Translate this page into:
Association between patient characteristics and dissatisfaction after cranial neurosurgery: A prospective observational study
*Corresponding author: Sudhir Venkataramaiah, Department of Neuroanesthesia and Neurocritical Care, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India. vsudhir77@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wadhwa A, Akash VS, Bharadwaj S, Kadarapura NG, Konar SK, Naik S, et al. Association between patient characteristics and dissatisfaction after cranial neurosurgery: A prospective observational study. J Neurosci Rural Pract 2023;14:280-5.
Abstract
Objectives:
Patient satisfaction is an indicator of the quality of healthcare. It can improve treatment adherence and health outcomes. This study aimed to determine the incidence, predictive factors, and impact of post-operative patient dissatisfaction with perioperative care after cranial neurosurgery.
Materials and Methods:
This was a prospective observational study conducted in a tertiary care academic university hospital. Adult patients undergoing cranial neurosurgery were assessed for satisfaction 24 h after surgery using a five-point scale. The data regarding patient characteristics that may predict dissatisfaction after surgery were collected along with ambulation time and hospital stay. Shapiro–Wilk test was used to assess normality of data. Univariate analysis was performed using Mann–Whitney U-test and significant factors were entered into binary logistic regression model for identifying predictors. The level of significance was set at P < 0.05.
Results:
Four hundred and ninety-six adult patients undergoing cranial neurosurgery were recruited into the study from September 2021 to June 2022. Data of 390 were analyzed. The incidence of patient dissatisfaction was 20.5%. On univariate analysis, literacy, economic status, pre-operative pain, and anxiety were associated with post-operative patient dissatisfaction. On logistic regression analysis, illiteracy, higher economic status, and no pre-operative anxiety were predictors of dissatisfaction. The patient dissatisfaction did not impact ambulation time or duration of hospital stay after the surgery.
Conclusion:
One in five patients reported dissatisfaction after cranial neurosurgery. Illiteracy, higher economic status, and no pre-operative anxiety were predictors of patient dissatisfaction. Dissatisfaction was not associated with delayed ambulation or hospital discharge.
Keywords
Patient satisfaction
Cranial neurosurgery
Incidence
Predictive factors
Outcome
INTRODUCTION
Patient satisfaction is an individual’s assessment and emotional response to health-care experience and is an indicator of the quality of healthcare.[1,2] It largely depends on the alignment of the patient’s perceived expectations and actual health outcomes.[1] The patient satisfaction is not only a desired result of healthcare but also a means to improve treatment outcomes.[3] Dissatisfied patients often tend to have a poor health-related quality of life.[4] The patient dissatisfaction may be due to clinical or non-clinical factors or both.[5] The patient dissatisfaction varies depending on the type of surgery, time of evaluation, and the assessment methods used.
While there are many studies evaluating perioperative patient satisfaction after non-cranial surgeries, there is paucity of literature on patient satisfaction after cranial neurosurgery.[6,7] Hence, it is important to assess this patient reported outcome in this specific surgical population, especially in the developing countries where no such data is available. This knowledge will provide insights about the magnitude of dissatisfaction and potential factors contributing to it and if the patient dissatisfaction affects post-operative outcomes.
The primary objective of the present study was to determine the incidence of patient dissatisfaction with regard to perioperative care after cranial neurosurgery. The secondary objective was to identify patient characteristics that contribute to dissatisfaction after surgery. We also aimed to assess the impact of post-operative dissatisfaction on clinical outcomes of ambulation and duration of hospital stay after the surgery.
MATERIALS AND METHODS
Study design, setting, and ethics
This prospective observational cohort study was conducted among patients undergoing cranial neurosurgery at an academic tertiary care neurosciences hospital in India, from September 2021 to June 2022. The present study is a secondary analysis of our study evaluating acute postoperative pain after cranial neurosurgery. Approval was obtained from the Ethics Committee of the institute before the recruitment of patients for the study (National Institute of Mental Health and Neurosciences,/31st IEC [BS and NS DIV.]/2O21 dated August 31, 2021) and the study was registered with Clinicaltrials.gov (https://clinicaltrials.gov/ct2/show/NCT05264012) and the Clinical Trial Registry of India (CTRI/2021/09/036525 dated September 15, 2021).
