Translate this page into:
Clinical tools to assess posture in children with cerebral palsy: A systematic review
*Corresponding author: Aarti Gupta, PhD Scholar, Faculty of Physiotherapy, SGT University, Gurugram, Haryana, India. physioaarti@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta A, Rai A, Sen S. Clinical tools to assess posture in children with cerebral palsy: A systematic review. J Neurosci Rural Pract. 2024;15:525-35. doi: 10.25259/JNRP_84_2024
Abstract
Objectives:
The goal of this comprehensive evaluation of the literature is to evaluate the methodological quality of the tools available for measuring a child’s posture in relation to cerebral palsy (CP) in accordance with the consensus-based criteria for selection of health measurement instruments (COSMIN) criteria and checklist.
Materials and Methods:
The following inclusion criteria were applied while screening studies found in the PubMed, ScienceDirect, Web of Science, and Scopus databases to determine their eligibility: (1) Clinical examinations of the posture of children with CP; (2) age of 3 years or more at all gross motor function classification system levels; (3) posture evaluation measures described; (4) statistics on responsiveness, validity, and reliability for children with CP; and (5) published in peer-reviewed English-language journals. Data on study features, tool or scale characteristics, and study outcomes were evaluated and discussed. The “quality of research” was evaluated using the COSMIN.
Results:
Seven tools were found and included in this study out of 349,928 studies. Of these, three were observational measurements and four were instruments. The quality of the studies was very good in 40%, adequate in another 40%, and inadequate in the rest of the 20% studies. The evidence’s level of quality for the posture assessment tool’s measurement quality ranged from very low to low. However, none of the tools evaluated every COSMIN-recommended property. There was a lack of evidence about these measures’ responsiveness.
Conclusion:
Research on the measuring quality of tools used to evaluate posture in children with CP is scarce and of low quality. In accordance with the COSMIN guidelines, additional studies are required. The PROSPERO database has this review registered under the number CRD42022333121.
Keywords
Cerebral palsy
Posture
Consensus-based standards for the selection of health measurement instruments
Measurement properties
INTRODUCTION
Cerebral palsy (CP), the most frequent motor disability in children, is linked to a lifetime of motor impairment.[1] It is present in 2.5 out of every 1000 live births.[2] The musculoskeletal system consists of bone and soft tissues. Intrinsic factors (biochemical structure, growth potential, and physical properties) and extrinsic factors (gravity, muscle pull, and dynamic stress) act on the musculoskeletal system. An imbalance between these factors may result in bony, soft-tissue, or joint deformity or combinations. The alignment or orientation of body segments while maintaining an upright stance is known as posture.[3] For the maintenance of a normal resting posture, neuromuscular integrity has been proven to be crucial.[4] The most prevalent sign of CP is hypertonicity of the muscles due to brain injury, which is often accompanied by additional motor problems such as poor balance, coordination, and hand function.[5] Different aberrant muscular patterns, such as flaccid agonist versus a normal or spastic antagonist and normal agonist versus a spastic antagonist, are brought on by central nervous system lesions.[4] Aside from the head tilting to one side, there is a noticeable pelvic tilt and spinal scoliosis. Other common abnormalities associated with CP include windswept deformity, equinovarus foot, and knee flexion contracture. Postural deformity is closely associated with gross motor function in children with CP, and greater gross motor function classification system (GMFCS) levels are associated with more severe deformity.[6]
Human posture, which is dependent on body alignment in the sagittal, transverse, and coronal planes, alters kinetics and functions both locally and throughout the osteomioarticular chain, posing a risk to the functional health of the general public. Given the importance of maintaining the body’s kinetic and functional equilibrium through postural alignment and the increasing array of recommendations for postural assessment derived from studies in various planes, researchers have put forth methods for evaluating postural alignment such as inspection, palpation, radiographic, and photogrammetry for postural assessment[7] but all this has been done on normal population. Both research and the clinical management of CP depend heavily on the use of appropriate assessment techniques. An efficient evaluation tool should address the issue, be credible with the population that is currently of interest, have great internal validity, be easy to use, and be flexible. For many of the evaluation instruments used to evaluate people with CP, several of these requirements are not met. Furthermore, some of the tools were developed with the help of children who did not necessarily have CP. Moreover, a lot of systematic reviews on postural control have been done in the past but these studies only address postural control, that is, balance in concert with other motor functions.[8,9] A different examination is necessary for conditions such as CP to determine and assess measurements of posture or body alignment. Accordingly, the purpose of this systematic review was to apply the COSMIN recommendations to critically evaluate and summarize the measurement features of instruments used to evaluate posture in children with CP.
MATERIALS AND METHODS
Protocol and registration
In the International Prospective Registry of Systematic Reviews, the protocol for this study was entered (CRD42022333121) on June 18, 2022. This systematic review followed the COSMIN (Consensus-Based Standards for the Selection of Health Status Measures Instruments) and Parameters of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations.
