Translate this page into:
Acute dizziness in rural practice: Proposal of a diagnostic procedure
Address for correspondence: Dr. Josef G. Heckmann, Department of Neurology, Municipal Hospital Landshut, Robert-Koch Str. 1, Landshut - 84034, Germany. E-mail: josef.heckmann@klinikum-landshut.de
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Acute dizziness is a frequent index symptom in the emergency department as well as in the rural practice office. Most acute dizziness, however, is not dangerous, but some types are highly dangerous. Clinical routine acute dizziness can be separated into frequent benign syndromes including benign paroxysmal positional vertigo (BPPV), vestibular neuritis, Meniθre's disease or vestibular migraine, and what is here referred to as the “white shark” of dizziness, i.e. a stroke in the posterior circulation or more rarely a tumor in the posterior fossa. A practical concept is presented to clarify most frequent acute dizziness syndromes using clinical and low budget methods.
Keywords
Bedside examination
clinical examination
Dix-Hallpike test
dizziness
head impulse test
neurootological techniques
nystagmus
vertigo
Introduction
Dizziness is one of the most prominent and frequent neurological symptoms. It is estimated that about 30% of all people need medical care once in their life due to this index symptom.[1] In emergency units dizziness is as frequent as 12% of all neurological presentations.[23] Otherwise financial, technical and human resources as well as specific neurological expertise are limited in particular in underprivileged areas.[45] In addition, neurophobia among students, residents and general practitioners is widespread and leads to discomfort in caring for dizzy patients.[6] Moreover, the burden of neurological disorders is increasing due to demographic changes, epidemiological transition, improved care of chronic disease and survival of hitherto lethal accidents.[5] Thus, it is imperative to diagnose straightforwardly and as precisely as possible “dizziness” syndromes using clinical and resource-saving techniques.
Therefore, in this practical concept we wish to present a procedure to examine the dizzy patient in the emergency situation respectively in the rural practice office. The main focus is to elaborate clinically with a low budget the acute vestibular syndrome, which involves the frequent benign syndromes[7] and the “white shark,” the stroke in the posterior circulation. It is far beyond the scope of this article to cover the topic of vertigo and dizziness completely. These aspects are handled in detail elsewhere in outstanding specific medical textbooks.[89]
History taking in the dizzy patient with focus on the four ts (type, time, trigger and associated troubles)
It is generally recommended to elaborate what the patient means by dizziness: Is it vertigo, dizziness, lightheadedness, presyncope or imbalance?[1011] Vertigo itself is an illusional, mostly rotational movement. In particular, by asking the patient we wish to catch the type of vertigo or dizziness and to differentiate between “spinning” and “wobbling." “Spinning vertigo” may occur in acute vestibular disorders of both peripheral and central origin.[12] “Wobbling” is a symptom and can indicate both vestibular and non-vestibular disorders. However, patients often have difficulties describing the type of dizziness, thus the information is of limited value.[13] Hence, more important is the history on time, duration and tempo.