
- [Google Scholar]
- Use of propofol as adjuvant therapy in refractory delirium tremens. Ind Psychiatry J. 2010;19(1):58-59.
- [Google Scholar]
- Electroconvulsive therapy in the treatment of delirious mania: a report of 2 patients. J ECT. 2010;26(4):278-279.
- [Google Scholar]
- Successful use of oxazepam in the treatment of delirium tremens. Prim Care Companion CNS Disord. 2012;14(6):14.
- [Google Scholar]
- Postoperative delirium in elderly citizens and current practice. J Anaesthesiol Clin Pharmacol. 2017;33(3):291-299.
- [Google Scholar]
- Delirium tremens: assessment and management. J Clin Exp Hepatol. 2018;8(4):460-470.
- [Google Scholar]
- Usefulness of atypical antipsychotics and choline esterase inhibitors in delirium: a review. Pharmacopsychiatry. 2011;44(2):43-54.
- [Google Scholar]
- Indian research on acute organic brain syndrome: delirium. Indian J Psychiatry. 2010;52(01):S139-S147.
- [Google Scholar]
- Postoperative anaesthetic concerns in children: Postoperative pain, emergence delirium and postoperative nausea and vomiting. Indian J Anaesth. 2019;63(9):763-770.
- [Google Scholar]
- Postoperative delirium in total joint arthroplasty patients. Gen Hosp Psychiatry. 2017;48:75.
- [Google Scholar]
- Letter to editor regarding “comparison of efficacy of haloperidol and olanzapine in the treatment of delirium”. Indian J Psychiatry. 2019;61(2):218-219.
- [Google Scholar]
- [Pharmacogenomics of sevoflurane: role in emergence delirium] (in Portuguese) Rev Bras Anestesiol. 2019;69(4):423.
- [Google Scholar]
- Delirium in geriatric patients in perioperative period–Indian perspective. J Assoc Physicians India. 2010;58:715-, author reply 715–716.
- [Google Scholar]
- Evaluation of delirium in the elderly: needs further evaluation. Geriatr Gerontol Int. 2012;12(1):171.
- [Google Scholar]
- Evidence for pharmacological management in delirium. Pharmacopsychiatry. 2012;45:164-165.
- [Google Scholar]
- Referral patterns in a consultation liaison psychiatry service in India: a comparison with the Western world. Gen Hosp Psychiatry. 2019;59:76-77.
- [Google Scholar]
- Dexmedetomidine and postoperative delirium: decoding the evidence! J Anaesthesiol Clin Pharmacol. 2020;36(1):140-141.
- [Google Scholar]
- Delirium: another factor when considering type of anesthetic for hip fracture surgery in adults. BMJ. 2014;349:g4871.
- [Google Scholar]
- How can we avoid delay in referrals of patients with delirium. Indian J Psychiatry. 2014;56(3):309-310. ?
- [Google Scholar]
- Delirium-most prevalent mental disorder: still a clinical orphan? J Geriatr Ment Health.. 2014;1:57.
- [Google Scholar]
- Clinical practice guidelines for management of delirium in elderly. Indian J Psychiatry. 2018;60(03):S329-S340.
- [Google Scholar]
- Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14(6):R210.
- [Google Scholar]
- Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762.
- [Google Scholar]
- Confirmatory factor analysis of the delirium rating scale revised-98 (DRS-R98) J Neuropsychiatry Clin Neurosci. 2015;27(2):e122-e127.
- [Google Scholar]
- Profile of patients seen in consultation-liasion psychiatry in India: a review. Indian J Psychol Med. 2019;42(6):503-512.
- [Google Scholar]
- Delirium and antipsychotics: a systematic review of epidemiology and somatic treatment options. Psychiatry (Edgmont Pa). 2008;5(10):29-36.
- [Google Scholar]
- “Delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:106.
- [Google Scholar]
- Preserve and strengthen family to promote mental health. Indian J Psychiatry. 2010;52(2):113-126.
- [Google Scholar]