Eligibility criteria
Inclusion/exclusion criteria
The following requirements were met by articles before they were included in our review: (1) Clinical examinations of children with CP’s posture; (2) analyzed a sample of children with CP older than 3 years at all GMFCS levels (as by this age, the majority of CP cases among children are diagnosed);[10] (3) posture evaluation measures dedicated, in whole or in part, to assessing posture; (4) statistics on validity, reliability, and responsiveness were provided for children with CP; and (5) published in peer-reviewed English-language journals.
Papers that satisfied any of the following requirements were not taken into consideration: (1) The tool’s primary goal was to examine motor function, not posture; the posture assessment was a subset of that examination; (2) people with CP made up fewer than 30% of the general population; (3) the articles were reviews; and (4) case studies comprised the papers.
Information sources and search strategy
We searched PubMed, Scopus, Web of Science, and Science Direct between April 20, 2022, and June 15, 2022. Finding clinical evaluation tools for posture in CP was the initial goal of the search. Both restricted terminology (MeSH) and free-text terms were used. The search word groupings representing the notions of “cerebral palsy,” “posture,” “method,” and “tool” were combined in queries using Boolean operators. Using further search parameters, all the databases were filtered to exclude reviews, animal studies, stroke, Parkinson’s disease, and research involving children under three [Supplementary material].
Measurement properties
In this systematic review, studies of reliability and construct validity were considered. A measure’s construct validity is the extent to which a patient-reported outcome measures (PROM’s) results align with theories predicated on the idea that the test accurately assesses the construct that needs to be assessed and reliability is the measure of how consistent and error-free the metric is.
Study selection and data extraction
The studies were brought into the reference manager on Endnote Desktop once a literature search was completed. The articles were gathered from each database (Web of Science, PubMed, Scopus, and Science Direct). Two reviewers (AG and AA) independently screened the publications’ titles and abstracts and compliance with the eligibility requirements. From selected studies’ reference lists, the potentially pertinent studies were looked for. In addition, the review authors (A.G., A.R.) individually assessed each full-text paper that they were able to retrieve. If there was ever a disagreement, it was settled by talking to the third reviewer (S.S.). To ensure a systematic appraisal and accurate choices, information about the author, scale/tool used, population (number of participants, age, gender, GMFCS level, and CP subtype), and measurement properties (reliability and construct validity) were extracted from each article and recorded using a Microsoft Excel spreadsheet.
Quality assessment
The criteria for consensus-based instrument selection for health assessments were employed to assess the research’s methodological quality (COSMIN).[11] The COSMIN checklist has nine measurement properties, each of which has five to eighteen elements that cover various parts of design and statistical techniques. The features of the measurements include internal consistency, reliability, measurement error, content validity, construct validity (structural validity, hypothesis testing, and cross-cultural validity), criterion validity, and responsiveness. Out of these nine measurement properties, we have chosen reliability and construct validity for quality assessment because only these two measurement properties had been mentioned in selected studies. For each of the seven properties, a study’s risk of bias is assessed on a four-point scale “very good,” “adequate,” “doubtful,” or “inadequate” (earlier, this rating system was “poor,” “fair,” “good,” or “excellent”) as per the COSMIN. The overall quality score for every measurement property was produced by taking the lowest rating of any component, also known as the “worst score counts.”[12]
RESULTS
Literature search
The PRISMA 2009 flow diagram is shown in Figure 1, which shows the studies that were used in this systematic review. A total of 349,928 articles, comprising Web of Science (16,933), PubMed (2619), Scopus (93,250), and Science Direct (237,126), were found through electronic searches. After removing duplicates, the title and abstract of the remaining articles (n = 349,886) were used to determine their eligibility. Of the 40 articles that were retrieved in full, 20 were eliminated since they did not fit the requirements. Twelve articles were excluded because of poor quality and eight articles were included in the study. Out of eight articles, three articles evaluated reliability as well as construct validity, seven articles included data on reliability and one on construct validity.
