Translate this page into:
Cervical disc herniation manifesting as a Brown-Sequard syndrome
Address for correspondence: Dr. Kunio Yokoyama, Department of Neurosurgery, Takeda general hospital, Kyoto, Japan, 28-1 Ishidamoriminamimachi, Fushimi, Kyoto City, Kyoto, 572-6331, Japan. E-mail: neu100@poh.osaka-med.ac.jp
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Brown-Sequard syndrome is commonly seen in the setting of spinal trauma or an extramedullary spinal neoplasm. The clinical picture reflects hemisection of the spinal cord. We report a rare case of Brown-Sequard syndrome caused by a large cervical herniated disc. A 63-year-old man presented with progressive right hemiparesis and disruption of pain and temperature sensation on the left side of the body. Magnetic resonance imaging showed large C3-C4 disc herniation compressing the spinal cord at that level, with severe canal stenosis from C4 through C7. Decompressive cervical laminoplasty was performed. After surgery, complete sensory function was restored and a marked improvement in motor power was obtained.
Keywords
Brown-Sequard syndrome
cervical disc herniation
decompressive cervical lamminoplasty
Introduction
Brown-Sequard syndrome involves ipsilateral loss of motor function resulting from corticospinal tract interruption, combined with contralateral loss of pain and temperature sensation as a result of spinothalamic tract dysfunction.[1] The most common causes of this syndrome are traumatic injuries and spinal cord neoplasms.[2–4]
In addition, other etiologies have been described including ischemia,[5] epidural hematoma,[4] multiple sclerosis,[6] and degenerative diseases such as disc herniation and cervical spondylosis.[78] However, a herniated cervical disc is a rare cause of Brown-Sequard syndrome. We report a rare case of a C3-C4-herniated cervical disc resulting in Brown-Sequard syndrome.
Case Report
A 63-year-old man presented with a 4-day history of right neck pain and progressive right hemiparesis. He was referred from the orthopedics department on the suspicion of cerebrovascular disease. There was no history of trauma, arthritis, or collagen disease, while neurological evaluation revealed motor weakness and spasticity of the right side of the body (Manual Muscle Test 4/5) and decreased pain and temperature sensation on the left side below the C5 dermatome. On deep tendon reflex examination, ipsilateral hyperreflexias were identified on the right side. However, there were no radicular symptoms and no bladder dysfunction. These findings were consistent with Brown-Sequard syndrome localized to the upper cervical region. Magnetic resonance imaging of the cervical spine revealed a large extradural paramedian C3-C4 disc herniation severely compressing the spinal cord on the right side, with myelomalacia of the cervical cord at that level on T2-weighted images [Figures 1a and b]. In addition, severe canal stenosis from C4 through C7 with myelomalacia accompanied the C3-C4 disc herniation. The patient underwent decompressive posterior cervical laminoplasty (C3-C6) and partial laminectomy of C7. On postoperative day 1, he showed significant improvement in his left-sided sensation and a marked recovery of right-sided motor function. After postoperative treatment with a soft collar and rehabilitation for 13 days, the patient was discharged. Postoperative magnetic resonance imaging revealed a significant decrease of the spinal cord hyperintensity on T2-weighted images [Figure 1c]. One month after surgery, a follow-up examination revealed normal motor power on the right side and full recovery of the left-sided pain and temperature sensation.
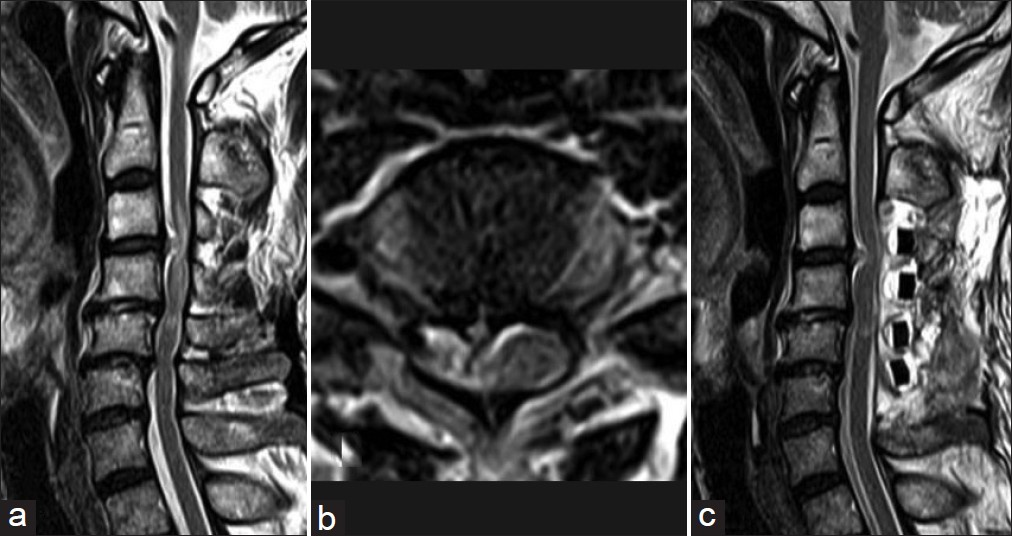
- Pre and postoperative magnetic resonance images of the cervical spine. (a) Preoperative sagittal T2-weighted image showing a C3-C4 herniated disc, cervical cord signal change with edema, and C4 through C7cervical canal stenosis. (b) Preoperative axial T2- weighted image consistent with signal changes in the right hemicord. (c) Post-operative magnetic resonance image of the cervical spine. The sagittal T2-weighted image shows the improvement of signal changes in the hemicord
Discussion
