Translate this page into:
Atypical meningioma and acute subdural hemorrhage
Address for correspondence: Dr. Dhaval P. Shukla, Department of Neurosurgery, National Institute of Mental Health and Neurosciences, Bangalore, India. E-mail: neurodhaval@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 65-year-old woman presented with a sudden onset of vomiting and altered sensorium of a one-day duration. Her Glasgow coma score at admission was 7 (not opening eyes, localizing to pain, and on an endotracheal tube). There was right hemiplegia. She did not have prior neurological symptoms, including headache. There was no history of trauma. The computed tomography (CT) scan showed a well-defined, left parietal-occipital mass lesion, based on cerebral convexity, with left fronto-tempo-parietal acute subdural hematoma (SDH) causing a midline shift of 12 mm [Figure 1a]. The coagulation profile was normal. She immediately underwent fronto-temporo-parieto-occipital craniotomy, evacuation of the acute SDH, and total excision of the parietal mass lesion. The tumor was arising from the dura, with a broad attachment. There was bleeding inside the tumor that communicated with the SDH. The postoperative CT scan showed total excision of the tumor and complete evacuation of the SDH [Figure 1b]. The histopathology report revealed atypical meningioma (WHO grade II), with intratumoral hemorrhage. At the one-month follow up, the right hemiplegia had significantly improved and she was able to walk without any support.
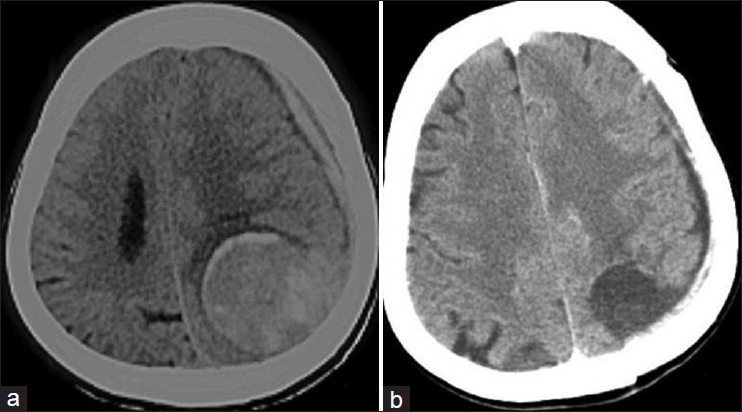
- (a) Preoperative plain CT scan axial section showing a well-defined left parieto-occipital lesion with left fronto-parietal acute subdural hemorrhage and midline shift. (b) Postoperative plain CT scan axial section showing total excision of the tumor and evacuation of the SDH
The association between meningioma and intracranial bleeding is rare. Meningiomas with bleed are found more often in patients who are older than 70 years or younger than 30 years of age.[1] The most common sites of meningioma, associated with bleeding, are intraventricular and convexity.[12] The most common bleeding locations are intracerebral/intratumoral and subarachnoid space, followed by subdural space.[13] Convexity meningiomas are more likely to produce SDH. Parasagittal and falcine meningiomas are more likely to produce intracerebral and intratumoral bleeding. Sphenoidal and intraventricular meningiomas are more likely to produce subarachnoid hemorrhage.[1] Among the histological subtypes, increased tendency for bleeding was found in malignant, followed by fibrous and angioblastic meningiomas.[1] The mortality rate associated with SDH is the lowest, and that with intracerebral hemorrhage (ICH) is the highest[1] The mechanism of bleeding related to meningioma is unclear. The following are the proposed mechanisms for SDH associated with meningiomas:[1]
-
Compensatory enlargement and weakening of blood vessels supplying or draining from the tumor
-
Bleeding from a neo-membrane on the inner surface of the dura in proximity to the tumor
-
Meningeal invasion of the vessel wall resulting in vessel disruption
-
Minor head trauma.
In our case none of the above was found. The cause of bleeding in our case could have been thinned and friable vessel walls leading to intratumoral bleeding, with massive spillage into the subdural space. In a patient presenting with acute SDH and a convexity-based tumor, the possibility of meningioma with bleed should be considered. Prompt evacuation of the SDH should be done, as it is life-saving. The meningioma should also be removed, if feasible.
References
- Spontaneous intracranial meningioma bleeding: Clinicopathological features and outcome. J Neurosurg. 2005;103:473-84.
- [Google Scholar]
- Intracranial meningiomas revealed by non-traumatic subdural haematomas: A series of four cases. Acta Neurochir (Wien). 2001;143:977-82.
- [Google Scholar]
- Intracranial meningiomas associated with non-traumatic chronic subdural hematoma. Acta Neurochir (Wien). 2006;148:1097-102.
- [Google Scholar]