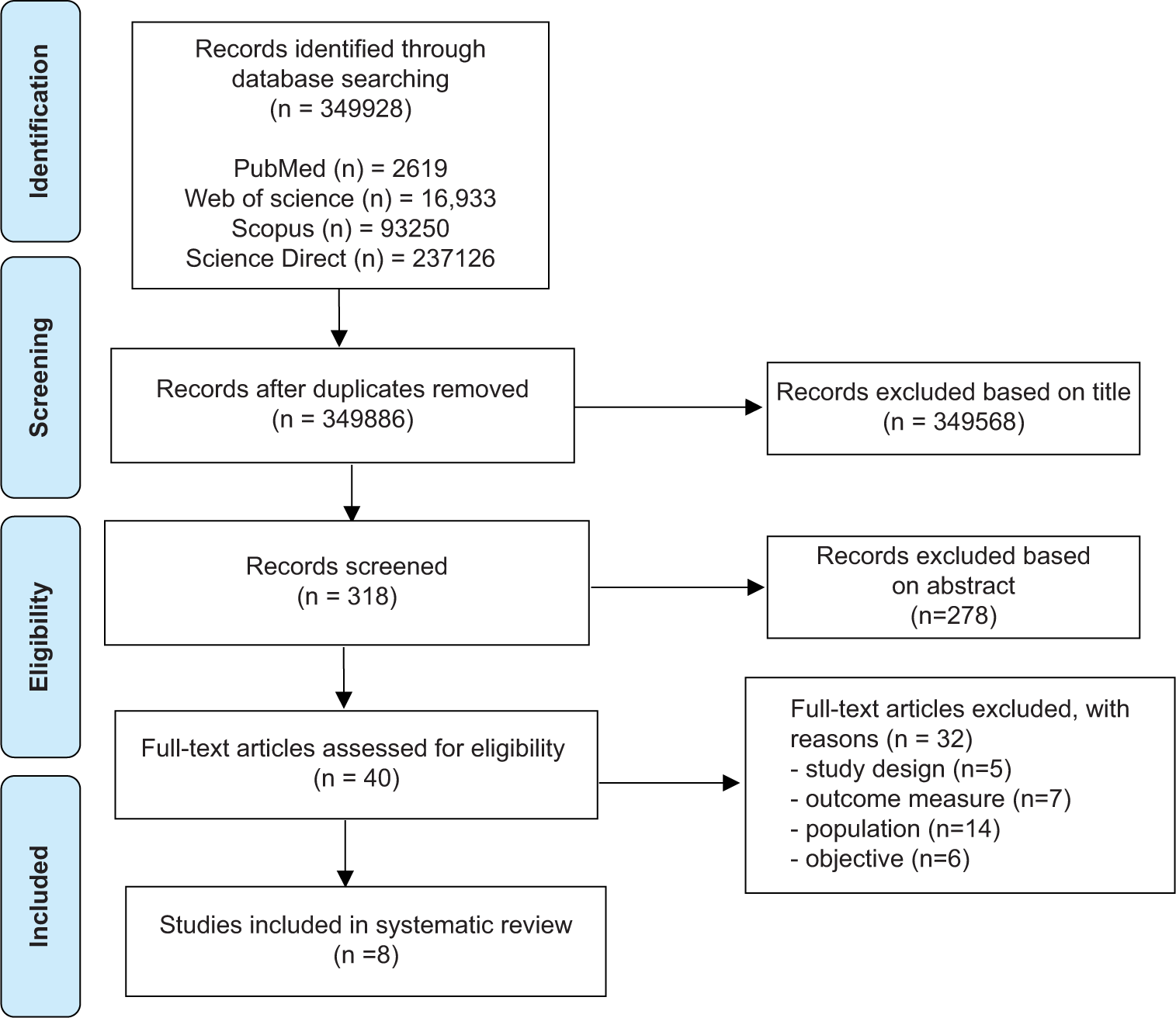
- Parameters of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart showing identification and selection of trials for the systematic review.
Generalizability
The COSMIN criteria for generalizability in Table 1 included a description of scale or tool, GMFCS level, subtype of CP, subject number according to GMFCS, age, distribution of gender, language, and country.[13] All the eight included articles[11-18] met the criteria of generalizability; however, only two studies[16,18] mentioned the CP subtype, two studies[19,20] did not mention the GMFCS level, and five studies[15,16,19-21] did not mention GMFCS level frequency.
| Measurement property | First author (Year of publication) | Scale/Tool | Population | GMFCS level | GMFCS level (frequency) | CP subtype | Country | Language | ||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Age | Gen der | ||||||||
| Reliability | Rodby-Bousquet et al., 2015 | PPAS | 29 | 6–16 years Median (12 years) | 15b, 14g | II-V | (II-10), (III-7), (1V-6), (V-6) | - | Sweden | English |
| Kim, 2021 | Smartphone application | 12 | 6–15 years Mean (9 years) | 7b, 5g | I-III | - | - | Korea | English | |
| Liu et al., 2014 | SPCM | 20 | 6–12 years Mean (9 years) | 14 b, 6 g | II-V | - | Bilateral spastic (diplegia=11, quadriplegia=9) | Taiwan | English | |
| Carmona-Pérez et al., 2020 | IMU | 24 | 4–14 years Mean (9 years) | 9b, 15g | I-IV | (I-11), (II-4), (III-1), (IV-8) | - | Spain | English | |
| Ruthard et al., 2020 | Spinal mouse | 28 | Mean (9.7 years) | 10b, 18g | 1-III | (I-2), (II-10), (III-16) | Bilateral spastic=21, Unilateral spastic=2 Dyskinetic=1, Ataxic-2, Mixed type=2 | Cologne | English | |
| George et al., 2020 | CABA | 240 | - | - | - | - | - | UK | English | |
| Field and Roxborough, 2011 | SPCM-A | 61 | 5–18 years | 28b, 23g | - | - | - | Canada | English | |
| Construct validity | Rodby-Bousquet et al., 2015 | PPAS | 29 | 6–16 years Median (12 years) | 15b, 14g | II-V | (II-10), (III-7), (1V-6), (V-6) | - | Sweden | English |
| Sadani et al., 2012 | Quantec scan | 18 | 5–11 years | - | IV-V | - | Spastic Quadriplegia=6, Spastic diplegia=1, TBI=2, Dyskinetic=4 | UK | English | |
| Carmona-Pérez et al., 2020 | IMU | 24 | 4–14 year Mean (9 years) | 9b, 15g | I-IV | I-11, II-4, III-1, IV-8 | Spastic=20, Dyskinetic=3, Ataxic=0, Mixed=1 | Spain | English | |
PPAS: Posture and posture ability scale, SPCM: Seated postural control measure, SPCM-A: Seated postural control measure-A, IMU: Inertial measurement unit, CABA: Clinical assessment of body alignment, TBI: Total body involvement, GMFCS: Gross motor function classification system, CP: Cerebral palsy
Reliability
The seven included studies[15-20] depict the reliability of posture assessment tools in children with CP as mentioned in Table 2.
