Translate this page into:
Chronic subdural hematoma: Management, sequelae with its predictive factors, and health-related quality of life of survivors
*Corresponding author: Farrukh Javeed, Department of Neurosurgery, Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan. farrukhjavedkhi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Javeed F, Shakeel A, Khan MZ. Chronic subdural hematoma: Management, sequelae with its predictive factors, and health-related quality of life of survivors. J Neurosci Rural Pract. 2024;15:566-72. doi: 10.25259/JNRP_223_2024
Abstract
Objectives:
The objective of the study is to identify the risk factors associated with chronic subdural hematoma (CSDH) in the Pakistani population, to compare various surgical techniques commonly used in its management, and to analyze the outcomes of patients, including early, that is, at the time of discharge, and late, that is, the disability status of patients on follow-up after ≥6 weeks.
Materials and Methods:
This retrospective study was carried out at a tertiary care hospital in Pakistan between March 2023 and October 2023 and included 100 patients with CSDH. All patients underwent surgical procedures, and outcomes were assessed at six weeks.
Results:
The mean age of the patients diagnosed with CSDH in this study was 53.81 ± 11.54 years. The most commonly reported symptom was an altered level of consciousness (30%), but most patients presented with more than one symptom (50%). Mortality was associated with only 10% of cases, and 90% reported no complications or significant morbidity. The most commonly used surgical technique was two burr-hole drainage (67%). The risk of recurrence was increased with the presence of comorbidities (P = 0.001) and remarkably reduced with intraoperative subdural drain placement (P = 0.000).
Conclusion:
The choice of surgical technique had no influence on the length of stay in the hospital or functional status post-discharge but surgery with intraoperative subdural drain placement proved to yield definitive favorable outcomes.
Keywords
Chronic subdural hematoma
Recurrence
Follow-up
Karnofsky score
Mortality
Two burr-hole drainage
Subdural drain
INTRODUCTION
Chronic subdural hematoma (CSDH), one of the most common intracranial hemorrhages, associated with a progressively increasing incidence, morbidity, and fatality, is actually an encapsulated collection of pathological blood in the subdural region older than two weeks or more, with external membranogenesis being its hallmark.[1] The leading precipitating factors include old age, male gender, antithrombotic therapy, history of head trauma, and any previous shunt surgery or craniotomy.[2] The best initial diagnostic modality of choice for CSDH is a non-contrast computed tomography (CT) scan of the head, demonstrating a slightly hyperdense crescent-shaped collection of fluid surrounded by neomembrane crossing suture lines, causing the midline to shift.[3]
With the advancing growth and progression of hematoma resulting in intracranial hypertension and cerebral compression, a variety of clinical manifestations appear, which may resolve after drainage or recur with rebleeding, including headache, nausea or vomiting, altered mental status, seizures, sensory or motor weakness, gait disturbance, and coma.[4] For symptomatic patients with a diagnosis of CSDH and apparent cerebral compression, surgical evacuation of the hematoma through a burr hole, twist drill openings, or craniotomy continues to be the cornerstone of management, whereas asymptomatic CSDH without cerebral compression is often treated conservatively with a window of watchful monitoring and symptomatic care, such as intracranial pressure control, anticoagulation reversal, and serial examinations.[5]
Burr hole with irrigation and closed-system subdural drainage is the most preferred surgical technique, with craniotomy being reserved for extensive hematoma, yielding rapid clinical and functional improvement in more than 80% of patients.[6] However, mortality rates of 0–32% and morbidity rates ranging from 3% to 12% have been demonstrated postoperatively, varying with the primary surgical techniques utilized. Recurrence is a serious CSDH consequence seen in up to 70% of cases, with 10–20% necessitating a redo-surgery.[7] For CSDH recurrence following primary surgery, four interpretations have been established: (1) Redo-surgery without additional clinical or radiological signs; (2) clinical symptoms with or without radiological signs warranting reoperation; (3) combination of clinical progression of symptoms and radiological recurrence or growth of ipsilateral CSDH; and (4) recurrence or progression of CSDH evident only radiologically.[8] Postoperative surgical site infections, pneumocephalus, seizures, acute subdural hematoma (SDH), and hemorrhage secondary to intracranial hypertension also pose challenges following a successful evacuation.[9]
