Translate this page into:
Clinical outcomes and efficacy of transforaminal lumbar endoscopic discectomy
Address for correspondence: Dr. Cezmi Çağrı Türk, Antalya Eğitim ve Araştırma Hastanesi, Beyin Cerrahisi Kliniği, Varlık Mah, Muratpaşa, Antalya, Turkey. E-mail: drcezmiturk@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Transforaminal lumbar endoscopic discectomy (TLED) is a minimally invasive procedure for removing lumbar disc herniations. This technique was initially reserved for herniations in the foraminal or extraforaminal region. This study concentrated on our experience regarding the outcomes and efficacy of TLED.
Materials and Methods:
A total of 105 patients were included in the study. The patients were retrospectively evaluated for demographic features, lesion levels, numbers of affected levels, visual analog scores (VASs), Oswestry disability questionnaire scale scores and MacNab pain relief scores.
Results:
A total of 48 female and 57 male patients aged between 25 and 64 years (mean: 41.8 years) underwent TLED procedures. The majority (83%) of the cases were operated on at the levels of L4-5 and L5-S1. Five patients had herniations at two levels. There were significant decreases between the preoperative VAS scores collected postoperatively at 6 months (2.3) and those collected after 1-year (2.5). Two patients were referred for microdiscectomy after TLED due to unsatisfactory pain relief on the 1st postoperative day. The overall success rate with respect to pain relief was 90.4% (95/105). Seven patients with previous histories of open discectomy at the same level reported fair pain relief after TLED.
Conclusions:
Transforaminal lumbar endoscopic discectomy is a safe and effective alternative to microdiscectomy that is associated with minor tissue trauma. Herniations that involved single levels and foraminal/extraforaminal localizations were associated with better responses to TLED.
Keywords
Endoscopic discectomy
lumbar spine
revision
transforaminal
Introduction
Transforaminal lumbar endoscopic discectomy (TLED) is a minimally invasive technique for removing lumbar disc herniations. This technique was initially reserved for herniations in the foraminal or extraforaminal regions. Since, Kambin and Gellman publicized their experiences with nine patients in 1983,[1] the surgical techniques and instruments have improved. Moreover, the indications and age groups have extended such that foraminal stenosis and different herniations, including central/paracentral and even sequestrated herniations, can be targeted with this technique.[2] Depending on the level of experience, nearly all lumbar levels are within the scope of this technique, including the technically challenging L5-S1 level.[3]
In the literature, TLED is basically favored due to the success rates that are comparable to those of microdiscectomy. In addition, this method offers more advantages related to its minimally invasive nature that include reduced hospital stays, early return to work and minimal blood loss.[4] However, the critical factor for the success rate is the surgeon's experience. Familiarity with intraoperative roentgenography is particularly crucial in determining the correct level and in selecting the safe route to the herniation.[2]
In the present study, we present our institutional experience regarding transforaminal endoscopic discectomies with emphases on recurrent cases and herniations at the L5-S1 level.
Materials and Methods
A total of 110 patients underwent TLED procedures between January 2006 and February 2013 in our clinic. The patient charts were retrospectively evaluated for demographic features, lesion levels, secondary surgeries, visual analogue scores (VAS),[5] Oswestry disability questionnaire scales scores[6] and MacNab scores.[7] The outcomes were determined by direct postoperative interviews, phone calls and mailings. Five of the patients were lost to follow-up and could not be contacted by their registered phone numbers or addresses.
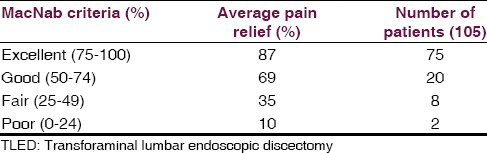
The MacNab scale scores were used as indicators of success in terms of pain relief. The scores were divided into the following four grades: 75–100% (excellent), 50–74% (good), 25–49% (fair) and 0–24% (poor). The “excellent” and “good” results were accepted as favorable outcomes, and the “fair” and “poor” results were considered unsatisfactory. A VAS was modified to inquire about pain on a scale from 0 to 10. For the Oswestry scores, the patients were asked to complete a questionnaire, and their daily life experiences were evaluated.
