Translate this page into:
Catatonia in Patients with Dementia Admitted to a Geriatric Psychiatry Ward
Address for correspondence: Dr. Walter Jaimes-Albornoz, Psychiatry Service, Donostia University Hospital, Basque Health Service-Osakidetza, Paseo del Dr. Begiristain s/n, CP: 20014, Donostia-San Sebastian, Basque Country, Spain. E-mail: walter.jaimesalbornoz@osakidetza.eus
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
To determine the frequency and characteristics of catatonia in persons with dementia, all patients admitted to an old age psychiatry ward were screened for catatonia with the Bush-Francis Catatonia Screening Instrument (BFCSI) over a period of 6 months. Thirty-seven patients were admitted, and there were 14 patients with dementia. The rate of catatonia in these patients was 42.8% (6 out of 14). Five out of six of these patients received treatment for catatonia with lorazepam, all achieving complete remission. Catatonia occurred frequently in patients admitted with dementia.
Keywords
Geriatric psychiatry
catatonia
prevalence
INTRODUCTION
Catatonia is a treatable neuropsychiatric disorder characterized by motor, behavioral, and autonomic abnormalities,[1] which remains underdiagnosed in older adults and those with dementia.[23] In this group, its frequency is unclear, etiology tends to be multifactorial,[23] and there is a greater risk of complications if undiagnosed or untreated.[2] To ascertain the frequency and clinical characteristics of catatonia in patients with dementia admitted to an acute old age psychiatry ward, we undertook a prospective survey that identified six patients with dementia and catatonia over a 6-month period, using the BFCSI.[4]
CASE SERIES
We prospectively identified patients with dementia and catatonia admitted to an acute geriatric psychiatry ward over a 6-month period to ascertain the frequency of catatonia, using the BFCSI to aid the clinical assessment.[4] The survey was approved by our institution. Patients met the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria[5] for major neurocognitive disorder. Patients in whom two or more catatonic signs were detected were assessed for severity with the Bush-Francis Catatonia Rating Scale (BFCRS).[4] Catatonia was diagnosed using the DSM-5[5] and Fink and Taylor criteria.[6] Data were collected on sociodemographics, past medical/psychiatric/drug history, clinical findings, treatment, complications/outcome, and investigations. Treatment with lorazepam orally or intramuscularly was initiated in patients who fulfilled diagnostic criteria for catatonia, based on the regime proposed by Rosebush and Mazurek.[7] Catatonic phenomena were reevaluated regularly using the BFCRS until complete resolution or until day 25. Informed consent for routine clinical treatment was not possible in these patients due to their significant cognitive impairment; treatment was provided within specific English mental health/mental capacity legislation.
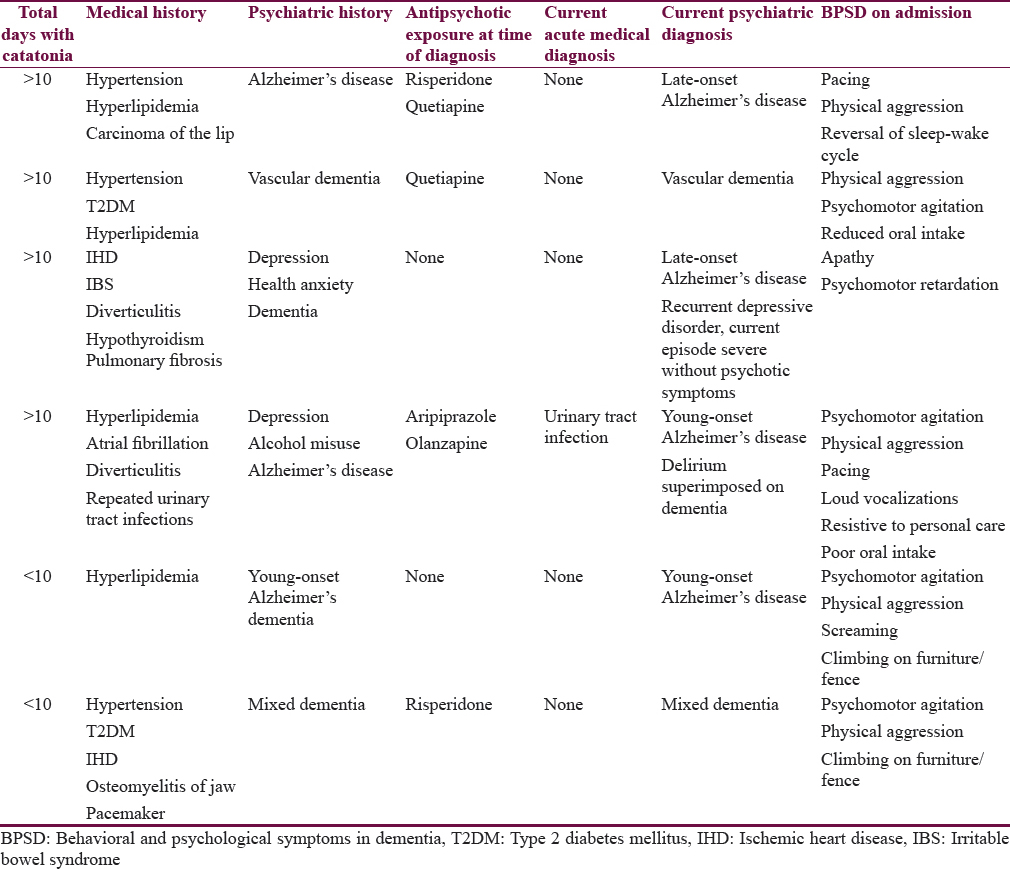
Thirty-seven patients were admitted, of which 14 had a diagnosis of dementia. Of these, six patients (2 males/4 females; mean age: 77 years; range: 68–87; Alzheimer-type (4), mixed dementia (1), and vascular dementia (1) [Table 1] presented with two or more signs of catatonia in the BFCSI.[4] All cases met the DSM-5 and Fink and Taylor diagnostic criteria for catatonia.[56] One patient suffered from comorbid severe depression without psychotic symptoms and another from delirium from a urinary tract infection. Eight patients with dementia did not have catatonia (5 female/3 male; mean age 77.4 years; range: 65–90). The rate of catatonia in patients with dementia was 42.8%. They presented with four to eight catatonic signs (mean 5.7). The mean total severity score on the BFCRS was 16.3 (range: 9–27). Half of the patients presented with the retarded-stuporous variety of catatonia. All six patients underwent a brain computed tomography scan which demonstrated cortical atrophy. One case presented with a left-sided lacunar infarct in the internal capsule and a larger left parieto-occipital lesion plus more diffuse subcortical ischemia. The only relevant biochemical parameter found was a raised creatine kinase of 1083 IU/L (25–200) in one patient, attributed to the effects of catatonia and its duration (other cardiac enzymes and electrocardiogram were normal). Its values rapidly normalized with treatment for catatonia. Four patients were on antipsychotic drugs at the time of admission. Dosages of antipsychotics were modest, and they were all discontinued immediately on admission. The severity of dementia was moderate to severe in four and moderate in two patients. Two patients scored 53/100 and 54/100 in the Addenbrooke's Cognitive Examination-III.[8] The rest were too impaired to be tested.