Multiple retrospective studies have demonstrated certain variables predicting the formidable risk of morbidity, deaths, and recurrence following CSDH, including age >75 years, obesity (body mass index ≥25), poor Glasgow coma scale (GCS) status on admission, pre-existing systemic diseases, alcohol abuse, and male gender. Bilateral hematoma, decreased brain expansion intraoperatively, postoperative pneumocranium, minimum reduction in hematoma thickness, no subdural drain placement intraoperatively, size of hematoma before surgery, midline shift (MLS) ≥10 mm, drainage of hematoma ≥100 mL, location, and characteristics of hematoma are individual lesion-specific factors entailing poor outcomes.[7,10] Since re-bleeding warrants redo-surgery and has a substantial impact on functional status and quality of life postoperatively, many interventions have been proposed to reduce recurrence rates, like external subdural drain placement, which is successful in up to 50% of cases, and the use of steroids or angiotensin-converting enzyme inhibitors.[11] This wide spectrum of complications arising post-evacuation has induced dilemmas regarding surgical paradigms to avoid unfortunate outcomes. Hence, the aim of this study is to determine the association of primary management CSDH patients received in a tertiary care hospital and patient factors with post-surgical outcomes and their quality of life on follow-up at least 6 weeks after getting discharged from the hospital.
Objectives
To identify the risk factors associated with CSDH in the Pakistani population
To compare various surgical techniques commonly used in the management of CSDH
To analyze the outcomes of patients who underwent different treatment modalities, including early, that is, at the time of discharge, and late, that is the disability status of patients on follow-up after 6 weeks or more.
MATERIALS AND METHODS
This retrospective study was carried out in the Department of Neurosurgery at one of Pakistan’s largest public-sector tertiary care hospitals in Karachi after receiving approval from the institutional review board. The patients included were (1) adults of any gender, (2) diagnosed with CSDH, and (3) admitted between March 2023 and October 2023. Patients were retrospectively identified from the hospital’s patient administrative database. Patients diagnosed with acute or subacute SDH were excluded. Data were collected from their medical records and the department’s in-patient files. Study instruments include a validated questionnaire, which comprises five sections. The first section is about demographic data, including age, gender, the presence of comorbidities, history of addiction, use of anticoagulant therapy, and history of trauma. A second section presents symptoms, duration from the trauma to the onset of symptoms, duration and severity of symptoms, and arrival GCS. The third section contains characteristics of the hematoma, such as whether it was unilateral or bilateral, left or right sided, primary or recurrent, with details like size, thickness, and the presence of MLS. The fourth section includes treatment, time of surgical intervention from admission, volume of hematoma drained, subdural drain placement, and antiepileptic prophylaxis. The last section represents outcomes showing the postoperative size of the hematoma, surgical outcomes, operative complications, outcome of the patient, length of stay at the hospital, mortality rate, and GCS at discharge. Moreover, recurrence of CSDH, redo surgery, and functional performance status using the Karnofsky score were also assessed at follow-up visits at least six weeks after surgery. The data were analyzed using the Statistical Package for the Social Sciences software version 22. Chi-square, univariate, and multivariate analyses were performed to identify the relationships. A confidence interval of 95% was taken with a margin of error of 5% and a P < 0.05 as statistically significant. Any research misconduct was avoided, and the confidentiality of participants was preserved.
RESULTS
Demographic and patient-specific factors
A total of 100 patients during the study period were included retrospectively from the hospital database based on their diagnosis. The mean age of the patients diagnosed with CSDH in this study was 54.76 ± 8.77 years, with the youngest patient being 31 years and the eldest being 75 years of age. The majority of the patients, that is, 63%, were males (n = 63) and 37% were females (n = 37).
