Translate this page into:
A series of enterococcal brain abscesses
Address for correspondence: Dr. Dhaval P. Shukla, Department of Neurosurgery, National Institute of Mental Health and Neurosciences, Bengaluru - 560 029, Karnataka, India. E-mail: neurodhaval@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Neurosurgeons in developing countries come across brain abscess frequently, but Enterococcus as a cause of abscess is rare.
Aims:
To describe clinical profile and treatment of a series of patients with enterococcal brain abscess.
Materials and Methods:
We retrospectively reviewed microbiological records of patients with brain abscess to identify Enterococcus as a causative organism.
Results:
12 patients (nine males) were diagnosed to have enterococcal brain abscess. All were due to E. species.
Conclusions:
The clinical feature and management are not different from other etiological agents. The prognosis of enterococcal brain abscess is more favourable than bacteremia.
Keywords
Brain abscess
cerebral abscess
Enterococcus
neuroinfection
Introduction
Brain abscess remains one of the commonly encountered neurologic emergencies in developing countries despite advances in neurosurgical, neuroimaging, and microbiological techniques; and the availability of new antibiotics. The successful treatment of brain abscesses requires surgery, appropriate antibiotic therapy, and eradication of the primary source. Though high mortality and morbidity has been reported, timely intervention can lead to favourable outcome.[1] The common causative organisms of brain abscess are Staphylococcus aureus, Streptococcus pneumoniae, Hemophilus influenzae, Escherechia coli, proteus, and Pseudomonas species.[1] Enterococcus is a rare cause of brain abscess. We present a series of 12 cases of enterococcal brain abscess.
Materials and Methods
We retrospectively reviewed the patients of enterococcal brain abscess treated at our institute in last 5 years. The clinical profile, microbiological characteristics, treatment, and outcome of these patients were reviewed. The drained abscess material was processed for Gram-staining, Ziehl–Neelsen staining and was cultured aerobically on blood agar, chocolate agar, MacConkey agar, Lowenstein Jensen medium, Sabouraud's dextrose agar and thioglycollate broth with overnight incubation. For the isolation of anaerobic organisms, blood agar was inoculated and incubated in anaerobic jar (Hi media gas pak) where the plates were read after 48 h. The Gram-stained smear showed pus cells with Gram-positive oval cocci in pairs with typical arrangement suggestive of E. species. Following precise aerobic and anaerobic incubations small, translucent, round α haemolytic/nonhaemolytic colony were observed. The isolates were identified as E. species after subjecting to biochemical studies like catalase test, esculin hydrolysis and ruling out, according to standard identification methods. Antibiotic susceptibility was performed according to Clinical and Laboratory Standards Institute guidelines and the different isolates were found to be variably sensitive to common antibiotics. No isolate was resistant to vancomycin.
Results
Demographics
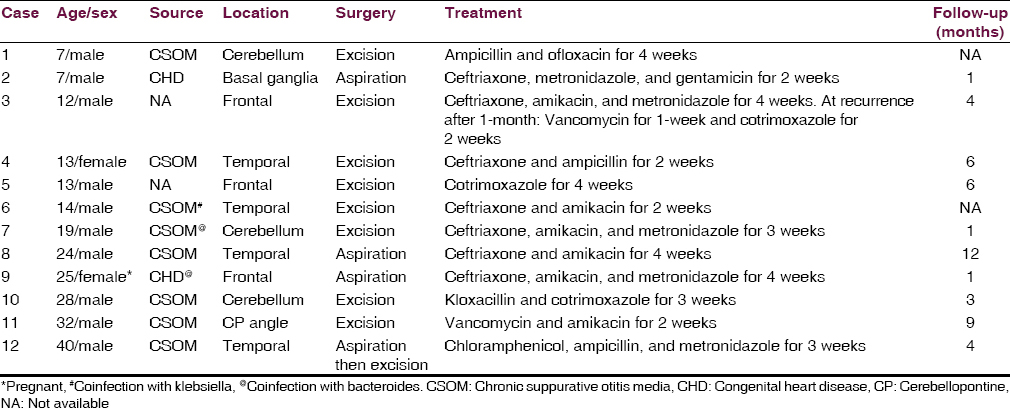
Twelve patients (nine males) were diagnosed to have enterococcal brain abscess. All were due to E. species. Children were equally susceptible like the adults. Supratentorial location was more common. All of them had raised intracranial features. Fever was present in half of them. 3 patients presented in unconscious state. Predisposing factor could be identified in 10 (83.33%); eight had chronic suppurative otitis media (CSOM), and two congenital heart disease (CHD). One lady was 2 months pregnant at the time of diagnosis, she had cardiogenic source. 1 patient had recurrent abscess due to CSOM, the causative organism of which was bacteroides in first instance and Enterococcus in second.