Surgical technique
The procedures were performed under local anesthesia and mild sedation. All patients were monitored in terms of blood pressure, pulse rate, oxygen saturation and electrocardiographic signals. The initial application of local anesthetic (prilocaine 2% and priloc 2%; Idol pharmaceuticals, Istanbul, Turkey) was performed at the needle entry site following disinfection of the surgical field. The patients were positioned lying down on the opposite side such that the lesion was facing up, and the patient was in the lateral decubitus position. After the needle was placed through the Kambin triangle using a fluoroscopic technique termed tunnel view, contrast material was injected into the intradiscal region. After verification of the level, mild sedation and analgesia were provided with fentanyl (Fentanyl ampule, Abbott pharmaceuticals, Istanbul) because enlargement of a neural foramen is painful. The compliance of the patient was affected during the sequential passage of reamers. Next, a cannula and endoscope were placed, and the nerve root was secured. Subsequently, the discectomy was performed with graspers. The patients were generally followed for two additional hours in the wards and then mobilized.
The patients were allowed to be discharged from the hospital on the same day and were called for the first follow-up 1-day later. However, for the first 60 patients, the authors preferred overnight stays and follow-ups. The time of discharge was tailored to the patient depending on his/her wishes, the experience of the physicians and center-based factors.
All of the TLED procedures were performed with the Joimax TESSYS™ endoscopic system [Figures 1 and 2]. The surgical technique has been discussed and described in various previous articles.[89] For the technical details specific to the L5-S1 level, the reader should see the Yeung and Tsou article.[3]
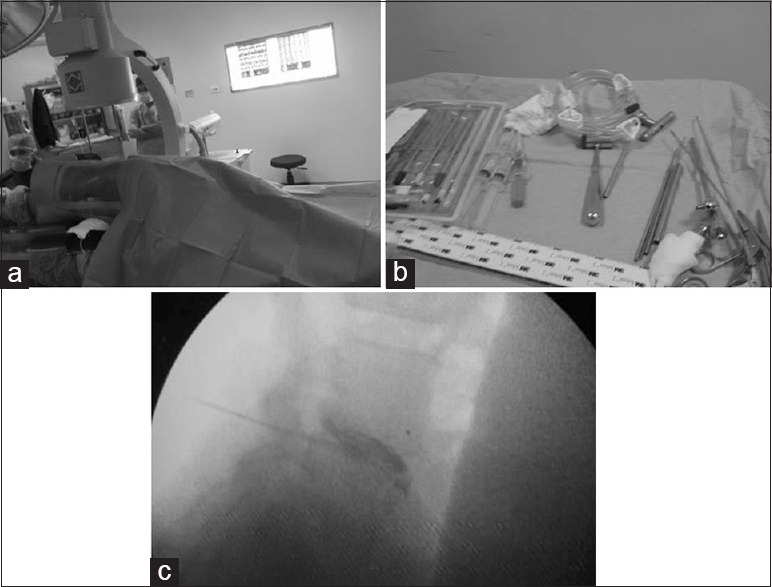
- Preoperative positioning of the patients (a) and endoscopic equipment (b) with intraoperative discography (c)
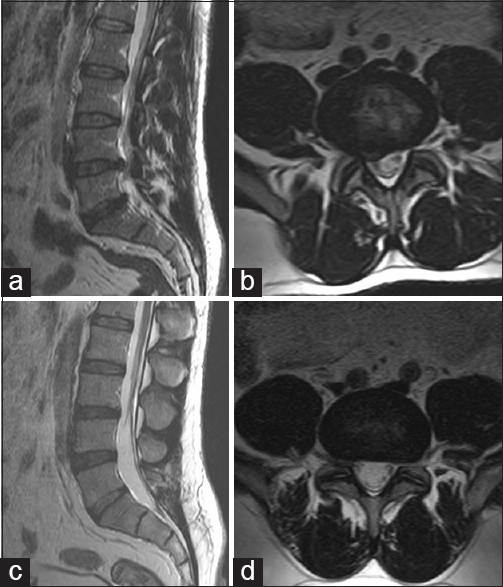
- Preoperative sagittal (a) and axial T2-weighted magnetic resonance (MR) images (b) showing a right L4-5 lumbar disc herniation. Postoperative 1-year follow-up sagittal (c) and axial T2-weighted MR images (d)
Results
A total of 105 patients were included in the study. There were 48 female and 57 male patients with ages that ranged from 25 to 64 years (mean: 41.8). Five patients had herniations at two levels, and both levels were treated with TLED in the same session. The study evaluated 105 patients and 110 TLEDs. Among these patients, 10 had undergone previous microdiscectomies for lumbar disc herniations, five of which were at the same level, three were one level above, and two were on the contralateral side.