Participants
This study included patients of either gender over 18 years of age undergoing elective cranial neurosurgery. Exclusion criteria for patients were being below 18 years of age, undergoing emergency or non-cranial surgery, and surgery under local anesthesia. Patients who were unable to verbalize due to altered consciousness and having a tracheal tube in situ were also excluded from the study. Informed consent was obtained from the participants before their recruitment.
Data collection
The surgery list was screened daily to identify prospective patients that might fit the inclusion criteria of the study. Data regarding clinical variables and patient demographics such as age, body mass index (BMI), gender, domicile, literacy, employment status, income, and comorbidities were obtained preoperatively. Our hospital classifies patients as below poverty line (annual income < INR 20,000), middle level (annual income between INR 20,000 and 40,000), and above poverty line (annual income > INR 40,000) for the purpose of providing free, partially free, and paid treatment. Pre-operative assessments for depression and anxiety were conducted using the hospital anxiety and depression scale and categorized as normal (0–7 score), borderline (8–10 score), and abnormal (11–21 score).[8] Pre-operative and post-operative pain were assessed using a numeric rating scale (NRS) ranging from 0 to 10. Patients with a score of four or higher were considered as having significant pain. Patients’ perception about surgery was assessed using five questions: (1) Do you believe surgery will improve your current problem?; (2) Do you believe this hospital is best suited to treat your problem?; (3) Are you spiritual/ religious?; (4) Are you scared/worried about your surgery?; and (5) Have your concerns/fear been addressed by doctors attending you?. Each question was scored as either zero (for no) or one (for yes), excluding question 4, which was reverse scored. The final cumulative score ranged from 0 to 5, with five indicating highest positive perception and zero implying lowest positive perception. Intraoperative data included American Society of Anesthesiologists grade, and type of surgery and anesthesia. On post-operative day 1, roughly about 24 h after surgery, data regarding NRS for pain, ambulation, and patient dissatisfaction were collected. The patient satisfaction was assessed on a five-point rating scale with five being very satisfied, four being somewhat satisfied, three being neutral, two being somewhat dissatisfied, and one being very dissatisfied. For the purpose of this study, we considered scores of 1 and 2 as dissatisfaction and 3–5 as no dissatisfaction. The duration of post-operative hospital stay was calculated from surgery and discharge dates.
Sample size estimation and statistical analyses
Based on a previous study that observed, a 6% dissatisfaction rate after cranial neurosurgery among the 418 patients studied,[6] and considering a confidence level of 99%, and a margin of error of 1%, a sample size of 377 was deemed essential for this study. Expecting about 10% attrition from the analysis due to inability to assess satisfaction in the postoperative period due to different reasons, we planned to recruit at least 415 patients in this study.
Statistical analyses were conducted using the Statistical Package for the Social Sciences version 28 statistical package (Chicago, IL, USA). The Shapiro–Wilk test was used to test the normality of data. The results are presented as median and interquartile range, or number and percentage. The univariate analysis was done using the Mann–Whitney U-test as data were not normally distributed. The factors significant after the univariate analysis were entered into a binary logistic regression model to identify the possible predictors of patient dissatisfaction. The level of significance was set at P < 0.05.
RESULTS
A total of 1491 patients undergoing neurosurgery were screened for eligibility for recruitment and 496 patients were included into the study. However, 106 patients were excluded from the analysis for reasons mentioned in the flow diagram [Figure 1] and data from 390 patients were analyzed.