Treatment
Eight underwent surgical excision. 1 patient underwent burr-hole aspiration followed by surgical excision. Only burr-hole aspiration was performed in three. Enterococcus was the sole causative organism in nine. Co-infection was found in three; two were bacteroides, and other one was Klebsiella. Patients’ details are summarised in Table 1. All patients were treated with appropriate antibiotics for variable periods. There was no mortality.
Discussion
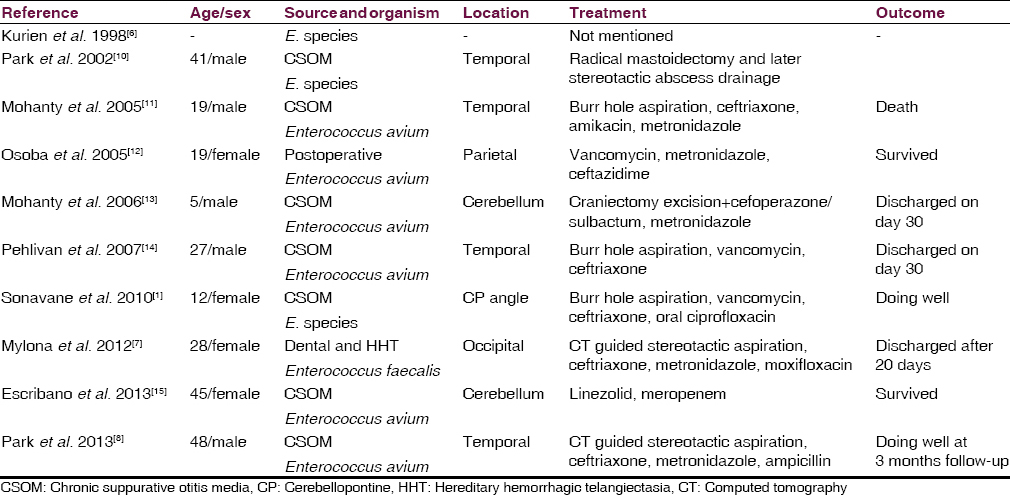
The causative pathogens of brain abscesses vary according to temporal and geographic diversity. The age, underlying medical and/or surgical condition of the patient, and possible source of infection also determine the causative organisms.[1] Once believed to be harmless, E. species is now considered as causative agent for urinary tract infections, hepatobiliary sepsis, endocarditis, surgical wound infection, bacteraemia, neonatal sepsis, and nosocomial infection with high mortality.[23] Enterococcus faecalis is the most common species associated with clinical infection, while Enterococcus faecium poses the higher antibiotic resistance threat.[4] However enterococci are considered as a rare causative pathogen for central nervous system infection, brain abscess being even rarer.[5] The true incidence of enterococcal brain abscess is difficult to determine. Kurien et al. found Enterococcus in only 1 patient among the 153 patients in their series.[6] We found only 10 cases of enterococcal brain abscess described in literature, and ours is the largest series of its kind.[178]
Clinical features
The clinical features of enterococcal brain abscess are not different from other causative organisms. It has been reported more often in younger patients.[18] In our series, half of the patients were children. Enterococcal abscesses have been commonly described in supratentorial lobar locations, cerebellum, and cerebellopontine angle. Besides these locations, we had a patient (case 2) with brain abscess in basal ganglia due to CHD. The cause of enterococcal brain abscess was CSOM in 7 cases,[18] dental procedure in a case of hereditary hemorrhagic telangiectasia in one,[7] and after neurosurgical procedure in one.[8] CHD, which was source in two of our patients, has not been reported as cause of enterococcal abscess earlier. The species of Enterococcus reported were Enterococcus avium in 6 cases, E. species in three, and E. faecalis in one.