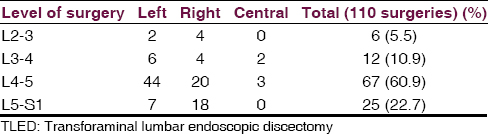
The distribution of the levels is summarized in Table 1. In the majority (83%) of the cases, the levels operated on were L4-5 and L5-S1. Among these, two consecutive segments were involved in five patients, including L4-5 and L3-4 (three patients) and L4-5 and L5-S1 (two patients). These patients underwent TLED operations on both levels.
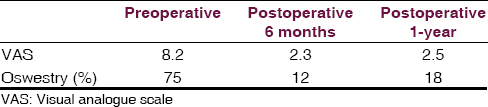
The preoperative and postoperative VAS and Oswestry scores are summarized in Table 2. The results revealed significant decreases in the preoperative VAS scores in the early postoperative period (mean: 1.7); however, after 6 months, the mean scores increased to 2.3 and remained stable at the 1-year follow-up (mean: 2.5). The scores were debatable in the patients with two-level involvements. In two patients who underwent operations at the L3-4 and L4-5 levels, the Oswestry scores were at the upper limits for minimal and moderate (18% and 16%) disabilities, that is, 60% and 62% pain relief rates. These patients had central herniations at the L3-4 level. Similarly, in an additional two patients with consecutive involvements (L4-5 and L5-S1), satisfactory changes in the VAS scores were not achieved in the postoperative period. Because the complaints were not resolved, these patients underwent re-operations with microdiscectomy 1-day later due to inadequate disc removal and lumbar stenosis. However, only one patient with two-level involvement (L3-4 and L4-5) experienced a satisfactory pain relief rate (85%).
The overall success rate for TLED in terms of pain relief was 90.4% [95/105; Table 3]. Among the eight patients who reported fair (25–49%) pain relief, seven had histories of previous open surgery at the same level (five on the same side and two on the contralateral side), and the other patient had undergone a previous operation for a paracentral disc herniation at the L4-5 level. The patients with poor MacNab scores were re-operated on with microdiscectomy.
Discussion
The indications for TLED are similar to those for microdiscectomy. The preference for TLED is primarily based on the ability to achieve similar rates of pain relief with minimal tissue trauma (i.e., to the paraspinal musculature) and less removal of normal anatomical structures (i.e., the lamina and facet joints).[10] The risk of epidural fibrosis (which occurs in approximately 10% of patients), complicating dural injuries (4% vs. 0.3%) and iatrogenic spondylolisthesis associated with TLED are decreased, and these reductions are also counted among the procedural advantages of TLED over microdiscectomy.[3] Jasper et al. reported a total complication rate of 1.2%.[2] In addition, early mobilization and early return to work provide additional motivations for TLED. However, there are some limitations to this procedure, particularly during the early phase of the learning curve of the surgeon, for example, difficulties in manipulating calcified, centrally located herniations and challenging approaches to the L5-S1 foramen.