Around 58% of the patients (n = 58) had no known comorbidities. However, 29% of patients (n = 29) were hypertensive before the diagnosis, and 3% had diabetes (n = 3) and chronic kidney disease (CKD) (n = 3), whereas seven patients had both preexisting diabetes mellitus and hypertension at the time of diagnosis (7%).
The majority of the patients, i.e., 90% (n = 90), had no history of taking any blood thinners. However, 87% of the patients (n = 87) had a history of identifiable trauma precipitating CSDH progression, and the onset of symptoms was most commonly, 50% (n = 50), apparent after six weeks of afflicting trauma, followed by 4–6 weeks (26%, n = 26) and <4 weeks (10%, n = 10).
Clinical presentation
The most commonly reported symptom was an altered level of consciousness (30%, n = 30), as illustrated in Figure 1, followed by headache (10%, n = 10); however, the major subset of the cohort presented with more than one symptom (50%, n = 50).
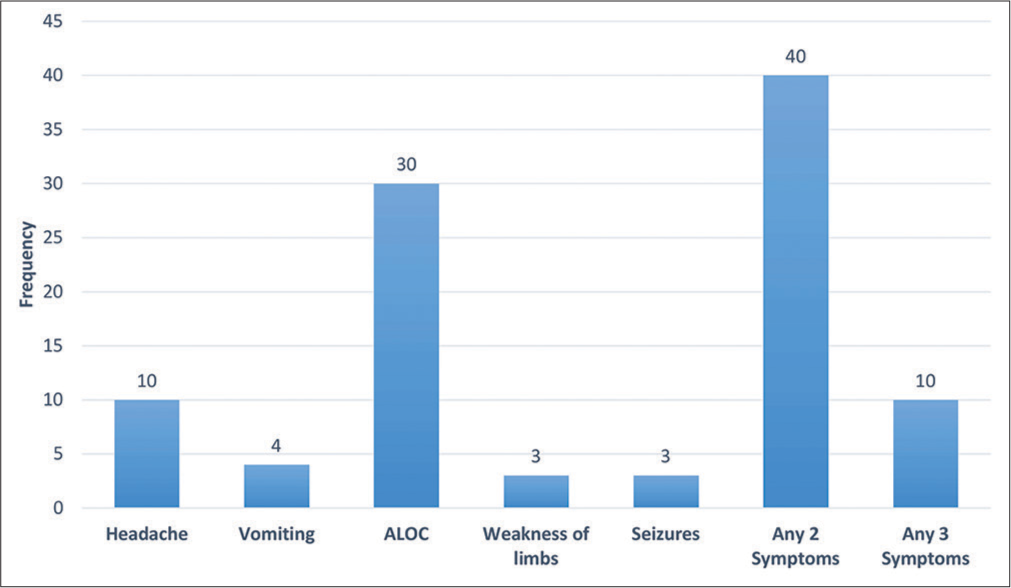
- Presenting symptoms of the patients diagnosed with chronic subdural hematoma. ALOC: Altered level of consciousness.
The duration of symptoms was mostly less than a week in 73% of the patients (n = 73), followed by a duration of 1–2 weeks (20%) and more than two weeks (7%). Furthermore, the most commonly recorded GCS at the arrival of patients was 15 (38%, n = 38), followed by a GCS ranging from 11 to 14 (34%, n = 34) and 6 to 10 (28%, n = 28).
Serial CT scans were done in all of the patients (100%, n = 100), which revealed 90% (n = 90) of unilateral CSDH, as demonstrated in Table 1, predominantly on the left side (47%, n = 47), whereas in 43% of the patients (n = 43), CSDH was found to be on the right side, and bilateral CSDH was found in only 10% of cases. The size and thickness of the hematoma were most commonly reported as >50 mL (74%, n = 74) and <20 mm (61%, n = 61), respectively, with a MLS of <10 mm in 73% of the patients (n = 73) and 10 mm or more in 27% (n = 27). The prevalence of recurrent SDH was only 7% among all patients; hence, the majority of patients (93%) were diagnosed for the first time.
