Translate this page into:
Delayed incidental diagnosis of postoperative extradural hematoma following ventriculoperitoneal shunt
Address for correspondence: Prof. Bhadrinarayan Varadarajan, Department of Neuroanaesthesia, National Institute of Mental Health and Neurosciences, Bangalore - 560 029, Karnataka, India. E-mail: n_bhadri@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Ventriculo peritoneal (VP) shunt uncommonly complicates as intracranial hematomas which can still occur in patients with a functioning VP shunt leading to a delay in the diagnosis which can be extremely dangerous and lead to adverse outcomes. We report a case of an incidental diagnosis of delayed post-operative EDH following VP shunt in an young adult patient with a right cerebellar lesion and highlight the need for meticulous post-operative neurological examination.
Keywords
Extradural hematoma
ventriculoperitoneal shunt
young adult
Introduction
Ventriculoperitoneal (VP) shunting is a common procedure done for the treatment of hydrocephalus, and is associated with fewer complications as compared to other methods of ventricular decompression[1] and include shunt obstruction, infection, development of craniosynostosis, microcephaly, and excessive drainage of cerebrospinal fluid (CSF) leading to intracranial hematomas (subdural, epidural, and intraventricular). Among the intracranial hematomas, subdural hematomas (SDHs) are more common than extradural hematomas (EDHs).[2]
We are reporting a case of an incidental diagnosis of delayed postoperative EDH following VP shunt placement in an adult patient with a right cerebellar lesion. We shall also discuss the possible role of the shunt in the patient remaining symptom free postoperatively.
Case Report
A 24-year-old male presented with complaints of headache of 8 months duration and blurring of vision of 1 month duration. On examination, he was conscious and oriented, with a right hemiparesis, right lower motor neuron facial palsy, bilateral cerebellar signs, and papilledema. Systemic examination was normal. Initial computed tomography (CT) scan brain (contrast) showed heterogeneous mass lesion in the right cerebellar region, extending to the brain stem with peripheral enhancement and obstructive hydrocephalus Figure 1a and b]. Since the patient had signs and symptoms of raised intracranial pressure due to obstructive hydrocephalus, surgeons planned for left VP shunt insertion (medium pressure, Chhabra “slit spring” hydrocephalus shunt system; G Surgiwear Limited, Shahjahanpur, India). Under general anesthesia, the patient was positioned supine with head turned to right on a head ring. Parts were painted and draped. Left Frazier's point was marked (4 cm lateral to the midline and 6 cm above the inion). A curved incision was given around the Frazier's point and the scalp layer reflected. A burr hole was made and the dura coagulated. Ventricles were hit in the first attempt and the chamber was secured. After achieving hemostasis, the scalp was closed. Postoperatively, the patient was conscious and oriented, and remained symptom free for 3 days. On the third postoperative day following the shunt insertion, magnetic resonance imaging (MRI) brain was planned to evaluate the posterior fossa lesion. MRI brain showed a large left temporoparietal EDH [Figure 1c and d]. In spite of the large EDH, the patient was asymptomatic. The patient was shifted immediately to the operating room and the extradural hematoma was evacuated. Postoperatively, the patient was conscious and oriented with no fresh deficits. The postoperative CT scan brain revealed complete evacuation of hematoma with VP shunt tip in situ [Figure 2]. On questioning, the patient revealed that he had mild headache of the left hemicranium of 2 days duration, but neglected it and regular clinical examination had not revealed any pupillary asymmetry to suspect an intracranial lesion.
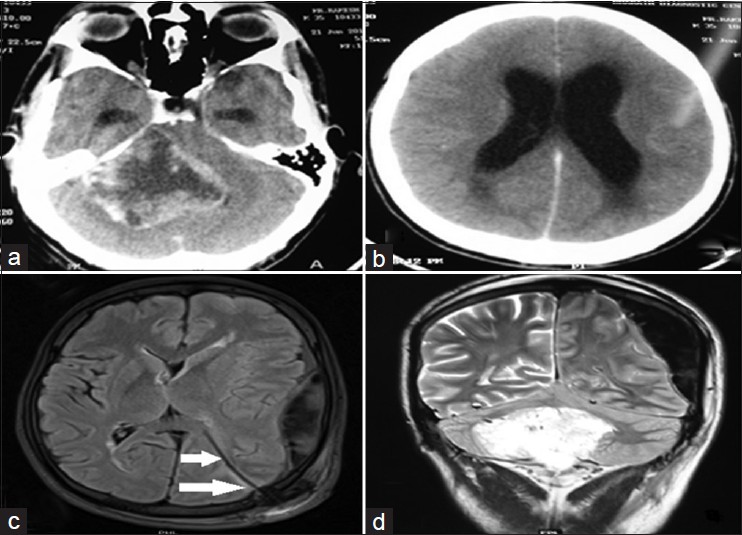
- (a and b) Preoperative computed tomography scan showing heterogeneous mass lesion in the right cerebellar region extending to the brain stem at the pontine region with peripheral enhancement on contrast and obstructive hydrocephalus. (c) Postoperative MRI on day 3; EDH in the right temporoparietal region on T2‑weighted image along with the shunt tip in situ (arrows). (d) Postoperative MRI on day 3 showing hyperintense image in the right cerebellar region along with EDH
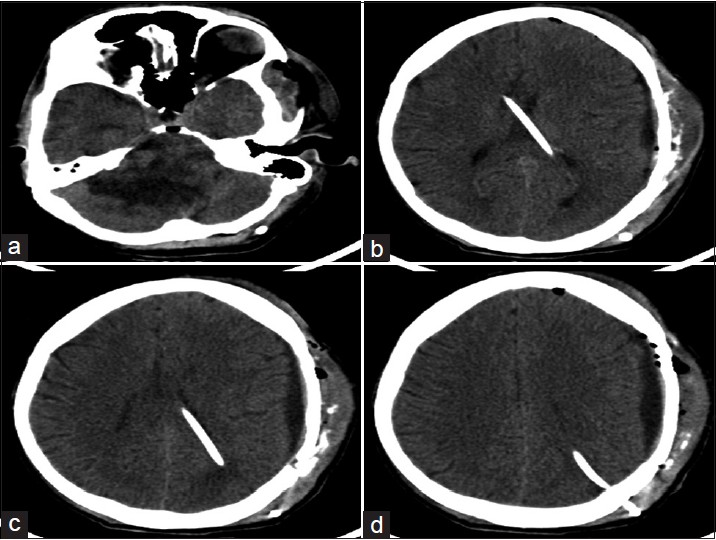
- Postoperative plain computed tomography scan brain: (a) Plain CT scan brain showing the mass lesion in the right cerebellar region; (b-d) plain CT scan brain showing the evacuated hematoma with the shunt tube in situ
Discussion