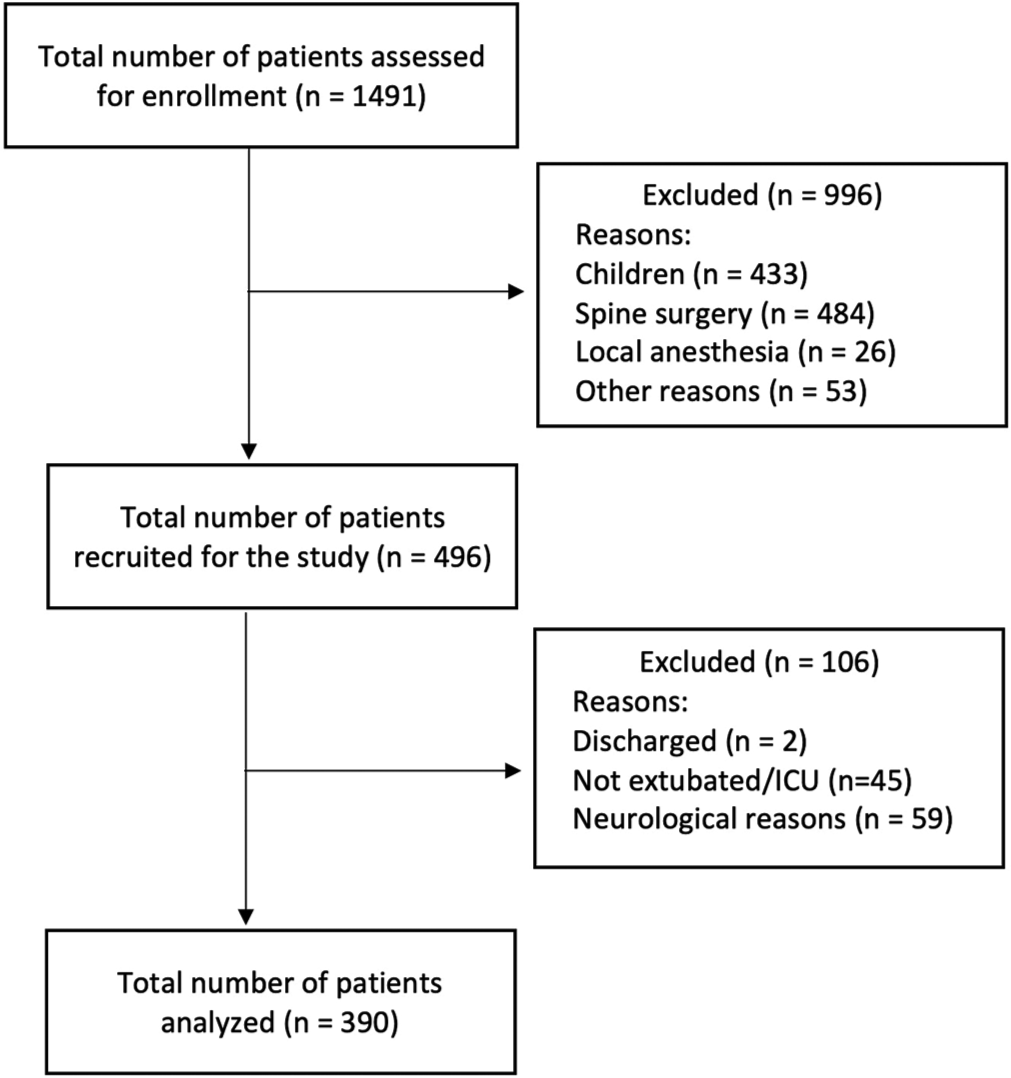
- Flow diagram showing patient flow into the study.
The overall incidence of patient dissatisfaction assessed 24 h after cranial neurosurgery was 20.5% (80/390). The results of the univariate analysis on comparing the potential risk factors for post-operative satisfaction and dissatisfaction after cranial neurosurgery are presented in [Table 1]. Among the potential risk factors assessed, literacy, economic status, pre-operative pain, and anxiety were found to be associated with post-operative patient dissatisfaction. A binary logistic regression model was used to identify independent predictors of patient dissatisfaction [Table 2]. Illiteracy, higher economic status, and absence of pre-operative anxiety were found to be predictors of post-operative dissatisfaction. The patient dissatisfaction did not impact the time for ambulation or duration of hospital stay after the surgery [Table 3].