| Characteristics of hematoma | Frequency | Percentage |
|---|---|---|
| Unilateral/bilateral | ||
| Unilateral | 90 | 90 |
| Bilateral | 10 | 10 |
| Primary/recurrent | ||
| Primary | 93 | 93 |
| Recurrent | 7 | 7 |
| Side of CSDH | ||
| Left | 47 | 47 |
| Right | 43 | 43 |
| Both | 10 | 10 |
| Size of CSDH | ||
| <15 mL | 0 | 0 |
| 15–30 mL | 1 | 1 |
| 31–50 mL | 25 | 25 |
| >50 mL | 74 | 74 |
| Thickness of CSDH | ||
| <20 mm | 61 | 61 |
| 20 mm or more | 39 | 39 |
| Midline shift | ||
| <10 mm | 73 | 73 |
| 10 mm or more | 27 | 27 |
CSDH: Chronic subdural hematoma
Surprisingly, mortality was associated with only 10% of cases (n = 10), and the majority of the patients reported no complications or significant morbidity (87%, n = 87). Nevertheless, the formation of an acute hematoma was reported in three patients (3%) and the recurrence of CSDH in 6% (n = 6).
Treatment
All of the patients included in this study (100%) were managed surgically, and the most commonly used surgical technique was two burr-hole drainage (67%, n = 67), followed by single burr-hole drainage (20%, n = 20), and the least opted was craniotomy (13%, n = 13). Among them, 84% (n = 84) were operated on the same day of admission and the remaining (16%, n = 16) on the first day after admission. Less than 100 mL of hematoma was drained in 67% of patients (n = 67), and 100 mL or more was drained in 33% of patients (n = 33). A subdural drain was placed intraoperatively and seizure prophylaxis was given in 93% of cases (n = 93).
Outcome
Statistically, 86% of the patients exhibited favorable outcomes after surgery (n = 86), as shown in Table 2, whereas only 14% showed unfavorable post-operative outcomes (n = 14). Of these 14 patients, 10 died during the hospital stay, 2 developed limb weakness on the contralateral side, and 2 developed post-operative seizures. Moreover, 90% of the patients were stable and discharged (n = 90), whereas mortality was reported to be only 10% (n = 10). The length of stay in the hospital was <3 days in 70% of patients (n = 70), whereas 27% stayed for 3–7 days (n = 27) and three patients stayed more than a week (3%). The GCS at discharge was strikingly 15/15 in 80% of the patients (n = 80), and post-discharge functional status at follow-up according to the Karnofsky score was 80–100 in 70% of them (n = 70). The choice of surgical technique had no influence on the length of stay in the hospital (P = 0.062) or functional status post-discharge (P = 0.109). Moreover, the overall outcome was favorable in most of the patients (86%) but it showed no statistically significant relation with the type of surgical treatment (P = 0.319).
| Treatment | Outcome | Total (%) | P-value | |
|---|---|---|---|---|
| Favorable (%) | Unfavorable (%) | |||
| Single burr-hole drainage | 19 (95.0) | 1 (5.0) | 20 (100.0) | 0.319 |
| Two burr-hole drainage | 57 (85.1) | 10 (14.9) | 67 (100.0) | |
| Craniotomy and drainage | 10 (76.9) | 3 (23.1) | 13 (100.0) | |
| Total | 86 (86.0) | 14 (14.0) | 100 (100.0) | |
CSDH: Chronic subdural hematoma
Prognostic factors for recurrent CSDH
Upon comparing the risk of recurrence with demographic variables, recurrence was established in male participants, but unconventionally, no linear correlation was found with the age and gender of the participants (P = 0.215 and 0.481, respectively). The use of anticoagulant therapy (P = 0.435) and GCS at arrival (P = 0.063) had no role in the recurrence of these patients. However, the presence of comorbidities was found to be statistically correlated with recurrent CSDH (P = 0.005).