The findings in the literature reveal comparable rates of satisfaction following TLED and microdiscectomy. Yeung and Tsou reported a rate of satisfactory results of 89%.[3] Jasper et al. achieved pain relief in 83.9% and 69.7% of their patients with single- and multilevel-disc involvement, respectively. The overall average rate reported by Jasper et al. was 71.7%, and the VAS results improved from 8.8 to 2.6 at 6 months.[2] Comparing to these series, our figures are more promising. We achieved >87% (excellent) pain relief in 71% (75/105) of the patients. In addition, good results (i.e. a mean pain relief rate of 69%) were achieved in 19% (20/105) of the patients. The rate of excellent outcomes was higher in our series, which can be attributed to rather conservative application of TLED in the early period of our experience. The procedure was preferentially indicated for single-level, largely foraminal and extraforaminal herniations. The VAS and Oswestry scores in our series were similar to those reported in the literature.
Our series also revealed an inverse correlation between the number of levels and the rate of postoperative pain relief. In two of our patients, two consecutive levels (L3-4 and L4-5) were operated on in the same session. The postoperative VAS scores decreased to 4/10 at best. The satisfaction with the procedure remained at approximately 60% with respect to the rate of pain relief (i.e. “good” on the MacNad scale). Moreover, the Oswestry scale results were close to the threshold between minimal disability and moderate disability (16–18% and <21–40%, respectively). This relative ineffectiveness might be attributable to our poor patient selection, specifically, the selection of patients with multi-level involvement and centrally located calcified disc herniations at the L3-4 level. Sung studied the causes of poor outcomes after TLED. These authors reported an 8.3% rate of fair and poor outcomes over 800 patients.[11] The reported causes were the following: (1) Inadequate indications in 2.5%, (2) procedural problems in 2.1% (e.g. incomplete removal of the disc), and (3) re-herniations in 1.8% of the patients. In our series, the corresponding figure was 9.5%.
Revision surgeries
Transforaminal lumbar endoscopic discectomy, as a primary modality, can also be implicated in revision surgeries for recurrent herniations and can be performed either after TLEDs or following microdiscectomies.
When required, we did not elect to perform revision surgeries with the TLED technique. The revisions (two cases) were performed with microdiscectomy. Sung reported 15 cases of recurrent herniation in a series of 800 patients (1.8%).[11] Sasani's experience involving 66 patients included three recurrences (4.5%) that were later subjected to open surgery.[8] Hoogland et al.'s recurrence rates were 4.62–6.9%. Hoogland et al. reported two TLED series. In one series, 5/9 patients with early recurrences were re-operated on with microdiscectomy.[12] In contrast, in another article by Hoogland et al.,[13] 36.3% (4/11) and 63.7% (7/11) of the patients with recurrences underwent re-operation with a repeated TLED and microdiscectomy, respectively. However, Hoogland et al. favored repeated TLED for the recurrences.[13] This approach was also supported by Jasper et al. After emphasizing the comparable rates of recurrence for TLED (4.1%: 8/195) and microdiscectomy (10%), these authors reported their experiences of utilizing repeated TLED procedures and did not encounter any specified difficulties.[2]
The second issue is the use of TLED for recurrences following microdiscectomies. Yeung and Tsou presented 27 patients with histories of prior laminectomies and discectomies (8.8% of their cases).[3] These authors were still able to achieved satisfactory results in 89% of the patients. Theoretically, and in our experience, revision surgery with TLED following micro-discectomy is a good alternative because the area is accessed through an untouched site. Moreover, the risk of inadvertent damage to the neural tissue and dura can be eliminated by approaching the site without troublesome epidural fibrosis.[14] These findings were also supported by Hoogland et al., who reported excellent or good results (85%) over a 2-year follow-up. These outcomes support TLED as a convenient method for recurrent cases irrespective of the type of previous surgery.[13] In contrast to these reports, we operated on seven recurrent cases after microdiscectomy and achieved only fair outcomes. We have contemplated the roles of probable segmental instability and epidural fibrosis in addition to recurrent herniation in the clinical presentations of these patients. Without underestimating the benefit of TLED in removing the offending pathology with a minimal risk of complications, we question the efficacy in the presence of such secondary pain generators. Therefore, we favored performing TLED as first-line therapy in selected cases and then, if necessary, implementing microsurgery for recurrent cases rather than utilizing microdiscectomy first with subsequent TLED for re-herniations. More studies are needed to determine the efficacies these approaches.