| Variables | Dissatisfaction (n=80) | No dissatisfaction (n=310) | P-value |
|---|---|---|---|
| Age (years) | 45 (31–57) | 42 (32–50) | 0.113 |
| BMI (kg/m2) | 23.5 (20.7–26.2) | 24.1 (22.0–26.6) | 0.177 |
| Female gender | 37 (46.2%) | 157 (50.6%) | 0.531 |
| Rural domicile | 63 (81.8%) | 267 (88.4%) | 0.237 |
| Illiterate | 30 (37.5%) | 60 (19.4%) | 0.001 |
| Unemployed | 56 (70%) | 189 (60.9%) | 0.154 |
| Income | <0.001 | ||
| Below poverty line | 21 (26.2%) | 192 (61.9%) | |
| Middle level | 7 (8.7%) | 17 (5.4%) | |
| Above poverty line | 52 (65%) | 101 (32.5%) | |
| Presence of comorbidities | 15 (18.7%) | 65 (20.9%) | 0.757 |
| Surgery site-supratentorial | 65 (81.2%) | 239 (77%) | 0.454 |
| Awake craniotomy | 9 (11.3%) | 16 (5.2%) | 0.067 |
| ASA Grade | 2 (2–2) | 2 (2–2) | 0.118 |
| Pre-operative NRS score for pain | 0 (0–0) | 0 (0–4) | 0.001 |
| Pre-operative anxiety score category | 1 (1–1) | 1 (1–2) | 0.001 |
| Pre-operative depression score category | 1 (1–1) | 1 (1–1) | 0.611 |
| Positive perception about surgery | 64 (80%) | 247 (79.7%) | 1.000 |
| Significant pain on 1st post-operative day | 32 (42.7%) | 147 (50.3%) | 0.247 |
BMI: Body mass index, ASA: American Society of anesthesiologists, NRS: Numerical rating scale, MAC: Minimum alveolar concentration
| Variables | B | S.E. | Wald | df | Sig. | Exp (B) | 95% CI for EXP (B) | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Anxiety score category | 0.595 | 0.140 | 18.084 | 1 | 0.000 | 1.813 | 1.378 | 2.385 |
| Pre-operative pain score | 0.078 | 0.059 | 1.733 | 1 | 0.188 | 1.081 | 0.963 | 1.215 |
| Education status | -0.827 | 0.306 | 7.308 | 1 | 0.007 | 0.437 | 0.240 | 0.797 |
| Income_1BPL_2ML_3APL | 27.473 | 2 | 0.000 | |||||
| Income_1BPL_2ML_3APL (1) | 1.596 | 0.306 | 27.280 | 1 | 0.000 | 4.935 | 2.711 | 8.982 |
| Income_1BPL_2ML_3APL (2) | 0.363 | 0.512 | 0.502 | 1 | 0.479 | 1.437 | 0.527 | 3.919 |
BPL: Below poverty line, ML: Middle level, APL: Above poverty line
| Variables | Dissatisfied (n=80) | Not dissatisfied (n=310) | P-value |
|---|---|---|---|
| Duration of post-operative hospital stay (days) | 7 (3−12) | 5 (4−9) | 0.475 |
| Ambulation on 1st post-operative day | 35 (46.7%) | 156 (52.5%) | 0.597 |
Values expressed as median (interquartile range) or number (percentage).
DISCUSSION
Studies on patient satisfaction after cranial neurosurgery are scarce. A previous study which evaluated patient satisfaction 30 days after cranial neurosurgery observed a patient dissatisfaction rate of 6% among the 418 patients studied.[6] The patient satisfaction was dependent on functional status, infections, overall health status, and severity of symptoms.[6] We observed a higher (20%) dissatisfaction rate when assessment was done during the early post-operative period. It is likely that dissatisfaction decreases over time as patients may not recollect their exact experience about the perioperative period after a significant delay or their views about certain aspects of perioperative care that led to the reporting of early dissatisfaction might not seem important at a later time point. In patients undergoing microvascular decompression (MVD) and partial sensory rhizotomy (PSR) for trigeminal neuralgia, dissatisfaction was noted in 4% and 20% of patients after MVD and PSR, respectively.[7] Our findings in overall cranial surgery population are similar to that observed after PSR but different after MVD. This suggests that within the cranial neurosurgery cohort itself, the patient dissatisfaction varies depending on the type of surgery the patient undergoes. The predictors of patient satisfaction in patients undergoing spine surgeries were patient and healthcare worker relationship, age, health status, length of hospital stay, pain, complications, readmission, and psychological factors such as depression and distress.[5] Among the patients surveyed in neurosurgery outpatient clinics, older age, cranial diagnosis, surgeon’s recommendation for surgery, and access to government health insurance were associated with better patient satisfaction.[9] A shorter symptom duration and immediate pain improvement after surgery were associated with better patient satisfaction after cervical spine surgery.[10] Among the several patient characteristics that we explored as risk factors, we observed only illiteracy, higher economic status, and absence of pre-operative anxiety to be predictors of patient dissatisfaction after cranial neurosurgery.
