Translate this page into:
Angiographic “omega (ω) sign” in the median artery of the corpus callosum
*Corresponding author: Prasad Krishnan, Department of Neurosurgery National Neurosciences Centre, Kolkata, West Bengal, India. prasad.krishnan@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Krishnan P, Das S. Angiographic “omega (ω) sign” in the median artery of the corpus callosum. J Neurosci Rural Pract. 2024;15:510-1. doi: 10.25259/JNRP_42_2024
A 48-year-old diabetic hypertensive lady was admitted with complaints of sudden-onset headache and vomiting. She had no neurological deficits. Computed tomography (CT) scan of the brain showed subarachnoid hemorrhage (SAH) in the suprasellar, crural, interhemispheric, and proximal Sylvian cisterns [Figures 1a and b]. The CT angiogram of the brain ruled out the presence of any aneurysm or arteriovenous malformation and showed neither A1 segments of the anterior cerebral artery were hypoplastic (though the left was larger than the right). However, three vessels were found to arise from the anterior communicating complex in the shape of the Greek letter omega “ω” in the lower case [Figures 1c and d]. The lateral two continued distally as the callosomarginal arteries and did not give any branch that ran on the corpus callosum [Figure 1e]. The central vessel continued on the course of the pericallosal arteries posterior to the other two and distally was noted to supply the medial part of both cerebral hemispheres [Figures 1f and g] and was identified as the median artery of the corpus callosum (MACC). The patient was treated conservatively and had an uneventful course in the hospital. She was subject to repeat imaging after four weeks and that too did not reveal any source of the bleed. The case was then labeled as an angionegative SAH.
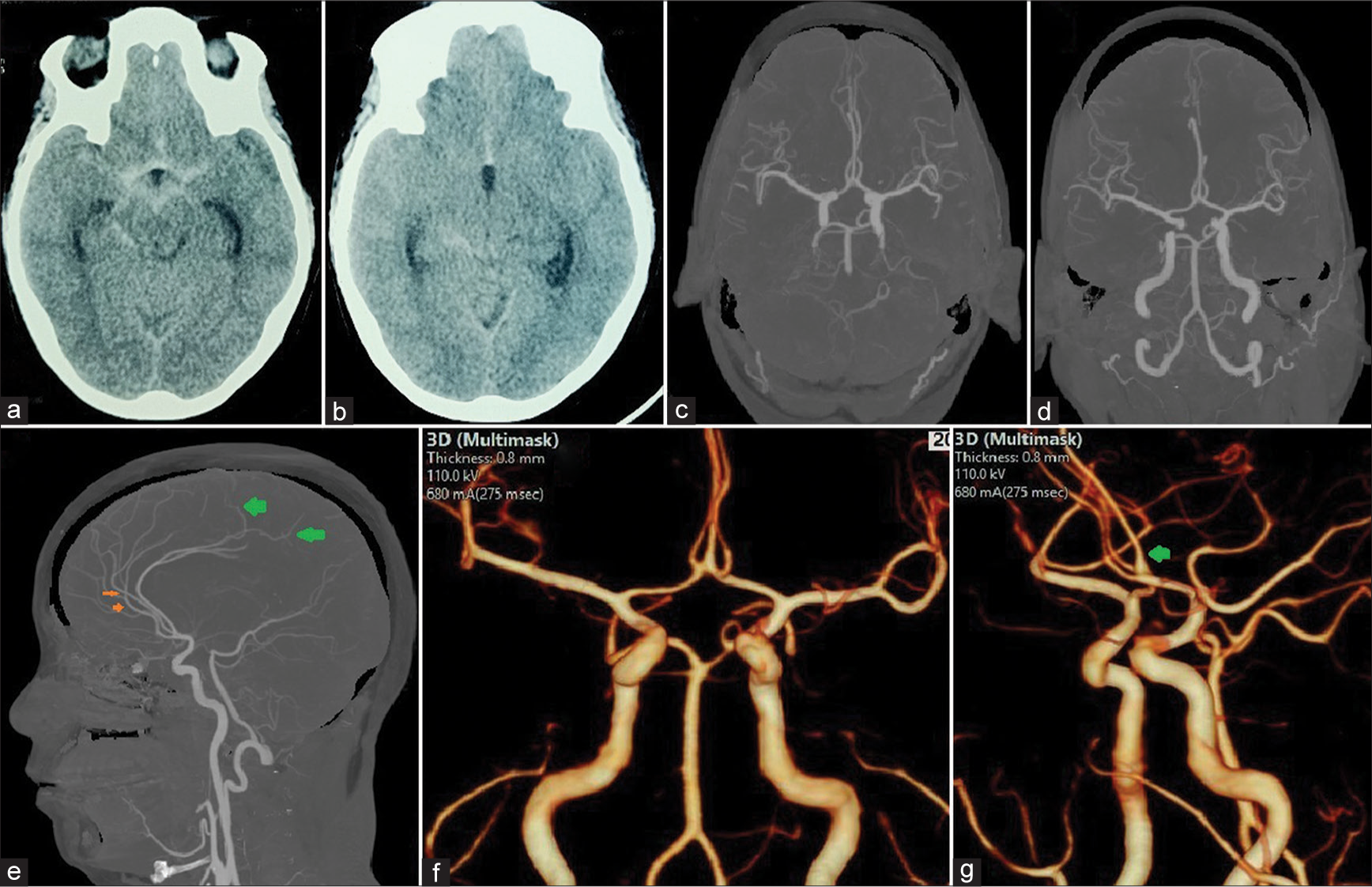
- Axial computed tomography (CT) scans (a and b) showing subarachnoid hemorrhage in the suprasellar, crural, proximal sylvian, and interhemispheric cisterns. Reconstructed CT angiographic images showing (c and d) three vessels arising from the anterior communicating artery complex and (e) showing one of these vessels following the course of the corpus callosum and supplying the posterior frontal and parietal lobes distally (green arrows). The two callosomarginal arteries are shown by orange arrows. CT scan with three-dimensional volume rendering techniques showing the cerebral vasculature (f) show the “omega (ω) sign” of the three vessels arising together and (g) the single median artery of the corpus callosum coursing posterior to the other two branches (green arrow).
Altafulla et al.[1] state that the MACC (also called the third A2 artery) is an embryonic remnant of a vessel arising from the anterior communicating artery that fails to involute and runs in the course of the pericallosal artery supplying blood to the corpus callosum, septum pellucidum rostral fornix, and frontal lobes.[1] It may exist in isolation or along with one or both of the pericallosal arteries.[2]