| S. No. | First author (Year of publication) | Scale name | Scale Description | Method | Main Result |
|---|---|---|---|---|---|
| 1 | Rodby-Bousquet et al., 2015 | PPAS | Any deviations from the midline in the position of the head, trunk, leg, or foot, as well as any asymmetries in the arm position or weight-bearing, are scored on a scale of 0–6, with a score of 6 denoting complete symmetry, and a score of 0 being given when a person cannot be placed in a position because of severe contractures | The children were told to get in and out of standing postures as well as supine, prone, and sitting positions on a plinth. Furthermore, the children were told to sit, stand, or lie down as straight as they could in a prone or supine position. The raters concurrently documented their findings. | Internal consistency (Cronbach’s alpha=0.95–0.96) (95% CI 0.90–0.98); Corrected item-total correlation varied between 0.55–0.91 (95% CI 0.20–0.95) Inter-rater reliability (Kappa score=0.77–0.99) (95% CI 0.60–1.0) |
| 2 | Liu et al., 2014 | SPCM-A | There are 22 postural alignment items in the SPCM-A which scored using a 4-point, criterion-referenced scale. A normal alignment of each body segment receives a score of 4, whereas slightly, moderately, and severely aberrant alignments -receive scores of 3, 2, and 1 respectively. | Subjects used a unilateral joystick and a bimanual interface to operate a motorised wheelchair. To capture postural alignment and driving behavior in both unilateral and bimanual situations, two cameras were placed in front and to the wheelchair’s left. | Intra-rater reliability (ICC [3,1]=0.74 for the scores from the anterior view and 0.76 for the ratings from the lateral view) |
| 3 | Field and Roxborough, 2011 | SPCM | The SPCM is a criterion-referenced, 34-item evaluation tool There are 22 components in the SPCM-A. Each body segment's alignment is recorded using a 4-point ordinal scale that ranges from neutral to severely out-of-alignment. The majority of deviations are expressed in degrees using an inclinometer or protractor. The 12 items on the SPCM-F are scored on a 4-point ordinal scale from 1 to 4, with 1 denoting inability to commence the task, 2 or 3 denoting partial task completion, and 4 denoting successful task completion. | Participants were evaluated twice: once upon enrollment (T1) and once after 6 months (T2). At T1, the moment the SPCM was administered, a brief digital video recording (about 5 min) of the child remaining still while engaging in a reaching and/or manipulating activity was made. The SPCM and a second digital video recording were administered again at T2. After the child’s SPCM was finished, the second video recording was received, and the first session’s video recording had been viewed, the parent was requested to finish the parent version of the Global Change Scale during the second visit (GCS). After watching the T1 and T2 recordings of each subject, two competent pediatric therapists independently completed the therapist’s version of the GCS for each subject. | Inter-rater reliability for SPCM-A was 0.996 (CI950.991–0.998). |
| 4 | Carmona-Pérez et al., 2020 | A new cervical posture test based on IMU technology | IMUs have a microcontroller coupled to an accelerometer, gyroscope, and magnetometer that can be used to record orientation. | An IMU Shimmer3 ®sensor was put on the subject’s forehead and it recorded orientation in three planes of motion at 50 hz while watching a video. | Test-retest reliability (ICC=0.82–0.94) (CI950.595–0.941). |
| 5 | Ruthard et al., 2020 | Spinal mouse | The SM measurement is a computer-assisted measurement technique that examines and visualizes the abnormal postures and mobility of specific spinal segments in both the frontal and sagittal planes. A wheel at the device’s base records the spine’s length, and a 150 Hz potentiometer gauges angles with respect to the vertical. | Two measurements were taken while the children sat on a chair, one in the frontal plane (FSU) and one in the sagittal plane (SSU). TS, LS, Inc, and SL were all evaluated as part of the spinal evaluation | Intra-rater reliability SSU TS 0.83 (CI950.63–0.92) LS 0.93 (CI950.85–0.97) Inc 0.7 (CI950.33–0.86) SL 0.99 (CI950.97–0.99) FSU TS 0.78 (CI950.54–0.89) LS 0.87 (CI950.71–0.94) Inc 0.69 (CI950.33–0.86) SL 0.96 (CI950.90–0.98) |
| 6 | Kim, 2021 | Inclinometer linked to a bubble-level android smartphone | Pelvic rotation was measured using a clinometer connected to an android smartphone with a bubble-level app. With a positive score for anterior pelvic rotation and a negative score for posterior pelvic rotation, it visually measures tilt. | In three different positions—sitting, standing, and one-legged standing—pelvic rotation was measured with a smartphone put on children’s backs along a line joining S1 and S2. | Test-retest reliability sitting=0.95 (P<0.001); standing=0.94 (P<0.001); one-leg standing=0.85 (P=0.002) |