Literate patients tend to be more satisfied with health-care services.[11] Conversely, patients with lower levels of education tend to be more dissatisfied with pre-operative care.[12] This was noted in our study too where illiteracy predicted patient dissatisfaction after cranial neurosurgery. It is important for health-care facilities to arrange for easy-to-comprehend materials and information to accommodate for illiterate patients when educating them about surgery, anesthesia, and perioperative course.
We observed that patients who paid from their pockets for the surgery and hospital services were more dissatisfied than patients below the poverty line. Poor patients whose health-care expenses are taken care by public funding are more receptive to the quality of perioperative care available for free to them. In contrast, patients who pay out of their pockets have higher expectations which often do not match the actual deliverables in a government hospital and, hence, tend to be more dissatisfied. Similar observations were reported in a non-surgical population from Iran, where patients from higher economic status reported more dissatisfaction.[13] However, the opposite is also seen where patients with low-income reporting more dissatisfaction and vice versa.[14] This is mainly due to poor access and quality of healthcare that they receive and may not be applicable to hospitalized patients undergoing surgery.
Higher pre-operative anxiety has been associated with more dissatisfaction in the previous studies.[15] In contrast, dissatisfaction was not noted in patients with pre-operative anxiety in the present study. Three main categories of pre-operative anxiety exist: Concern about the unknown, fear of getting ill, and concern for one’s life.[16] However, if the anxiety provoking stimulus is not followed with the feared consequence, the anxiety related to the stimulus reduces.[17] Moreover, pre-operative anxiety is significantly higher than the post-operative anxiety.[18] Therefore, after the surgery, in the absence of the feared consequence and uncertainty, perhaps our patients were less anxious than anticipated and consequently, more satisfied.
No other factor that we assessed in our study was associated with dissatisfaction after cranial neurosurgery. A previous study in patients undergoing total knee arthroplasty noted that post-operative pain but not pre-operative pain was associated with dissatisfaction after surgery.[19] We did not find either pre-operative or post-operative pain to be predictive of patient dissatisfaction. In an earlier study, despite 76% of the 191 patients reporting moderate-to-severe pain after surgery, satisfaction rate was high at 81%.[20] Similar findings were seen in another study where despite 86% patients experiencing post-operative pain, 90% reported satisfaction with the care they received.[21] Thus, the relationship between pain and satisfaction appears be complex. The patient satisfaction is likely to be higher if response of the health-care providers to their pain is humane, timely, and appropriate, even if they perceive higher pre- and post-operative pain.
Pre-operative depression was not associated with postoperative depression in our study. The relationship between depression and satisfaction is inconsistent with some studies observing dissatisfaction among the patients with pre-operative depression,[22] while others finding no association between the two,[11] similar to our findings.
Several factors that were not associated with patient dissatisfaction in our study were also not predictive of dissatisfaction in earlier studies. Older age and comorbidities were not associated with patient dissatisfaction in the present study, similar to previous studies.[6] Gender and occupation were not associated with patient satisfaction in our study as well as some previous studies.[23] We did not observe craniotomy site to be predictive of patient satisfaction which was similar to the results of a previous study.[6] The patients’ perception about surgery was not associated with their post-operative satisfaction in our study. Although this was not exactly explored in earlier studies, not meeting pre-operative expectations of surgical outcomes did not result in dissatisfaction after spine surgeries.[24] The previous studies have found no relationship between patient dissatisfaction and length of hospital stay,[12] corroborating our results.
Strengths and limitations
This is probably the first study from a developing world to assess dissatisfaction, an important patient reported outcome, after cranial neurosurgery. We explored the relationship between various patient characteristics and dissatisfaction, and also the impact of dissatisfaction on ambulation time and duration of hospital stay after surgery. However, there are certain important limitations. First, the patient satisfaction was assessed at only one time point. Perhaps the findings would be different if satisfaction was to be assessed at later time points. Second, we explored only the relationship between patient characteristics and dissatisfaction about perioperative care. The patient satisfaction can be impacted by other domains such as hospital environment (lighting, ventilation, noise, cleanliness, etc.), availability of family support, cost of surgery and hospitalization, waiting time for surgery and cancellations, prognosis of neurosurgical illness, and humanistic factors such as healthcare workers’ attitudes toward patients and their perioperative issues. These factors were not assessed in this study. Finally, as patient characteristics can vary between developing and developed world and between various types of surgeries, our findings regarding dissatisfaction after cranial neurosurgery from an Indian hospital may not be generalizable to populations which are dissimilar to that of our study.