[1314] It should be evaluated whether the onset was acute or sudden and what the time course and duration is. Short duration symptoms between seconds and minutes are characteristic for vestibular paroxysmia or benign paroxysmal position vertigo (BPPV), whereas symptoms for half an hour to a day are suggestive for Meniθre΄s disease or vestibular migraine, and symptoms for days indicate vestibular neuritis while weeks and longer indicate phobic dizziness, bilateral loss of vestibular function or a lesion of central vestibular structures. The next imperative in history taking is the question on potential triggers. Changing of the head position (turning in bed, getting in or out of bed, tilting the head back or bending forward) is a strong indicator of positional vertigo. Head motion alone is often not tolerated in vestibular neuritis. And the final key question is the question on associated troubles, which indicate a central cause of the clinical picture. Such associated trouble can be memorized using the five deadly ds: Diplopia, dysarthria, dysphagia, dysaesthesia and dysmetria [Table 1].[13] A major concern about the acute dizzy patient or “white shark” is the occurrence of an acute stroke in the posterior circulation (cerebellum or brainstem).[15] Recently, the HINTS test was implemented to identify stroke in the posterior circulation, which means that normal head impulse test, presence of gaze-evoked nystagmus and positive test of skew indicate such a clinical pattern.[1617] In addition, even in the emergency room and the rural practice, a basic standardized history should be supplemented regarding previous diseases, vascular risk factors, circumstances and medication in order to, for instance, diagnose cardiogenic vertigo, intoxications and other causes of dizziness.[18]

Clinical examination
A rapid examination that screens for most neurological abnormalities should be performed and include examination of the patient's mental status, the cranial nerves, the motor system, reflexes, sensation and gait.[19] This can usually be done in a few minutes. If abnormalities are detected, the exam should be conducted more in detail. The armamentarium for the further clinical neuroophthalmological and -otological examination is shown in Figure 1 and contains a penlight, Frenzel glasses, Munich glasses,[20] bucket,[21] optokinetic drum and poster instruction for the performance of the Dix–Hallpike[22] and head impulse test [Figure 1].[15]
![The basic armamentarium for the clinical neuroophthalmological and -otological examination containing a penlight, Frenzel glasses, Munich glasses,[20] a prepared bucket,[21] an optokinetic drum and poster instructions for the performance of the Dix-Hallpike maneuver and head impulse test[1522]](/content/150/2015/6/2/img/JNRP-6-272-g002.png)
Examination of eye movements
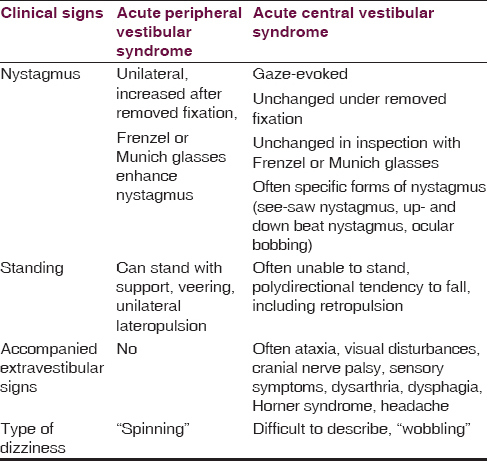
The clinical neuroopthalmological examination is of great value as it allows differentiating between a peripheral and a central oculomotor disorder and thus can give essential clues as to whether the patient suffers a stroke.[17] After inspection, as a rule smooth gaze pursuit and saccades, fixation and vergence should be examined followed by examination of the vestibulo-ocular and optokinetic reflexes.[23] By inspection in particular the tilt of the head is kept in mind as it indicates a dysfunction of the subjective visual vertical as a peripheral or central vestibular dysfunction. Normally it is examined proactively for a Horner syndrome as well as for a ptosis and pupil anisocoria.[24] In patients with nystagmus, the direction, the type and trigger should be noted. A spontaneous nystagmus of peripheral vestibular origin is always unidirectional, predominantly horizontal with a rotational component and increases when fixation is removed (Frenzel or Munich glasses, penlight-cover test).[25] Gaze-evoked nystagmus, in contrast with change of the direction, down- and upbeat nystagmus, pure torsional nystagmus and other special forms (seesaw nystagmus, rebound nystagmus and more rare forms) are always of central origin and indicate a brainstem or cerebellum disease.