Five patients received treatment with lorazepam. Four patients received regular and then reducing doses of oral lorazepam (dosages up to 2 mg/day), and one patient received first oral lorazepam and later oral clonazepam (0.75–2.25 mg/day) due to additional challenging behavior not fully responsive to lorazepam and then in reducing doses. One patient was treated with sodium valproate (400 mg bd orally) due to mild and nondistressing catatonic symptoms, high risk of falls, and other challenging behaviors. None of the patients treated with lorazepam presented with any adverse events.
Five patients treated with lorazepam achieved a complete remission from catatonia within 3–22 days. The patient treated with sodium valproate achieved a partial remission. Nursing and other interventions to ensure good hydration, food intake, and mobilization were also implemented.
No complications arising from catatonia were observed except in one case as explained.
In addition to treatment for catatonia, patients received treatment for dementia and associated challenging behaviors with the following drugs, alone or in combination: donepezil, sodium valproate, citalopram, mirtazapine, memantine, and trazodone. All patients were on medications for physical health problems, ranging from antihypertensives, aspirin, and statins to oral antidiabetics, iron, and proton-pump inhibitors.
All patients were eventually discharged to community settings. There was no recurrence of catatonia in any of them.
DISCUSSION
Catatonia occurred in 42.8% of patients with dementia admitted to an acute geriatric psychiatry ward over 6 months. The systematic use of the BFCSI could explain this high frequency of catatonia. Etiology appeared to be multifactorial, including structural brain disease (degenerative and vascular) due to dementia, and subsequent accrual of cognitive impairment; the presence of one or more chronic vascular risk factors; the occurrence of delirium secondary to a urine infection and a depressive episode; and exposure to antipsychotic drugs before admission in four out of six patients. There were no major complications in any patient, and it is possible that the early diagnosis of catatonia could have contributed to this. All patients who received standard treatment for catatonia with lorazepam achieved remission, and there were no recurrences.
The descriptive clinical design, the small number of cases, and the short duration of follow-up are the limitations of this survey, and its prospective design and use of a standardized catatonia scale are their relative strengths.
The early detection and treatment of catatonia in dementia can lead to significant symptomatic improvement, and this may help prevent potentially serious complications.[23] Clinicians should be aware of catatonia as a diagnostic possibility in this patient group and look for it proactively.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Rediscovering catatonia: The biography of a treatable syndrome. Acta Psychiatr Scand Suppl. 2013;127(Suppl 441):1-47.
- [Google Scholar]
- Prevalence and clinical correlations of catatonia in older adults referred to a liaison psychiatry service in a general hospital. Gen Hosp Psychiatry. 2013;35:512-6.
- [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition). Washington, DC: American Psychiatric Press; 2013.
- Catatonia: A Clinician's Guide to Diagnosis and Treatment. New York: Cambridge University Press; 2003.
- A brief cognitive test battery to differentiate Alzheimer's disease and frontotemporal dementia. Neurology. 2000;55:1613-20.
- [Google Scholar]