Challenging L5-S1 level
A literature review suggested that the L5-S1 level can be approached with quite good outcomes. Several techniques have been described for this route.[314] Yeung and Tsou reported their TLED experiences over 307 cases; 50% of these cases were at the L5-S1 level, and these authors stated that no lumbar disc space was inaccessible.[3] In addition, incomplete decompression was reported in only 3.3% of the cases.[14] In our series, the number of cases at the L5-S1 level was comparably low, that is, only 22% (25/110) of the cases. Indeed, two of the patients had two-level disc herniations at the L4-5 and L5-S1 levels, and unfortunately, underwent additional open surgeries 1-day after TLED. The approach to the L5-S1 level was challenging particularly in the first 10 cases. However, considering our 23 cases of single-level involvement, the good outcomes and experience-based improvements in access motivated us to apply TLED in L5-S1 cases.
Conclusion
Transforaminal lumbar endoscopic discectomy is a safe, minimally invasive and effective alternative to microdiscectomy. Postoperatively, the minimal tissue trauma reduces the risk of spinal instability and epidural fibrosis, which decreases the risk of complications in secondary surgeries. Patients with single-level and foraminal/extraforaminal herniations have better outcomes; however, thorough patient selection and a careful localization of the responsible level will increase the success rates. Moreover, it is preferable to initially allow a minimally invasive and safe method for alleviating the symptoms of disc herniations a chance to succeed and then progress to into microdiscectomy when necessary.
Ethics
The work described in this article has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans; Uniform Requirements for manuscripts submitted to biomedical journals.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Percutaneous lateral discectomy of the lumbar spine. A preliminary report. Clin Orthop. 1983;174:127-32.
- [Google Scholar]
- Clinical success of transforaminal endoscopic discectomy with foraminotomy: A retrospective evaluation. Clin Neurol Neurosurg. 2013;115:1961-5.
- [Google Scholar]
- Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976). 2002;27:722-31.
- [Google Scholar]
- Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008;33:931-9.
- [Google Scholar]
- Validation of the Turkish version of the Oswestry Disability Index for patients with low back pain. Spine (Phila Pa 1976). 2004;29:581-5.
- [Google Scholar]
- Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53:891-903.
- [Google Scholar]
- Percutaneous endoscopic discectomy for far lateral lumbar disc herniations: Prospective study and outcome of 66 patients. Minim Invasive Neurosurg. 2007;50:91-7.
- [Google Scholar]
- Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: Outcome and technique. Spine J. 2002;2:41-8.
- [Google Scholar]
- Transforaminal endoscopic discectomy. In: Mayer HM, ed. Minimally Invasive Spine Surgery. A Surgical Manual (2nd ed). Berlin: Springer-Verlag; 2006. p. :315-21.
- [Google Scholar]
- A retrospective review of failed percutaneous transforaminal endoscopic discectomy. Korean J Spine. 2005;2:237-42.
- [Google Scholar]
- Transforaminal posterolateral endoscopic discectomy with or without the combination of a low. dose chymopapain: A prospective randomized study in 280 consecutive cases. In: Spine (Phila Pa 1976). Vol 31. 2006. p. :E890-7.
- [Google Scholar]
- Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: A prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976). 2008;33:973-8.
- [Google Scholar]
- Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation:Transforaminal versus interlaminar approach. Pain Physician. 2013;16:547-56.
- [Google Scholar]