Dix–Hallpike maneuver
Considering the index symptom dizziness due to positional vertigo the Dix–Hallpike maneuver should be performed. The patient is directed from the sitting position to the supine with the head rotated 45° and positioned 10° below the end of the examination table, and it is observed whether vertigo and nystagmus can be provoked. An upbeating and transient vertical nystagmus with a rotational component to the down lying ear is mostly suggestive of canalolithisis of the posterior semicircular canal and allows the diagnosis of benign paroxysmal positional vertigo (BPPV).[22] Based on this observation repositional maneuvers (Epley, modified Epley, Semont, Brandt-Daroff) can be undertaken, which are described more in detail elsewhere.[2226] In BPPV canalolithiasis rarely affects the horizontal or anterior semicircular canal, which can be treated with some different maneuvers (Barbeque, Guffoni and others).[26] For identification of BPPV of the horizontal semicircular canal the supine roll test is recommended.[27]
The head impulse test
This test, introduced by Halmagyi and Curthoys (1988), is mostly positive in the case of an acute peripheral vestibulopathy and rather rarely normal in these patients when performed clinically.[28] The head is thrusted about 10° to 15° whereby the patient is asked to fixate the examiner΄s nose. If the vestibulo-ocular reflex is intact, the patient is able to fixate the target. In the case of a hypofunction of the labyrinth the patient cannot fixate the target and needs a voluntary rapid eye movement—a saccade—back to the target when the head is quickly rotated toward the side of the affected ear. This recatching saccade is visible by the examiner and indicates a disturbed vestibulo-ocular reflex.[28]
Test to suppress visual fixation with Frenzel or Munich glasses, penlight cover test, head shaking
These tests are used to detect nystagmus, which can be suppressed by visual fixation. Recently, the penlight-cover test was proposed as a bedside method to unmask nystagmus. A penlight is shined into one eye, and the other one is intermittently occluded. Thus, the fixation is blocked and a suppressed nystagmus is more visible.[25] This test can be used if no Frenzel classes are available, which unfortunately cost about 400€ and are manufactured only by a few companies worldwide.[25] Of interest in this case are the new Munich glasses, which are remarkably cheaper and can be carried in the doctor's coat and serve the same purpose of detecting nystagmus after suppression of fixation.[20] After head shaking (about 20 times from side to side with closed eyes), the patient is examined with the Frenzel or Munich glasses for nystagmus. A horizontal-torsional nystagmus after head shaking is suggestive for a latent vestibular dysbalance, indicating a peripheral vestibular deficit. In central impairments a vertical nystagmus can be provoked.[23] In Table 2 important clinical signs are summarized that contribute to the differentiation between peripheral and central acute vestibular syndrome [Table 2].
Optokinetic reflexes (optokinetic drum)
Using this method, the physiological optokinetic reflex can be tested, which includes the rapid and slow eye movements. The patient is asked to fixate a figure of the drum, which is jolted to rotate slowly (optimal rotation velocity 60°/sec). A regular horizontal and vertical optokinetic nystagmus indicates an intact brainstem function as the responsible centers lie in the mesencephalon and pons.[23]
Subjective visual vertical (Bucket test)
By looking into the bucket the patient is asked to adjust the visible line as vertically as possible. The test is performed about 10 times in a variable sequence. Healthy subjects adjust this line ± 2.5° which can be identified by the examiner at a scale at the backside of the bucket. A more pronounced displacement indicates a pathological subjective vertical, which occurs in nearly all cases of peripheral and central vestibular disorders.[21]
Minimal ice water test
In places where a neurootological lab is not available, vestibular testing can be performed with the minimal ice water test at the bedside.[29]
Cover test, alternate cover test
In the cover test the patient is asked to fixate a target (near 30-40 cm or far 5-6 m). Then one eye is covered, and the uncovered eye is observed to see whether it is stable or shows any displacement. After uncovering, the eye is observed on any drift; if so, a tropia (misalignment of one eye to the other during binocular viewing) is to suspect. The alternate cover test allows examining for heterophoria (latent misalignment of the eyes): One eye and then the other are repeatedly covered in order to interrupt binocular viewing. The eyes are observed to see whether the position is parallel or horizontally or vertically misaligned.[30] In particular in the dizzy patient a vertical misalignment can be a sign of skew deviation, which in turn represents a central lesion.