| 7 | George et al., 2020 | CABA | CABA posture classifications employed a 0-–3-point scoring system, with 0 denoting a position that was within 5° of the ideal alignment on either side, and 3 denoting the position that deviated the greatest from the ideal alignment. | A survey was issued to 283 pediatric physical therapists seeking their professional opinions. Participants evaluated items to see whether they matched the body alignment domain or not. |
Inter-rater reliability (Fleiss kappa=0.422; 95% CI, 0.33–0.51;P<0.005) |
PPAS: Posture and posture ability scale, SPCM: Seated postural control measure, SPCM-A: Seated postural control measure-A, IMU: Inertial measurement unit, CABA: Clinical assessment of body alignment, FSU: Frontal sitting upright, SSU: Sagittal sitting upright, LS: Lumbar spine, Inc: Inclination, TS: Thoracic spine, SL: Spine length, CI: Confidence interval, GCS: Glasgow Coma Scale
The Seated Postural Control Measure-A (SPCM-A) achieved excellent inter-rater reliability. Its ICC (3, 1) was reported as 0.996 (confidence interval [CI]95 0.991–0.998).[20] Inter-rater reliability was adequate for the Posture and Posture Ability Scale (PPAS) and Clinical Assessment of Body Alignment (CABA). Three independent raters were used in the PPAS, which showed inter-rater reliability with weighted kappa values of 0.77–0.99 (95% CI 0.60–1.0).[14] In CABA, Fleiss kappa was 0.422; 95% CI, 0.33–0.51; P < 0.005.[19] Intra-rater reliability was found to be excellent for computer-assisted spinal mouse instrument. The ICC computations for all variables revealed values in the frontal and sagittal planes between 0.69 and 0.99. The spine length showed ICC values mostly between 0.96 and 0.99 at both measurement sites, that is, sagittal sitting upright and frontal sitting upright.[18] With an intraclass correlation coefficient of 0.74 for the anterior view scores and 0.76 for the lateral view scores, it was determined that SPCM’s intra-rater reliability was adequate.[16] There was high internal consistency identified with Cronbach’s alpha value-0.95–0.96 in PPAS.[14] Smartphone-based pelvic rotation talked about test-retest reliability and it came out to be 0.95 (P < 0.001), 0.94 (P < 0.001), and 0.85 (P = 0.002) in the sitting, standing, and one-leg standing position, respectively.[15] In a new test using inertial measurement unit (IMU) technology to detect cervical position, test-retest reliability ranged from 0.82 to 094.[17]
Validity
The validity of tools or scales used to assess posture in children with CP was covered in three research which is reported in Table 3.[14,17,21] The Posture and Postural Abilities Scale for Children with CP showed good psychometric qualities but inadequate construct validity. To analyze the arithmetic average values provided by the raters, JonckheereTerpstra was used to assess the construct validity for known groups based on the GMFCS levels. P-value was found to be <0.001 for postural ability in all four positions, that is, supine, prone, sitting, and standing. P-value was between 0.01 and 0.009 for postural symmetry and alignment in the same four positions.[14] Sadani et al., in 2012, proved adequate construct validity using radiological and quantec spinal assessment. When compared to the Cobb angle in a supportive seating system, quantec scanning was practicable, reproducible, and showed good validity. Cobb and quantec (Q) angle differences were 0.02° (6.2°) in mean (and standard deviation).[21] Carmona-Pérez et al., in 2020, depicted inadequate construct validity using IMUs. The ability of the new test to discriminate was evaluated, as well as any correlation between the results of the new test and the functional measurements.[17]
| S. No. | First author (Year of publication) |
Scale/Tool name | Scale/Tool Description | Method | Main Result |
|---|---|---|---|---|---|
| 1 | Rodby-Bousquet et al., 2015 |
PPAS | Any deviations from the midline in the position of the head, trunk, leg, or foot, as well as any asymmetries in the arm or weight bearing, are scored from 0 to 6, with a score of 6 representing complete symmetry and a score of 0 indicating that the subject is unable to be placed in a position due to severe contractures. | The children were told to go into and out of standing postures as well as supine, prone, and sitting positions on a plinth. The children were also told to sit, stand, lie supine or prone, and do all of these things as straight as they could. The raters concurrently documented their findings. | For postural ability in the supine, prone, sitting, and standing positions, the P value was 0.001, and for frontal and sagittal ability in the same situations, it ranged from 0.001 to 0.009. |