Although left-sided CSDH and a size of more than 50 mL predisposed to recurrence, the characteristics of the hematoma, whether it was unilateral or bilateral (P = 0.70), side of CSDH (P = 0.82), size (P = 0.39), thickness (P = 0.08), MLS (P = 0.19), volume of hematoma drained (P = 0.62), and postoperative size (P = 0.58), also had no linear correlation with the recurrence of CSDH. The type of surgical technique used (P = 0.4) and seizure prophylaxis (P = 0.48) had no statistically significant relationship, but duration from arrival to surgery (P = 0.00) and intraoperative subdural drain placement (P = 0.00), had a major impact on recurrence, as shown in Table 3.
| Subdural drain placement | Recurrence | Total (%) | P-value | ||
|---|---|---|---|---|---|
| Yes (%) | No (%) | Not applicable (%) | |||
| Yes | 3 (3.2) | 82 (88.2) | 8 (8.6) | 93 (100.0) | 0.000 |
| No | 3 (42.9) | 2 (28.6) | 2 (28.6) | 7 (100.0) | |
| Total | 6 (6.0) | 84 (84.0) | 10 (10.0) | 100 (100.0) | |
CSDH: Chronic subdural hematoma
Factors accelerating the mortality rate
Likewise, the associated mortality rate in this cohort of CSDH was not statistically related to age (P = 0.56), gender (P = 0.24), use of anticoagulants (P = 0.26), or GCS at arrival (P = 0.15) but shared a significant linear correlation with the coexisting diseases (P = 0.001), as given in Table 4. Subsequently, the risk of mortality was not exacerbated by the side (P = 0.88), size (P = 0.14), drained volume (P = 0.62), or MLS (P = 0.08) of the hematoma but was statistically related to the presence of comorbidity (P = 0.001) and thickness of the hematoma (P = 0.034).
| Characteristics | Mortality | Total (%) | P-value | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Comorbidities | ||||
| HTN | 3 (10.3) | 26 (89.7) | 29 (100.0) | 0.001 |
| DM | 0 (0.0) | 3 (100.0) | 3 (100.0) | |
| CKD | 0 (0.0) | 3 (100.0) | 3 (100.0) | |
| None | 3 (5.2) | 55 (94.8) | 58 (100.0) | |
| >1 | 4 (57.1) | 3 (42.9) | 7 (100.0) | |
| Thickness of hematoma | ||||
| <20 mm | 3 (4.9) | 58 (95.1) | 61 (100.0) | 0.034 |
| ≥20 mm | 7 (17.9) | 32 (82.1) | 39 (100.0) | |
CSDH: Chronic subdural hematoma, HTN: Hypertension, DM: Diabetes mellitus, CKD: Chronic kidney disease
DISCUSSION
This study aims to identify various factors and their effects on the prognosis of patients with CSDH that took place in a public sector hospital in Karachi and is among the very few studies done in Pakistan on this topic. The majority of the patients, that is, 63%, were males, and 37% were females. The age group of patients was between 31 and 75 years, with an average of 54.76 years. Old age, along with the male gender, has been a potential risk factor for CSDH, which is supported by the literature.[12] Most of the patients had no known comorbidities. The most common comorbidity was hypertension, similar to a retrospective study done in Italy, while, in contrast to this study, the second most common comorbidities were diabetes and CKD.[13] The majority of the patients (87%) had a history of trauma, and the time duration between the trauma and the onset of symptoms was more than 6 weeks in half of the patients (50%), followed by 4–6 weeks in 26% of the patients, while only 10% presented within four weeks. Almost all the patients presented after three weeks of trauma, which favors a literature review, but it also states that with increased use of anticoagulants, CSDH can occur in the absence of any identifiable trauma, which contradicts our finding, which shows trauma to be the single most common precipitant for CSDH development.[14]
Clinically, most of the patients presented with more than one symptom, while an altered level of consciousness was the most common symptom reported. This is contrary to a study where headache was the most common presenting symptom.[15] The arrival GCS of the patient was also recorded for comparison with postoperative discharge, and strikingly, it was 15 in the majority of our patients (38%), while 34% had a GCS ranging between 11 and 14 which is supported by research where the majority of patients had an arrival GCS of 13–15.[16]
Our findings on the proportion of unilateral vs. bilateral CSDH were similar to most of the studies done previously. The majority of our patients had CSDH, which was 90% unilateral, while only 10% were bilateral on CT scans. Unilateral CSDH was slightly more common on the left side as compared to the right.[17] The age and gender of the patients did not influence recurrence. Surprisingly, GCS at the arrival of patients and the use of blood thinners also played no role in recurrence, which were proven to be predictors of recurrence previously by studies.[12] However, we found the presence of comorbidities to be a potential risk for recurrence, similar to a Sub-Saharan African study that referred to hypertension as the accelerating factor.[18] The size of the hematoma also has an impact on recurrence. Larger hematomas have a higher recurrence rate as compared to smaller hematomas. In our study, we found that hematomas >50 mL were at risk for recurrence.