CONCLUSION
Every one in five patients in our study reported dissatisfaction after cranial neurosurgery. Illiteracy, higher economic status, and absence of pre-operative anxiety were predictive of patient dissatisfaction. However, dissatisfaction was not associated with longer time to ambulation or hospital discharge. Improving literacy (including health literacy) as a broad public health measure and providing value for money for paying patients as a specific intervention may help reduce dissatisfaction among patients undergoing cranial neurosurgery in a health-care setup similar to ours.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
The study is part of a cognitive science research initiative of the department of science and technology funded research project.
References
- Patient satisfaction: Implications and predictors of success. J Bone Jt Surg Am. 2013;95:e69.
- [CrossRef] [PubMed] [Google Scholar]
- The quality of care. How can it be assessed? JAMA. 1988;260:1743-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of patient satisfaction on outcomes of care. Expert Rev Pharmacoecon Outcomes Res. 2009;9:393-5.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with patient satisfaction with care among dermatological outpatients. Br J Dermatol. 2001;145:617-23.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of patient satisfaction in spine surgery: A systematic review. World Neurosurg. 2021;146:e1160-70.
- [CrossRef] [PubMed] [Google Scholar]
- Patient satisfaction and short-term outcome in elective cranial neurosurgery. Neurosurgery. 2015;77:769-75.
- [CrossRef] [PubMed] [Google Scholar]
- Patient reports of satisfaction after microvascular decompression and partial sensory rhizotomy for trigeminal neuralgia. Neurosurgery. 2005;56:1304-11.
- [CrossRef] [PubMed] [Google Scholar]
- The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-70.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with greater patient satisfaction in outpatient neurosurgical clinics: Recommendation for surgery, older age, cranial chief complaint, and public health insurance. Clin Neurol Neurosurg. 2022;222:107436.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of patient satisfaction following anterior cervical discectomy and fusion for cervical radiculopathy. Clin Neurol Neurosurg. 2021;205:106648.
- [CrossRef] [PubMed] [Google Scholar]
- Early patient satisfaction following orthopaedic surgery. J Clin Orthop Trauma. 2020;11:S823-8.
- [CrossRef] [PubMed] [Google Scholar]
- Patient satisfaction with preoperative care and its relationship with patient characteristics. Med J Cairo Univ. 2013;81:1-10.
- [Google Scholar]
- Socioeconomic status and satisfaction with public healthcare system in Iran. Int J Community Based Nurs Midwifery. 2017;5:22-9.
- [Google Scholar]
- Evaluation of patient satisfaction in relation to patient factors in surgical centre-a study from central India. IOSR J Dent Med Sci. 2015;14:104-9.
- [Google Scholar]
- Relationship between preoperative anxiety and postoperative satisfaction in dental implant surgery with intravenous conscious sedation. Med Oral Patol Oral Cir Bucal. 2010;15:e379-82.
- [CrossRef] [PubMed] [Google Scholar]
- The visual analog scale allows effective measurement of preoperative anxiety and detection of patients' anesthetic concerns. Anesth Analg. 2000;90:706-12.
- [CrossRef] [PubMed] [Google Scholar]
- Psychotherapy by reciprocal inhibition. Cond Reflex. 1968;3:234-40.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of preoperative and postoperative anxiety among elective major surgery patients in a tertiary hospital in Nigeria. Middle East J Anaesthesiol. 2015;23:235-40.
- [Google Scholar]
- Preoperative and postoperative factors affecting patient satisfaction after total knee arthroplasty. Kafkas J Med Sci. 2017;7:139-43.
- [CrossRef] [Google Scholar]
- Influence of expectations and actual pain experiences on satisfaction with postoperative pain management. Eur J Pain. 2001;5:125-33.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin. 2014;30:149-60.
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial factors and surgical outcomes: Are elderly depressed patients less satisfied with surgery? Spine (Phila Pa 1976). 2014;39:1614-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of demographic characteristics on patient's satisfaction with health care facility. Postgr Med Inst. 2014;28:154-60.
- [Google Scholar]
- An exploration of patients' expectation of and satisfaction with surgical outcome. Eur Spine J. 2013;22:2836-44.
- [CrossRef] [PubMed] [Google Scholar]