| 2 | Sadani et al., 2012 | Quantec scan | A “spine-line” is determined by the Quantec scanner using the position of markers along the posterior spinal components to rebuild the 3D surface of the back. | Dot markers were placed at the top of the natal cleft, Venus’ dimples, the spinous processes of the T1, T12, and the vertebra at the point of the curvature on the child's exposed back. Two medical professionals used the Quantec scanner to collect six measurements of the spine topography in groups of three. | Cobb and Quantec (Q) angle discrepancies had a mean and standard deviation of 0.02° (6.2°) |
| 3 | Carmona-Pérez et al., 2020 |
IMU | IMUs have a microcontroller coupled to an accelerometer, gyroscope, and magnetometer that can be used to record orientation. | On the subject’s forehead, an IMU Shimmer® sensor was used to capture orientation in three planes of motion at 50 hz, while watching a video. Construct validity was assessed in two separate ways. (1) Between those who have CP and the control group. (2) Between the CP group’s wheelchair and non-wheelchair-using persons. | The discriminant cap/a city of the area and both the dimensions was high (AUC=0.8) |
PPAS: Posture and posture ability scale, IMU: Inertial measurement unit, AUC: Area under curve, CP: Cerebral palsy
Quality assessment
An evaluation of the listed research’s methodological quality is presented in the Table 4. The reliability and construct validity of the quality evaluation were rated using the COSMIN checklist. The articles were evaluated individually and independently, and any discrepancies were further clarified through conversation. There are a number of questions for each measurement attribute on the COSMIN checklist. The questions classified each study’s methodological quality as very good, adequate, inadequate, or doubtful. Each measurement property was rated and given a grade of sufficient (+), insufficient (−), or indeterminate (?) in accordance with Table 4’s COSMIN criteria. In reliability research, an ICC of 0.70 or more is considered sufficient, <0.70 is considered insufficient, and if ICC is not reported, it is considered indeterminate. In construct validity studies, results are categorized as sufficient if they support the hypothesis; indeterminate if the review team has not identified a hypothesis; and insufficient if they do not support the hypothesis.[11-13]
| PROM | Country (language) in which the questionnaire was evaluated | Reliability | Construct Validity | ||||
|---|---|---|---|---|---|---|---|
| n | Methodological Quality | Result (Rating) | n | Methodological Quality | Result (Rating) | ||
| PPAS | Sweden | 29 | Very good | + | 29 | Inadequate | + |
| Smartphone application | Korea | 12 | Very good | + | |||
| SPCM | Taiwan | 20 | Adequate | + | |||
| IMUs | Spain | 24 | Very good | + | 24 | Inadequate | + |
| Spinal mouse | Cologne | 28 | Adequate | - | |||
| CABA | UK | 240 | Very good | - | |||
| SPCM-A | Canada | 61 | Adequate | + | |||
| Quantec Assessment | UK | 13 | Adequate | + | |||
PPAS: Posture and posture ability scale, SPCM: Seated postural control measure, IMU: Inertial measurement unit, CABA: Clinical assessment of body alignment
Evaluation of the evidence’s quality is the following phase or summarizing all of the data for each measurement property within each PROMs against the standards for good measurement properties. The degree to which the pooled or compiled result can be trusted is determined by the quality of the evidence. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach is used to grade the quality of systematic reviews of clinical trials.[22] A modified GRADE system is used to grade the quality of the evidence as high, moderate, low, or very low depicted in Table 5.
| Instrument | Risk of bias | Inconsistency | Indirectness | Imprecision | Final |
|---|---|---|---|---|---|
| Reliability | |||||
| PPAS | 0 | 0 | 0 | −2 | Low |
| SPCM | 0 | 0 | −1 | −1 | Low |
| IMU | 0 | 0 | 0 | −2 | Low |
| Spinal mouse | −1 | 0 | 0 | −2 | Very low |
| Smartphone | 0 | 0 | 0 | −2 | Low |
| CABA | 0 | 0 | 0 | 0 | High |
| Validity | |||||
| PPAS | −3 | 0 | 0 | −2 | Very low |
| Quantec Scan | −1 | 0 | 0 | −2 | Very low |
| IMU | −3 | 0 | 0 | −2 | Very low |
PPAS: Posture and posture ability scale, SPCM: Seated postural control measure, IMU: Inertial measurement unit, CABA: Clinical assessment of body alignment
DISCUSSION
This review aimed to assess, contrast, and summarize the measuring capabilities of tools used to measure posture in children with CP by means of the COSMIN approach. Seven distinct tools in all could be located. Out of the seven tools, three tools[14,16,19,20] were observational measurements in which photo or video recording had been used to observe postural alignment, and scoring was done based on the deviations of body parts. The other four tools[15,17,18,21] were a spinal mouse, a clinometer linked to a smartphone, IMUs, and Quantec spinal assessment.