Krzyzewski et al.[3] report that its frequency ranges between 0.4% and 3.03%, is usually an incidental finding, and is exclusively found in females. However, Ture et al.[4] found this vessel in 30% of cadaveric specimens that they dissected and described two variants of the same – classical and hemispheric. While the former predominantly supplied the corpus callosum, the latter (which they found in only one case) supplied the medial aspect of the frontal and parietal lobes as well and this variant was found in our case.
The only other diagnosis of a single vessel on the corpus callosum is an azygos pericallosal artery.[5] However, in this case, the vessel usually arises from one of the A2 arteries (while the other A2 continues as the callosomarginal artery) but, in the case of the MACC, its origin is from the anterior communicating artery itself.[5] Such an origin can be easily appreciated by seeing the “omega (ω) sign” on the AP projection of a CT angiogram that rules out an early bifurcation of one of the A2 vessels and distinguishes an azygos pericallosal artery from a MACC.
We could not find any mention in the literature of any association of SAH specifically with this anomaly. Kovač et al.[6] analyzed CT angiographic findings of 517 patients and noted that the incidence of vascular variations did not vary significantly between patients who had and did not have aneurysms and also remarked that there were no significant differences in the incidence of aneurysms in patients who had variations in normal cerebral vasculature compared to those that did not. The “ω” sign that we noted in this case is hence an angiographic finding, which though unrelated to the SAH in this case, may be useful to identify this vessel preoperatively in an aneurysm surgery and prevent accidental clipping of the origin of this vessel and infarction of the corpus callosum.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Microanatomy of the pericallosal arterial complex. J Neurosurg. 2000;93:667-75.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical variations of the anterior communicating artery complex: Gender relationship. Surg Radiol Anat. 2015;37:81-6.
- [CrossRef] [PubMed] [Google Scholar]
- The arteries of the corpus callosum: A microsurgical anatomic study. Neurosurgery. 1996;39:1075-84.
- [CrossRef] [PubMed] [Google Scholar]
- Transcallosal and pericallosal courses of the anterior cerebral artery. Medicina (Kaunas). 2022;58:1365.
- [CrossRef] [PubMed] [Google Scholar]
- Intracranial arterial variations: A comprehensive evaluation using CT angiography. Med Sci Monit. 2014;20:420-7.
- [CrossRef] [PubMed] [Google Scholar]