Fixation-suppression of the vestibulo-ocular reflex
This test examines how the vestibulo-ocular reflex can be suppressed. The patient looks at the outstretched thumb and rotates the trunk. By fixating the thumb under healthy conditions the eyes remain stable and no ocular movement is visible. If eye movements occur in the opposite direction to rotation with catch-up saccades to refix gaze, then the suppression of the VOR is impaired and a brainstem or cerebellar dysfunction is probable.[23]
Romberg and gait testing
With the Romberg test the capacity to stand with closed eyes is tested.[31] A dysfunction can have many causes. Aside from vestibular (central and peripheral) disorder, neuropathy and spinal cord dysfunction can also be underlying. To use a tandem position or standing on a foam pad can make this test more sensitive to vestibular deficits.[31] Furthermore, gait testing is useful as a patient with peripheral vestibular disorder can usually remain upright using “furniture walking” while patients with cerebellar stroke are mostly unable to stand.[32]
Discussion
The main goal in the examination of the acute dizzy patient is to differentiate by clinical means between a peripheral vestibular disorder and a central disorder, in particular a stroke in the posterior circulation. In diagnosing most vertigo, dizziness, and imbalance syndromes, it is extremely useful to consider clinical key symptoms and signs including red flags [Tables 1 and 2].[713] In particular, regarding peripheral vestibular syndromes, a “rule in” approach is favored, that is to look proactively for the characteristic clinical key findings such as unidirectional spontaneous nystagmus combined with positive head impulse test in vestibular neuritis or distinctly positive findings in the Dix–Hallpike test in BPPV.[33] Taking the history carefully will allow medical professionals to identify Menière's disease and vestibular migraine.[34] The spectrum of red flags (headache, associated troubles, and signs other than vestibulocochlear nerve dysfunction) should be checked on the presence, and if positive, additional tests such as imaging procedures, lumbar puncture or specific tests in the neurootological lab should be ordered. It is, however, enormously important to realize that stroke can cause isolated dizziness and accompanying hearing loss can be a symptom of ischemia in the area of the anterior inferior cerebellar artery.[153536] Therefore, the above-mentioned three-step test (HINTS) consisting of HIT, nystagmus and test of skew introduced by Kattah et al. (2009) is very promising.[16] A normal impulse test, a fast alternating nystagmus (a spontaneous nystagmus that changes direction with gaze) and a vertical refixation on cover test (acronymized to INFARCT = Impulse normal, fast-phase alternating, refixation on cover test) revealed a sensitivity to detect stroke in 98% and a specificity of 85%.[17] Concerns about these results were expressed that they were generated with neurootological experts as clinical examiners and it would be not known how far the results can be transferred to non-specialists or even novices.[37] However, in a recent study by Chen et al. (2011) it could be shown that the bedside testing of patients is also accurate when performed by physicians inexperienced in neurootology.[38] Lately a type of ocular ECG has been suggested that may improve the accuracy of the HIT and thus facilitate the clinical diagnostic process.[39] Taken together a careful clinical examination will substantially contribute to a correct differentiation between a peripheral and a central vestibular disorder.[3840] Thus, expensive or sparsely available imaging procedures should be used only in selected patients. Otherwise a critical point of view should always be kept in mind in order to recognize non-benign positional vertigo and “tricky” vertigo in brainstem and cerebellar stroke.[4142434445] Currently vestibular disorders are intensively investigated and a number of new insights can be gained from the current research.[46] In addition, new clinical syndromes such as CANVAS have been proposed.[47] From the therapeutic side new strategies under evidence-based aspects are developed such as reposition maneuvers, vestibular rehabilitation programs and medical treatment.[48] Moreover, new techniques such as fundusphotography will be available and will become cheaper due to technical progress.[49]
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Central vertigo and dizziness: Epidemiology, differential diagnosis, and common causes. Neurologist. 2008;14:355-64.
- [Google Scholar]
- Dizziness in the emergency room: Diagnoses and misdiagnoses. Eur Neurol. 2011;66:256-63.
- [Google Scholar]
- Diagnosis of acute vertigo in the emergency department. Emerg Med J. 2011;28:538-9.
- [Google Scholar]
- Neurophobia among medical students and non-specialist doctors in Sri Lanka. BMC Med Educ. 2013;13:164.
- [Google Scholar]
- Five keys for diagnosing most vertigo, dizziness, and imbalance syndromes: An expert opinion. J Neurol. 2014;261:229-31.