We discovered that while grading each study’s quality on a measurement property, 40% of the time the methodological quality was judged as very good, 40% as adequate, and 20% as inadequate. This may be because COSMIN uses the “worst score counts” approach to assess how well each study is rated overall, but it may also mean that studies in the future should carefully examine their technique in comparison to current norms of methodological excellence.[23]
No one instrument measures all the measurement qualities. Only three studies evaluated construct validity, which is the body of evidence supporting the interpretation of what a measure indicates. This is relevant, as many studies have been done on children and adolescents with typical development, but there are very few studies in CP that investigated posture. Furthermore, the majority of tools only assess the alignment of a single segment; there is scant support for methods that test the alignment of the entire body. The CABA scale is the only one that assesses whole-body alignment and provides researchers and clinicians with a therapeutically useful way to assess postural alignment in children with CP.[19] The SPCM also offers a checklist for assessing particular functional movement and postural alignment characteristics that are anticipated to alter due to interventions for adaptive sitting.[16,20] Internal consistency, content validity, measurement error, structural validity, cross-cultural validity/measurement invariance, and criterion validity were not assessed in the included studies.
The current review evaluates the methodological quality and findings of the included research (i.e., the reported measurement properties of each measure) to provide an overview of the overall data regarding measurement characteristics of outcome measures used to assess posture in children with CP. The methodological quality of the measurement feature research must be adequate to trust the results about the metrics utilized to evaluate an outcome.[22] Almost half of the included studies had low to fair methodological quality, despite the fact that the majority of them had positive results for the measurement attributes under investigation. This meant that the best evidence synthesis only found minimal evidence. In this context, the COSMIN ranking of the included studies’ methodological quality was particularly helpful.
Three tools were identified that were observational measurements. Methodological quality was adequate to very good for reliability in these tools. However, the rating was insufficient to sufficient. The CP diagnosis encompasses a diverse range of mobility and postural impairments that impede activity in general. As a result, it is possible that children with other subtypes of CP cannot use outcome metrics that have been verified for one subtype (such as unilateral spastic CP). Investigating the measuring characteristics of pertinent outcome measures for the various subtypes is therefore crucial. In PPAS, Rodby-Bousquet et al. took a small sample size (n = 29) which resulted in low evidence despite very good reliability. Its construct validity also came out inadequate resulting in very low evidence.[14] The SPCM had been used in two studies.[16,20] Liu et al.’s study had a particular subtype, that is, spastic CP but a small sample size(n = 34).[16] The field also used SPCM in his study, but the sample size was not mentioned in his study, and the population was not homogenous resulting in a downgrading of scores. The pooled results of these two studies came out low.[16] The CABA scale was rated as very good for reliability with high evidence.[19]
Out of the seven tools, besides observational tools, four other tools were a spinal mouse, a clinometer linked to a smartphone, IMUs, and Quantec spinal assessment. The reliability of the spinal mouse was found to be adequate, and the rating was insufficient. Despite of homogenous population, the small sample size (n = 28) made its evidence very low.[18] A new test for determining cervical position that uses IMU technology was judged as having good reliability but inadequate construct validity.[17] Its evidence also came out very low due to the small population(n = 24) and the absence of a homogenous population. A clinometer associated with a bubble-level android smartphone was used to measure pelvic rotation. Although it was rated as very good for reliability, a small population (n = 12) made its evidence low.[15] Quantec scanning had adequate construct validity, but a small population (n = 13) made its evidence very low.[21]
In general, most tools only examined one measurement property, no tool reviewed all measurement characteristics, and for at least one of the measurement qualities examined, the most of papers were deemed to have poor or questionable methodological quality. When considered collectively, these findings prevent recommendations from being made regarding the appropriate tools to utilize in clinical practice. The evidence’s grade ranges from very poor to low. Clearly, more research is required to assess the measurement capabilities of posture tools or instruments in CP patients, and this research must strictly adhere to the COSMIN recommendations.
Limitations
This study has some inherent limitations. The English language restriction is the first constraint in this review. This review has not filtered or included any scientific studies written in languages other than English. Second, we solely examined strategies suggested in published literature. As a result, our conclusions are limited by the information provided in the published literature. Third, we excluded studies from the systematic assessment of measurement features that were primarily focused on evaluating the impact of interventions. Fourth, because we were unable to locate much research for each instrument, the findings of the studies could not be summarized. In addition, the majority of the tools have only tested the reliability and construct validity of two measurement attributes.
CONCLUSION
From the eight studies included in this study, seven techniques for posture assessment were found. The CABA has the strongest level of evidence that we could find. Pediatric physical therapists, who participated in the CABA questionnaire, evaluated each item’s compatibility with the domain of body alignment. There is a need for greater research to give higher degrees of proof for the validity, reliability, and other measuring characteristics of posture assessment instruments. The technological field of postural assessment research is growing and progressing, although the majority of the studies are being done on children with typical development. Further studies are required to demonstrate these emerging technologies in children with CP.
