Translate this page into:
Acinetobacter lwoffi brain abscess in a post-COVID-19 patient
*Corresponding author: Santhanam Rengarajan, Department of Neurosurgery, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India. santhanamrengarajan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Krishnasamy L, Venkatraman I, Rengarajan S. Acinetobacter lwoffi brain abscess in a post-COVID-19 patient. J Neurosci Rural Pract 2023;14:549-50.
Dear Editor,
A 71-year-old man who recovered from COVID-19 pneumonia presented with seizures without any neurological deficits. Contrast magnetic resonance (MR) imaging scan brain revealed a rounded thin walled peripherally contrast-enhancing lesion in the left frontal lobe with perilesional edema, mass effect, and midline shift with few eccentric nodular areas without restriction on diffusion-weighted images with lipid lactate peak in MR spectroscopy [Figure 1]. Possibilities of neoplastic versus fungal abscess were considered. The hemorrhagic aspirate revealed Acinetobacter lwoffii sensitive to cefoperazone and meropenem. Follow-up scan showed complete resolution of the abscess [Figure 2].
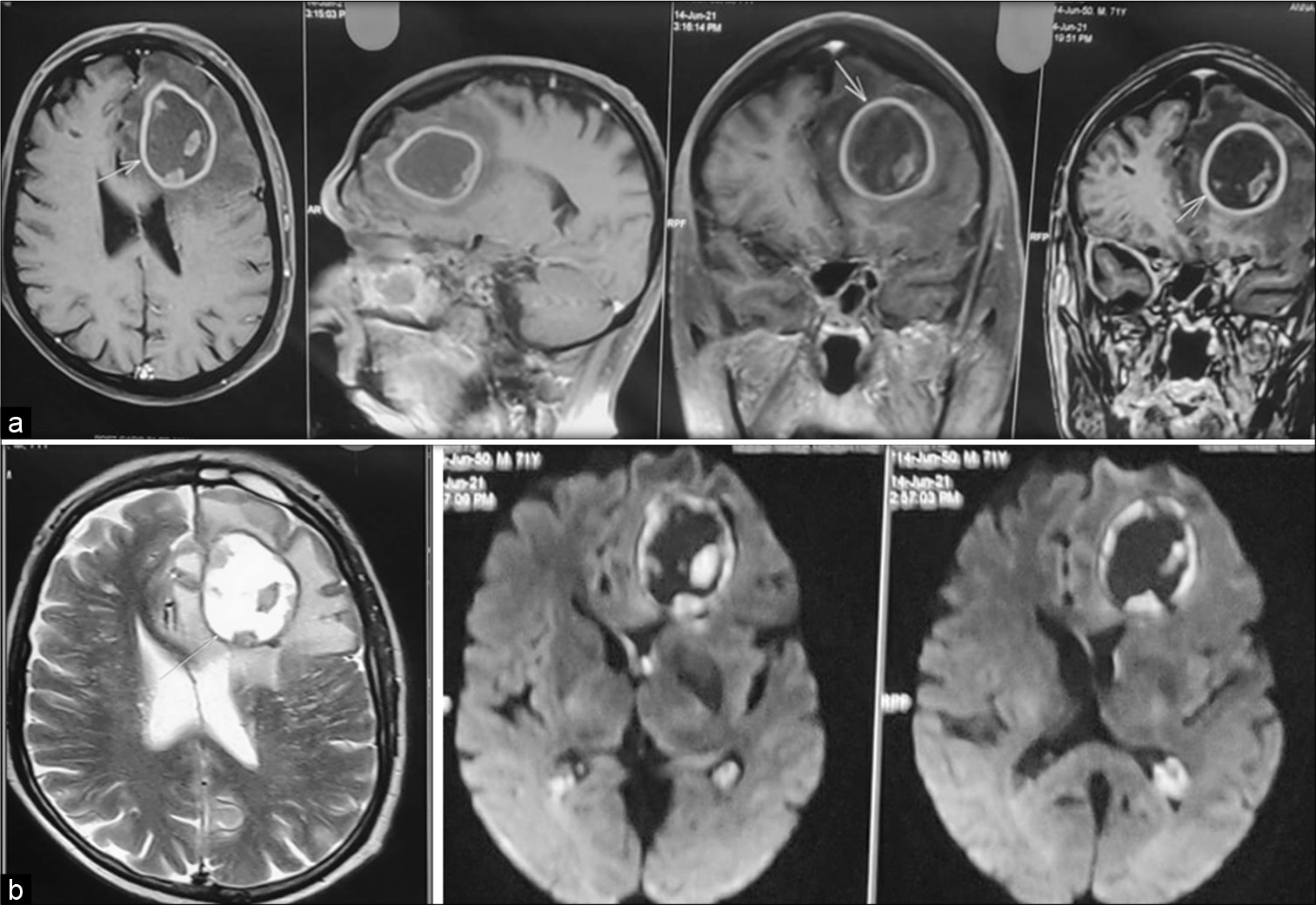
- (a) Contrast magnetic resonance imaging brain showing the left frontal peripherally enhancing cystic lesion with central non-enhancing areas and focal isointense particulate material in the walls (b) T2-weighted image showing hyperintense cyst with hypointense rim and nodular foci; Diffusion-weighted image showing lack of restriction in the contents with hemorrhagic areas in the wall of the cyst.