The most commonly chosen surgical treatment was two burr-hole drainage, followed by single burr-hole drainage, and the least common was craniotomy. We did not find that surgical intervention, particularly two burr-hole drainage, yielded favorable outcomes postoperatively which has been strongly supported by the literature.[12] 84% of the patients had undergone surgery on the same day of presentation, while the remaining cases were operated on 1 day after admission. Our results showed that the shorter the time from arrival to surgery, the lesser the risk of recurrence, contradicting a study. The length of hospital stay was <3 days for 70% of the patients, while others stayed for 3–7 days or more. This remarkably reduced hospital stay can be explained by this study, which found that length of stay at the hospital is directly associated with the time of admission to the time of surgery but has no effect on outcome.[19] Seizure prophylaxis was also given to 93% of our patients because postoperative seizures can lead to increased mortality.[20]
Most patients showed favorable outcomes at the time of discharge postoperatively, with a surprising GCS of 15.[4] We followed the quality of life of patients for at least 6 weeks after their discharge. We found that favorable surgical outcomes were associated with a better quality of life. Strikingly, the majority of patients had a Karnofsky score of 80– 100.[21] It might be more helpful if we knew the pre-admission Karnofsky of these patients for comparison. Although we observed that two burr-hole drainage was associated with better functional status, we could not find any linear relationship between the two. Mortality was reported to be 10%, which was close to a study previously done that stated that the generally accepted mortality rate is usually 8%.[22] Surprisingly, we also found that mortality does not share a linear correlation with age, gender, use of anticoagulants, or GCS at arrival but with the presence of pre-existing disease and thickness of the hematoma. Research has shown that post-operative morbidity and mortality are significantly higher in those with pre-existing comorbidities. On the contrary, hematoma thickness was not associated with increased mortality, according to the above-cited study.
We could not find any linear relation between age, gender, and the use of anticoagulants with CSDH recurrence, which is contrary to this same study that describes old age, male gender, and the use of anticoagulants as potential risk factors for CSDH recurrence, which contradicts our finding. In our study, we observed that recurrence was seen in patients with known comorbidities and left-sided hematomas where the volume of the hematoma exceeded 50 mL. Additionally, we found that there was no relation between unilateral or bilateral CSDH and recurrence, which is contrary to this study that has shown bilateral CSDH to increase the risk of recurrence significantly. We found that the thickness of the hematoma also does not affect recurrence, but this is again in contrast with a study in which they found recurrence to be significantly more common in thick hematomas.[12] Similarly, we found that the type of surgical procedure had no impact on recurrence, which is supported by some studies showing no statistically significant difference in recurrence of CSDH in patients who underwent single vs. two burr-hole drainage.[23]
A subdural drain was placed in 93% of cases, which is shown to reduce the risk of recurrence and mortality.[15]
CONCLUSION
CSDH has been most prevalent in older age groups, but strikingly, it has started afflicting middle-aged men as well, with the history of trauma being the strongest precipitating factor. Two burr-hole drainage is the most trusted and frequently employed surgical technique. The choice of surgical technique had no influence on the length of stay in the hospital or functional status post-discharge but surgery with intraoperative subdural drain placement proved to yield definitively favorable outcomes. Nevertheless, a larger population-based trial and documentation of performance status before the diagnosis are needed for better comparisons.