Authors’ contributions
AA: Conceptualization, Methodology, Validation, Investigation, Data Curation, Writing – Original draft preparation, Writing – Reviewing and Editing. AR: Project administration, Supervision, Writing – Reviewing and Editing, Visualization, Investigation. SS: Supervision, Formal analysis, Validation, Resources, Visualization.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Supplementary material available on:
Financial support and sponsorship
Nil.
References
- Cerebral palsy: Clinical care and neurological rehabilitation. Lancet Neurol. 2011;10:844-52.
- [CrossRef] [PubMed] [Google Scholar]
- The reliability and validity of pain interference measures in persons with cerebral palsy. Arch Phys Med Rehabil. 2002;83:236-9.
- [CrossRef] [PubMed] [Google Scholar]
- Attributes and qualities of human posture and their relationship to dysfunction or musculoskeletal pain. Crit Rev Phys and Rehabil Med. 1994;6:409-37.
- [Google Scholar]
- The origin of prenatal and postnatal deformities. Pediatr Clin North Am. 1986;33:1277-97.
- [CrossRef] [PubMed] [Google Scholar]
- A review on recent advances of cerebral palsy. Oxid Med Cell Longev. 2022;2022:2622310.
- [CrossRef] [PubMed] [Google Scholar]
- Postural deformity in children with cerebral palsy: Why it occurs and how is it managed. Phys Ther Res. 2020;23:8-14.
- [CrossRef] [PubMed] [Google Scholar]
- Mobile applications for assessing human posture: A systematic literature review. Electronics. 2020;9:1196.
- [CrossRef] [Google Scholar]
- Clinical tools to assess balance in children and adults with cerebral palsy: A systematic review. Dev Med Child Neurol. 2013;55:988-99.
- [CrossRef] [PubMed] [Google Scholar]
- How to measure balance in clinical practice. A systematic review of the psychometrics and clinical utility of measures of balance activity for neurological conditions. Clin Rehabil. 2009;23:824-40.
- [CrossRef] [PubMed] [Google Scholar]
- A collaboration of cerebral palsy surveys and registers. Surveillance of Cerebral Palsy in Europe (SCPE) Dev Med Child Neurol. 2000;42:816-24.
- [CrossRef] [Google Scholar]
- The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: A clarification of its content. BMC Med Res Methodol. 2010;10:22.
- [CrossRef] [PubMed] [Google Scholar]
- Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Qual Life Res. 2012;21:651-7.
- [CrossRef] [PubMed] [Google Scholar]
- COSMIN methodology for systematic reviews of patient-reported outcome measures (PROMs) User Manual. 2018;78:6-3.
- [Google Scholar]
- Psychometric evaluation of the posture and postural ability scale for children with cerebral palsy. Clin Rehabil. 2015;30:697-704.
- [CrossRef] [PubMed] [Google Scholar]
- Validity and reliability of smartphone-based pelvic rotation evaluations of children with cerebral palsy while sitting, standing, and standing on one leg. J Pediatr Rehabil Med. 2021;14:295-9.
- [CrossRef] [PubMed] [Google Scholar]
- Postural alignment in children with bilateral spastic cerebral palsy using a bimanual interface for powered wheelchair control. J Rehabil Med. 2014;46:39-44.
- [CrossRef] [PubMed] [Google Scholar]
- Design, validity, and reliability of a new test, based on an inertial measurement unit system, for measuring cervical posture and motor control in children with cerebral palsy. Diagnostics. 2020;10:661.
- [CrossRef] [Google Scholar]
- Reliability of a radiation-free, noninvasive and computer-assisted assessment of the spine in children with cerebral palsy. Eur Spine J. 2020;29:937-42.
- [CrossRef] [PubMed] [Google Scholar]
- Development and content validity of the clinical assessment of body alignment for children with cerebral palsy. Pediatr Phys Ther. 2020;32:137-43.
- [CrossRef] [PubMed] [Google Scholar]
- Responsiveness of the seated postural control measure and the level of sitting scale in children with neuromotor disorders. Disabil Rehabil Assist Technol. 2011;6:473-82.
- [CrossRef] [PubMed] [Google Scholar]
- A pilot study of scoliosis assessment using radiation free surface topography in children with GMFCS IV and V cerebral palsy. Child Care Health Dev. 2012;38:854-62.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome measures evaluating hand function in children with bilateral cerebral palsy: A systematic review. Dev Med Child Neurol. 2016;58:662-71.
- [CrossRef] [PubMed] [Google Scholar]
- Pain assessment in cerebral palsy: A systematic review of measurement properties and evaluation using the COSMIN checklist. Disabil Rehabil. 2022;44:909-19.
- [CrossRef] [PubMed] [Google Scholar]