EDH is an uncommon but a dangerous recognized complication after shunt surgery. In a review by Fukamachi et al. of 1055 postoperative CT scans of patients who underwent intracranial surgery,[3] the incidence of EDH due to ventricular shunting or drainage procedures was estimated to be about 0.4%. PubMed search revealed only four reported cases of EDH following valve-regulated shunt surgery suggesting the rarity of this complication.[4567] Amongst the reported cases, shunt was the only surgery in two case reports,[45] whereas in other two reports, after shunt surgery, the patient underwent air ventriculogram[6] and posterior fossa exploration,[7] which led to decreased intracranial pressure and epidural bleeding. Further, in most reported cases including ventricular drainage procedures, the common factors associated with EDHs and CSF drainage were young patients, chronic hydrocephalus, and surgery in prone position.[8]
The mechanism of EDH development essentially requires two factors: A source of bleeding and separation of the dura from the cranium. A sudden fall in intracranial pressure after craniotomy or ventricular drainage can lead to separation of dura in some places, and the traction can lead to tearing of bridging veins/emissary veins leading to hematoma formation.[2] Some cases of postoperative EDHs may be due to inadequate hemostasis during surgery. Postoperative extradural hematomas after shunt surgery are mostly seen in young adults and children as the dura is loosely attached to calvarium in these groups of patients.[2] In our patient, the rapid reduction in intracranial pressure due to CSF drainage could have led to separation of dura from the cranium.
The other possible implications might be:
-
Coexistent bleeding disorder[8]
-
Disruption of an intracerebral vessel
-
Hemorrhage from an occult dural vascular malformation and head trauma occurring shortly after shunt placement.
But in our patient, we ruled out coexisting bleeding disorders based on clinical history, and since the shunt was inserted at the first attempt without any trauma, possibility of cerebral injury is rare. Also, there was no history of trauma in the immediate postoperative period.
The symptoms following the development of acute EDH develop very rapidly. However, patients can remain asymptomatic in small and slowly developing hematoma, leading to delayed clinical signs and symptoms.[9] Our patient, apart from having mild headache, was asymptomatic and did not evoke any suspicion. When the diagnosis of EDH would have been made in this patient if the MRI brain had not been done is debatable, as he remained asymptomatic. The factors that may explain this silent clinical course are the following:
-
The presence of a functioning VP shunt might have offset any acute rise in intracranial pressure leading to absence of symptoms
-
Hematomas located over the temporal region and posterior fossa produce significant mass effect and midline shift of brain leading to early onset of neurological symptoms and signs, but the hematoma in the frontoparietal convexity tends to spread along the whole hemisphere or even extends up to the falx leading to delayed neurological symptoms and signs, and may only appear when the hematoma reaches a large size.
Conclusion
We are reporting this case to highlight the finding that though the development of EDH following VP shunt surgery is rare, it can still occur and can be asymptomatic in patients with a functioning VP shunt, leading to a delay in the diagnosis which can be extremely dangerous causing adverse outcomes. Meticulous postoperative neurological examination and eliciting even minor symptoms like mild headache, especially in children and young adults, will help identify this condition which can lead to rapid neurological deterioration leading to a poor outcome.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Ventriculoperitoneal shunt complications in California: 1990 to 2000. Neurosurgery. 2007;61:557-63.
- [Google Scholar]
- Multiple epidural hematomas following ventriculoperitoneal shunt. Pediatr Neurosurg. 1993;19:78-80.
- [Google Scholar]
- Postoperative extradural hematomas: Computed tomographic survey of 1105 intracranial operations. Neurosurgery. 1986;19:589-93.
- [Google Scholar]
- Early epidural hematoma after CSF shunt for obstructive hydrocephalus. Neurochirurgie. 2009;55:350-3.
- [Google Scholar]
- Bifrontal epidural haematoma after shunt operation and posterior fossa exploration: Report of a case with survival. Neuroradiology. 1980;19:51-3.
- [Google Scholar]
- Massive epidural hematoma complicating ventricular decompression. Report of a case with survival. J Neurosurg. 1964;21:235-6.
- [Google Scholar]
- Fluid chronic epidural haematoma: A rare complication of ventriculo-peritoneal shunt. J Neurol Neurosurg Psychiatry. 1985;48:953-5.
- [Google Scholar]
- Spontaneous epidural hematoma following a shunt in an infant with congenital factor X deficiency. Case report and literature review. Neurosurg Rev. 1999;22:226-9.
- [Google Scholar]