Ethical approval
The research/study was approved by the Institutional Review Board at Jinnah Postgraduate Medical Centre, Karachi, number NO.F.2-81/2023-GENL/32/JPMC, dated March 20, 2023.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Current diagnosis and treatment of chronic subdural haematomas. J Med Life. 2015;8:278-84.
- [Google Scholar]
- Predictive factors for recurrence and clinical outcomes in patients with chronic subdural hematoma. J Neurosurg. 2017;127:1117-25.
- [CrossRef] [Google Scholar]
- Assessment of the nature and age of subdural collections in nonaccidental head injury with CT and MRI. Pediatr Radiol. 2009;39:586-90.
- [CrossRef] [Google Scholar]
- Updates in chronic subdural hematoma: Epidemiology, etiology, pathogenesis, treatment and outcome. World Neurosurg. 2020;141:339-45.
- [CrossRef] [Google Scholar]
- Surgical treatments for chronic subdural hematomas: A comprehensive systematic review. World Neurosurg. 2016;86:399-418.
- [CrossRef] [Google Scholar]
- Risk factors for recurrence of chronic subdural hematoma: A single center experience. World Neurosurg. 2019;132:e506-13.
- [CrossRef] [Google Scholar]
- Chronic subdural haematoma: Modern management and emerging therapies. Nat Rev Neurol. 2014;10:570-8.
- [CrossRef] [Google Scholar]
- Radiological prognostic factors of chronic subdural hematoma recurrence: A systematic review and meta-analysis. Neuroradiology. 2021;63:27-40.
- [CrossRef] [Google Scholar]
- Chronic subdural hematoma-incidence, complications, and financial impact. Acta Neurochir (Wien). 2020;162:2033-43.
- [CrossRef] [Google Scholar]
- Working toward rational and evidence-based treatment of chronic subdural hematoma. Clin Neurosurg. 2010;57:112-22.
- [Google Scholar]
- Chronic subdural hematoma: Epidemiology and natural history. Neurosurg Clin N Am. 2017;28:205-10.
- [CrossRef] [Google Scholar]
- Prognostic factors in chronic subdural hematoma: Results from a monocentric consecutive surgical series of 605 patients. J Neurosurg Sci. 2021;65:14-23.
- [CrossRef] [Google Scholar]
- Evidence based diagnosis and management of chronic subdural hematoma: A review of the literature. J Clin Neurosci. 2018;50:7-15.
- [CrossRef] [Google Scholar]
- Chronic subdural hematoma: A historical and clinical perspective. World Neurosurg. 2017;108:948-53.
- [CrossRef] [Google Scholar]
- The management and outcome for patients with chronic subdural hematoma: A prospective, multicenter, observational cohort study in the United Kingdom. J Neurosurg. 2017;127:732-9.
- [CrossRef] [Google Scholar]
- What determines the laterality of the chronic subdural hematoma? J Korean Neurosurg Soc. 2010;47:424-7.
- [CrossRef] [Google Scholar]
- Intraoperative hematoma volume can predict chronic subdural hematoma recurrence. Surg Neurol Int. 2021;12:232.
- [CrossRef] [Google Scholar]
- Time to surgery following chronic subdural hematoma: Post hoc analysis of a prospective cohort study. BMJ Surg Interv Health Technol. 2019;1:e000012.
- [CrossRef] [Google Scholar]
- The use of the Karnofsky index in the assessment of clinical state in patients with chronic subdural hematoma: The first observation from Vojvodina. Med Glas (Zenica). 2014;11:132-7.
- [Google Scholar]
- Burr-hole evacuation of chronic subdural hematoma: Biophysically and evidence-based technique improvement. J Neurosci Rural Pract. 2019;10:113-8.
- [CrossRef] [Google Scholar]
- Single versus double Burr hole for drainage of chronic subdural hematoma: Randomized controlled study. World Neurosurg. 2021;146:e565-7.
- [CrossRef] [Google Scholar]







