Translate this page into:
An uncommon cause for acute limb weakness: Iliopsoas hematoma
*Corresponding author: G. J. Vinayaka, Department of Neurosurgery, M. S. Ramaiah Medical College, Bengaluru, Karanataka, India. vinayakagj1789@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vinayaka GJ, Santosh SA, Naveen MA. An uncommon cause for acute limb weakness: Iliopsoas hematoma. J Neurosci Rural Pract. doi: 10.25259/JNRP_30_2025
A 66-year-old lady with diabetes and chronic kidney disease presented to us with vague symptoms of headache and vomiting. She had a history of posterior territory infarct two months prior and was on antiplatelets (Ecosprin 150 mg + Clopidogrel 75 mg). A cardiologist’s consult was sought in view of suspicion of inferior vena cava (IVC) thrombosis on 2D echo. Anticoagulation with enoxaparin 60 mg BID was started. She developed left hip pain progressing to weakness of the left hip (Grade 1/5) and knee (Grade 3/5) 2 days following the initiation of anticoagulation. Distal ankle and toe movements were intact. Her hemoglobin (Hb) was 6 mg/ dL, the international normalized ratio was 1.12, and her platelet count was 1.83 lakhs. Ultrasound abdomen revealed left psoas collection and on aspiration revealed blood. Magnetic resonance imaging [Figure 1a and b] was done showing stable hematoma and no active extravasation. Since her vitals were stable, she was managed conservatively with bed rest, cessation of anticoagulation, and antiplatelets. She was transfused with packed cells and fresh frozen plasma for anemia. Hb increased to 10 mg/dL. A computed tomography venogram was done to evaluate for the IVC thrombus which was negative. Gradually, physiotherapy was started and power improved to 3/5. On the one-week follow-up, she was ambulating with support. Antiplatelet with Ecosprin 75 mg was restarted after two weeks following a repeat ultrasound sonography, which showed a decreased size of hematoma.
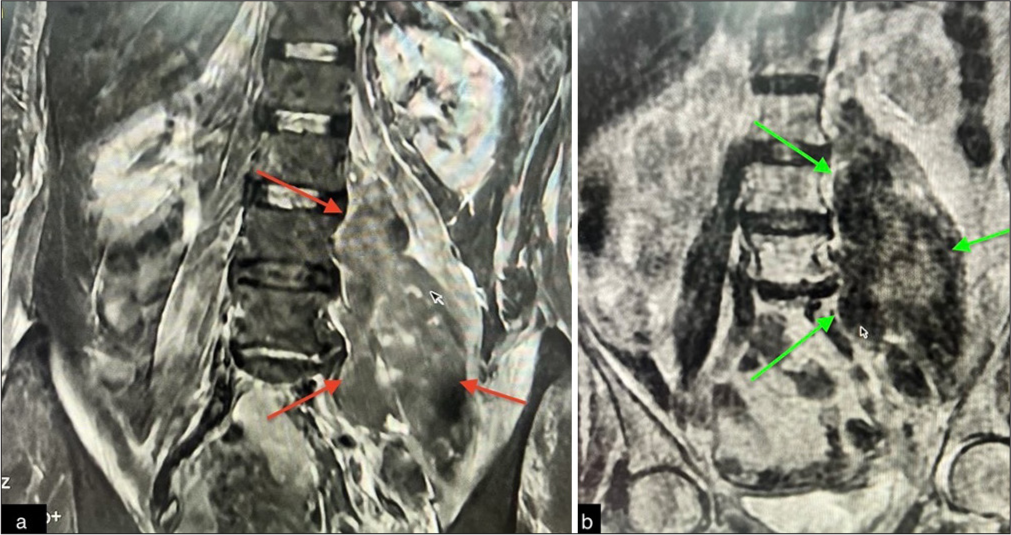
- (a) Coronal section of T2 short tau inversion recovery magnetic resonance imaging of LS spine showing hematoma in the left psoas muscle (red arrows). (b) T2-weighted image showing the hematoma (green arrows).
Iliopsoas hematoma is a rare entity. The incidence ranges from 0.6% to 6.6%.[1] It is usually reported in patients who are on anticoagulation or patients with hemophilia.[1] Weakness of the lower limb due to femoral nerve palsy is also quite uncommon.[2] and the diagnosis is challenging in the absence of trauma. Treatment of this condition is controversial, in part, due to its rarity. A conservative approach in the form of bed rest, blood transfusions, and cessation of antiplatelets/anticoagulants is justified in a hemodynamically stable patient. Serial neurological examinations and hemodynamic monitoring are required along with the high degree of suspicion in case of expanding hematoma. Surgery may be necessary in cases of large hematomas with severe neurological deficits or expanding hematoma, worsening neurological deficits.[3] More recently, another study recommended early fasciotomy of the iliopsoas muscle to minimize the chance of permanent nerve injury.[4] In another study, patients with motor deficits who underwent conservative or surgical intervention after 48 h still had permanent paresis.[5] Until large, high-quality studies are available, treatment has to be individualized.
Ethical approval
Institutional review board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Femoral neuropathy following retroperitoneal hemorrhage: Case series and review of the literature. Ann Vasc Surg. 2006;20:536-40.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral nerve palsy following iliacus hematoma. Orthopedics. 2008;31:178.
- [CrossRef] [PubMed] [Google Scholar]
- Femoral nerve palsy due to Iliopsoas hematoma. Eur J Gen Med. 2016;13:103-5.
- [CrossRef] [PubMed] [Google Scholar]
- Life-threatening spontaneous psoas haematoma treated by transcatheter arterial embolization. Eur Radiol. 1999;9:1231-4.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical impact of imaging iliopsoas hematomas during anticoagulation. Emerg Radiol. 1995;2:2-6.
- [CrossRef] [Google Scholar]