- [Google Scholar]
- Vertigo: Its multisensory syndromes. (2nd ed). New York, Berlin, Heidelberg: Springer; 2003.
- [Google Scholar]
- Dizziness: A Practical Approach to Diagnosis and Management. Cambridge: Cambridge University Press; 2007.
- [Google Scholar]
- Symptoms and signs of neuro-otologic disorders. Continuum (Minneap Minn). 2012;18:1016-40.
- [Google Scholar]
- Diagnosis and initial management of cerebellar infarction. Lancet Neurol. 2008;7:951-64.
- [Google Scholar]
- HINTS to diagnose stroke in the acute vestibular syndrome: Three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009;40:3504-10.
- [Google Scholar]
- Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome. CMAJ. 2011;183:E571-92.
- [Google Scholar]
- ‘Cardiogenic vertigo’–true vertigo as the presenting manifestation of primary cardiac disease. Nat Clin Pract Neurol. 2006;2:167-73.
- [Google Scholar]
- The detailed neurologic examination in adults. Available from: http://www.uptodate.com/
- [Google Scholar]
- Clinical practice. Benign paroxysmal positional vertigo. N Engl J Med. 2014;370:1138-47.
- [Google Scholar]
- Central oculomotor disturbances and nystagmus: A window into the brainstem and cerebellum. Dtsch Arztebl Int. 2011;108:197-204.
- [Google Scholar]
- The bedside and office neuro-ophthalmology examination. Semin Neurol. 2003;23:63-76.
- [Google Scholar]
- Penlight-cover test: A new bedside method to unmask nystagmus. J Neurol Neurosurg Psychiatry. 2009;80:900-3.
- [Google Scholar]
- Epley and beyond: An update on treating positional vertigo. Pract Neurol. 2014;14:210-21.
- [Google Scholar]
- Evidence-based practice: Management of vertigo. Otolaryngol Clin North Am. 2012;45:925-40.
- [Google Scholar]
- The minimal ice water caloric test compared with established vestibular caloric test procedures. J Vestib Res. 2005;15:215-24.
- [Google Scholar]
- Vertigo and dizziness in the emergency department. Emerg Med Clin North Am. 2009;27:39-50. viii
- [Google Scholar]
- Vestibular migraine: Clinical aspects and pathophysiology. Lancet Neurol. 2013;12:706-15.
- [Google Scholar]
- Acute vertigo due to hemispheric stroke: A case report and comprehensive review of the literature. J Neurol Sci. 2014;339:153-6.
- [Google Scholar]
- Can bedside oculomotor (HINTS) testing differentiate central from peripheral causes of vertigo? Ann Emerg Med. 2014;64:265-8.
- [Google Scholar]
- Diagnostic accuracy of acute vestibular syndrome at the bedside in a stroke unit. J Neurol. 2011;258:855-61.
- [Google Scholar]
- Quantitative video-oculography to help diagnose stroke in acute vertigo and dizziness: Toward an ECG for the eyes. Stroke. 2013;44:1158-61.
- [Google Scholar]
- Bedside differentiation of vestibular neuritis from central “vestibular pseudoneuritis”. J Neurol Neurosurg Psychiatry. 2008;79:458-60.
- [Google Scholar]
- Revised criteria for suspicion of non-benign positional vertigo. QJM. 2013;106:317-21.
- [Google Scholar]
- Small strokes causing severe vertigo: Frequency of false-negative MRIs and nonlacunar mechanisms. Neurology. 2014;83:169-73.
- [Google Scholar]
- Recent advances in the diagnosis and treatment of balance disorders. J Neurol. 2011;258:2305-8.
- [Google Scholar]
- Cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS): A review of the clinical features and video-oculographic diagnosis. Ann N Y Acad Sci. 2011;1233:139-47.
- [Google Scholar]
- New therapeutic maneuver for anterior benign paroxysmal positional vertigo. J Neurol. 2009;256:1851-5.
- [Google Scholar]
- The use of retinal photography in non-ophthalmic settings and its potential for neurology. Neurologist. 2012;18:350-5.
- [Google Scholar]