In 1928, Stookey first identified a herniated cervical disc as a possible cause of Brown-Sequard syndrome.[9] However, it is a rare cause, and to the best of our knowledge, only 39 cases of Brown-Sequard syndrome caused by cervical disc herniation have been reported in the international literature till date.[7810] Our literature review revealed that the age of onset ranged from 25 to 73 years, with a mean symptom duration of 2.4 months. As an initial symptom, neck pain was most frequent (26 cases, 67%), followed by numbness of the contralateral arm or leg (21 cases, 54%). However, only a few cases presented with classical radicular symptoms (9 cases, 23%). This indicated that the neural compression seen in these patients was primarily on the spinal cord itself and not the nerve root. There were 10 cases (26%) of intradural herniation and 29 cases (74%) of extradural herniation. The levels involved were C2-C3 in 2 cases, C3-C4 in 8 cases, C4-C5 in 6 cases, C5-C6 in 18 cases, and C6-C7 in 5 cases. In 46% of the cases, the level involved was C5-C6, and incidences of disc herniation at C3-C4 were comparatively rare. All patients were surgically treated with laminectomy or hemilaminectomy (7 cases), anterior discectomy without interbody fusion (5 cases), or anterior discectomy or corpectomy followed by interbody fusion (27 cases). In most cases, comparative recovery of the symptoms was obtained although minor residual deficits remained in some cases. There was no apparent difference in the clinical outcome between operative methods although most patients (82%) underwent an anterior discectomy with interbody fusion. Intradural herniation seemed to be associated with incomplete neurological recovery more often than extradural herniation. This is because of direct damage to the ipsilateral spinal cord caused by the intradural disc fragment. The technical decision of whether to use the anterior or the posterior approach is influenced by many factors including the exact location of disc herniation and the experience and preference of the surgeon. In the present case, because the myelomalacia associated with canal stenosis was extending to the C5 level, we chose decompressive laminoplasty. The anterior approach may allow easier exposure and direct decompression of the herniated disc. However, serious disadvantages of the anterior approach, such as adjacent segmental degeneration after anterior interbody fusion, have recently been recognized. Therefore, we did not choose an anterior approach. Fortunately, the postoperative neurological outcome of the present case was excellent. We believe that an improvement in the symptoms will be obtained if a posterior shift of the spinal cord is provided even slightly. However, we would have had to consider adding an anterior discectomy in the present case, if the residual motor deficit had remained.
Recent advances in medical technology, particularly diagnosis by magnetic resonance imaging, will increase the chance that clinicians will be able to identify this disease. However, the acute manifestation of hemiparesis associated with Brown-Sequard syndrome may mislead physicians into a delayed diagnosis, or incorrect diagnosis of a cerebral stroke. Therefore, careful history taking and detailed neurologic examination are indispensable as the symptoms caused by cervical herniation sometimes become worse rapidly. In addition we recommend early surgical intervention for these patients.
Source of Support: Nil
Conflict of Interest: None declared.
References
- De la transmission des impressions sensitives par la moelle epiniere. CR Soc Biol. 1849;1:192-4.
- [Google Scholar]
- Intramedullary spinal cord metastasis of lung adenocarcinoma presenting as Brown-Sequard syndrome. Surg Neurol. 2004;61:72-6.
- [Google Scholar]
- Relevance of the diagnosis traumatic cervical Brown-Sequard-plus syndrome: An analysis based on the neurological and functional recovery in a prospective cohort of 148 patients. Spinal Cord. 2010;48:614-8.
- [Google Scholar]
- Brown-Sequard syndrome due to non compressive disc prolapse and spinal cord infarction. QJM. 2009;102:225-7.
- [Google Scholar]
- Multiple sclerosis manifesting as a Brown-Secord syndrome. Eur J Neurol. 2003;10:190-1.
- [Google Scholar]
- High cervical disc herniation and Brown-Sequard syndrome. J Bone Joint Surg Br. 1999;81:462-3.
- [Google Scholar]
- Brown-Sequard syndrome produced by C3-C4 cervical disc herniation: A case report and review of the literature. Spine. 2008;20(33):E279-82.
- [Google Scholar]
- Compression of the spinal cord due to ventral extradural cervical chondromas: Diagnosis and surgical treatment. Arch Neurol Psychiatry. 1928;20:275-91.
- [Google Scholar]
- Cervical disc herniation as a cause of brown-séquard syndrome. J Korean Neurosurg Soc. 2009;46:505-10.
- [Google Scholar]