Treatment
Most of the enterococcal abscesses were treated with aspiration, either stereotactic, or burrhole.[178] Most of our patients underwent craniotomy and excision of brain abscess, as we believe that antibiotic therapy duration can be shortened by totally excising the abscess. The antibiotic treatment is based on culture sensitivity. Vancomycin is being used often for treatment of enterococcal infection. Na et al. described 53 patients of Enterococcus bacteremia, where vancomycin was the most commonly used antibiotics.[9] The average duration of therapy was 14.3 days with a mortality of 24.5%. The common antibiotics that have been used to treat enterococcal abscess are ceftriaxone in 5 cases, metronidazole in five, and vancomycin in 3 cases. Other antibiotics that have been used are amikacin, ceftazidime, cefoperazone/sulbactum, moxifloxacin, linezolid, meropenem, and ampicillin.[178] As per our hospital policy all patients with brain abscess receive ceftriaxone, amikacin, and metronidazole. If the organisms are sensitive to these antibiotics, these are continued for variable period based on operating surgeon's discretion. There is tendency to shorten the duration of antibiotic therapy if total surgical excision is done. The common antibiotics used in our patients were ceftriaxone in 7 cases, amikacin in six, metronidazole in five, and vancomycin in 3 cases. We also have preference of prescribing oral antibiotics, hence we have used ampicillin, ofloxacin, cotrimoxazole, kloxacillin, and chloramphenicol for our patients based on sensitivity report. The antibiotic therapy duration has been variable in literature, and also in our cases. Our patients received antibiotics for 2–6 weeks. 1 patient (case 3), who had recurrence while on first line of antibiotics for 1-month, received other antibiotics for two additional weeks.
Outcome
The outcome of enterococcal brain abscess is much better than bacteremia.[9] Death was reported in only one out of 10 patients in literature. None of our patients died. The follow-up is not reported well in literature, and the treatment outcome assessment is restricted to condition at discharge. We had follow-up data of 10 patients, with a duration ranging from 1–12 months (median 4 months). Only 1 patient had recurrence (case 3) at 1-month of surgery. All other patients were doing well at follow-up. The reported cases of enterococcal brain abscesses are summarized in Table 2.
Conclusion
Enterococci are among the rare pathogens responsible for brain abscess. Though presence of it does not warrant any extra precaution, the knowledge of its occurrence will help the clinician and the microbiologists to identify and formulate treatment accordingly. Most of the enterococcal brain abscesses can be treated with ceftriaxone. Vancomycin is not required as first line of antibiotic. As compare to bacteremia the outcome of enterococcal brain abscess is favourable.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Enterococcal cerebellopontine angle abscess in a 12-year-old female. J Glob Infect Dis. 2010;2:67-9.
- [Google Scholar]
- Epidemiology and clinical outcome of enterococcal bacteraemia in an acute care hospital. J Infect. 2006;52:383-6.
- [Google Scholar]
- Activity and expression of a virulence factor, gelatinase, in dairy enterococci. Int J Food Microbiol. 2006;112:208-14.
- [Google Scholar]
- Enterococcal meningitis: A clinical study of 39 cases and review of the literature. Medicine (Baltimore). 2003;82:346-64.
- [Google Scholar]
- Otogenic intracranial abscess: Concurrent craniotomy and mastoidectomy – Changing trends in a developing country. Arch Otolaryngol Head Neck Surg. 1998;124:1353-6.
- [Google Scholar]
- Brain abscess caused by Enterococcus faecalis following a dental procedure in a patient with hereditary hemorrhagic telangiectasia. J Clin Microbiol. 2012;50:1807-9.
- [Google Scholar]
- Brain abscess caused by Enterococcus avium: A case report and review of the literature. Infect Chemother. 2013;45:335-8.
- [Google Scholar]
- Enterococcus avium bacteremia: A 12-year clinical experience with 53 patients. Eur J Clin Microbiol Infect Dis. 2012;31:303-10.
- [Google Scholar]
- Enterococcal otogenic brain abscess. Korean J Otolaryngol Head Neck Surg. 2002;45:1188-92.
- [Google Scholar]
- Enterococcus avium. An unusual cause of cerebral abscess. Neurosciences (Riyadh). 2005;10:297-300.
- [Google Scholar]
- Otogenic cerebellar abscess by Enterococcus avium, a very rare infectious agent. J Neurol Surg A Cent Eur Neurosurg. 2013;74 Suppl 1:e155-8.
- [Google Scholar]