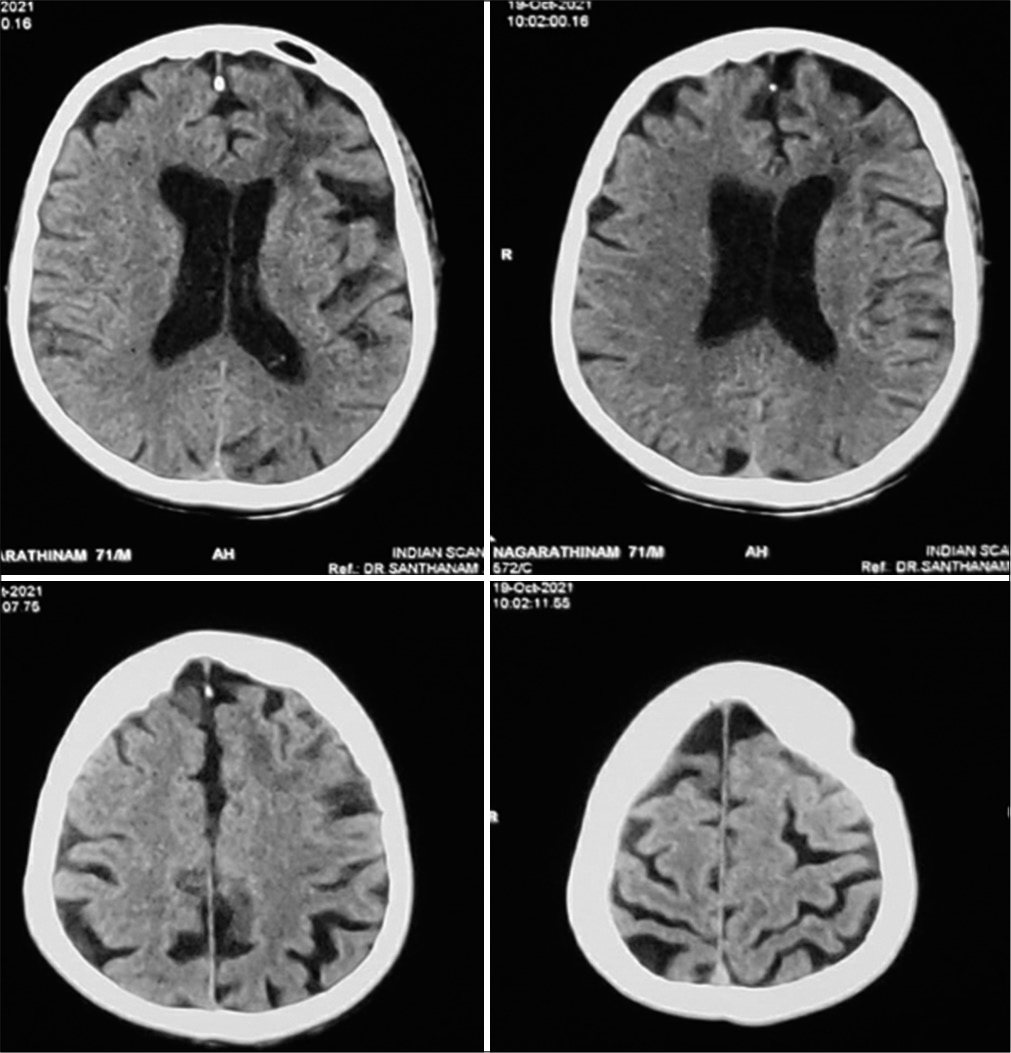
- Eight-week follow-up computed tomography showing complete resolution of the abscess with minimal left frontal gliosis.
Meningitis, ventriculitis, and brain abscess caused by Acinetobacter baumannii species have been reported earlier.[1,2] This is the first ever report of brain abscess caused by A. lwoffii. The radiological features of this case were also peculiar, though not characteristic. Absence of restriction on diffusion-weighted images in the contents of the cyst with hemorrhagic areas in the wall favored the possibility of either a neoplastic cyst or a fungal abscess and not consistent with pyogenic abscess.
Although abscesses classically show restricted diffusion in the central portion, a dual rim sign on susceptibility-weighted imaging and increased flow in perfusion imaging, exceptions have been seen in the form of low diffusion signal comparable with brain tumors. Newly formed thin vessels seen in the abscess wall may rupture with rising intracranial pressure, resulting in hemorrhage within the abscess. Thus, even though hemorrhage in brain abscess is rare, the diagnosis needs to be considered when appropriate.
Multidrug resistance among the Acinetobacter species makes the treatment of cases a great challenge. In our case, the response to cefoperazone and meropenem was good and resulted in complete clearance of the infection. The rarity of brain abscess being caused by a commonly found organism such as A. lwoffii along with peculiar radiological findings makes this case report interesting as a good learning material. The surgical strategies would be different for neoplastic lesions and obtaining the correct diagnosis early helped in avoiding major surgical interventions in this patient who was recovering from COVID pneumonia along with multiple comorbidities.
Brain abscess in humans due to A. lwoffii is being reported for the first time. The peculiar radiological features signal the possibility of alternative and uncommon diagnosis. Early diagnosis of A. lwoffii infection and appropriate antibiotic therapy based on the culture and susceptibility report is essential in preventing the emergence of antibiotic resistance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Adult Acinetobacter meningitis and its comparison with non-Acinetobacter gram-negative bacterial meningitis. Acta Neurol Taiwan. 2005;14:131-7.
- [Google Scholar]
- Brain abscess caused by multidrug-resistant Acinetobacter baumannii. Case report. J Neurosurg. 2009;111:306-10.
- [CrossRef] [PubMed] [Google Scholar]





