Translate this page into:
A giant frontal cavernous malformation with review of literature
Address for correspondence: Dr. Arvind Sharma, 22, Sunder Nagar, Civil Lines, Ajmer Road, Jaipur - 302 006, Rajasthan, India. E-mail: dr_arvindsharma@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cavernous malformations (CMs) are vascular anomalies with dilated spaces called caverns. These spaces are lined by endothelial cells and collage and devoid of smooth muscle or intervening neural tissue, and filled with blood at various stages of stasis, thrombosis, organization, and calcification. Most CMs are relatively small in size but when they are large enough they can produce sing of mass effect and may simulate neoplastic, vascular, inflammatory pathology. Giant CM (size >6 cm) are very rare lesions and very few cases are reported in world literature. We are reporting such a rare case of a 16 year male. Our case is also unique in the sense that it is the largest reported CM in Indian population.
Keywords
Cavernoma
cavernous malformation
giant
Introduction
The cavernous malformations (CMs) are well circumscribed, multilobulated occult vascular malformations. They are composed of sinusoidal vascular channels lined by single layer of endothelium called caverns.[1] There is no intervening brain parenchyma in these lesions.[2] CMs are acquired, sporadic in approximately 80% of the patients but may also be familial. CMs may vary in size from few millimeter to few centimeter with an average size of 1 cm. Lawton et al.[3] described any lesion larger than 6 cm as giant cavernoma. Here, we report a case of giant cavernoma of right frontal lobe in a young boy and a review of literature.
Case Report
A 16-year-old male presented to medical attention with a history of intermittent headache since last 1 month, particularly after doing strenuous activity. Patient advised for computed tomography (CT) scan [Figure 1] of the brain that showed a large mixed density lesion with mass effect for which he was referred to us. On examination patient was conscious, cooperative, and oriented to time, place, and person. His vitals were within normal range. He had no significant medical history, previous radiation exposure, or family history of vascular malformations. There was no sensory or motor deficit. His both fundus appears to be normal. Magnetic resonance imaging (MRI) of the brain [Figure 2] showed a large heterogenous partially hemorrhagic, multilobulated mass (68 mm × 69 mm × 74 mm) in right frontal lobe with perilesional edema and midline shift of approximately 15 mm to the contralateral side. Magnetic resonance spectroscopy performed and was nonconclusive for neoplastic pathology. CT angiography of the brain was negative for any Arteriovenous vascular malformation. After interdepartmental discussion and words with Neuroradiologist provisional diagnosis of arteriovenous malformation (AVM) with bleed or a high-grade malignancy with hemorrhage was made. After taking written and informed consent, the patient was taken for surgery. On operation table, his head end was elevated so that cerebral venous drainage improved. Question mark incision made and frontotemporoparietal craniotomy done. Dura opened after applying dural hitches. The brain was tense and edematous. A small opening was made over middle frontal gyrus, and cystic part of lesion aspirated out with help of suction. Cystic fluid was like old blood. Solid part of lesion was soft to firm in consistency and was purple green in appearance. Soft part of lesion was a suckable, but firm part was taken out in piecemeal. There was gliotic reaction all around the lesion that was left in situ. Overall, during surgery parts of the lesion bleed profusely with dark venous blood but controlled using bipolar cautery, hemostatic agents, and light pressure. Total excision of lesion was done. Immediately after surgery, the patient was arousable and moving all four limbs with obeying of commands. Postoperative period was uneventful, and the patient did not develop any neurological deficit. Histopathological examination [Figure 3] confirmed the diagnosis of CM. The patient was discharged on 10th postoperative day. Postoperative follow-up to 6 years and there was no development of new neurologic symptoms recurrence of the lesion on imaging.

- Noncontrast computed tomography scan showed a large mixed density hemorrhagic lesion with mass effect in right frontal lobe
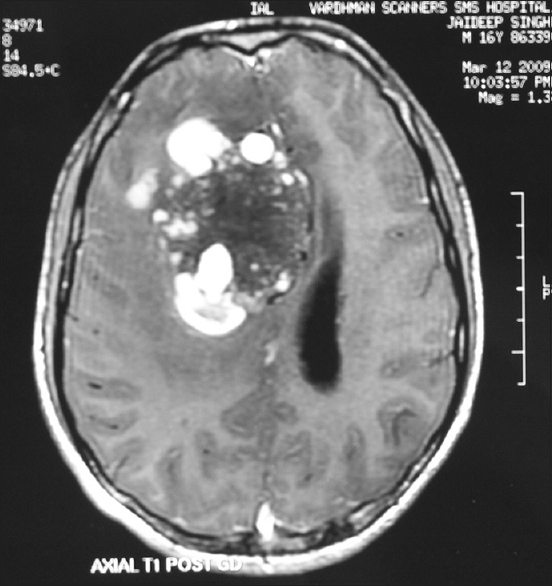
- T1-weighted axial magnetic resonance imaging scan of brain showing a large mixed intensity, hemorrhagic mass lesion of right frontal lobe causing mass effect
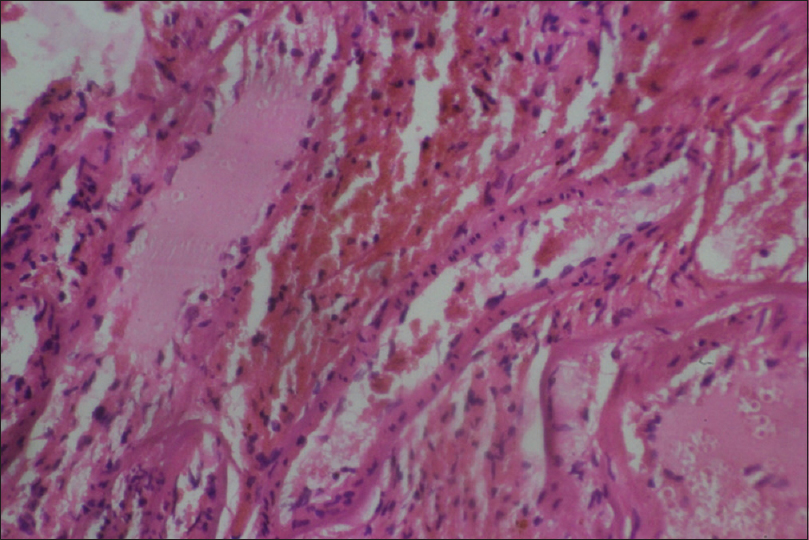
- High power magnification (H and E), stain showing sinusoidal vascular channels lined by single layer of endothelium
Discussion
CMs account for approximately 5–13% of all cerebral vascular malformations.[1] Patients with CM usually remain asymptomatic, and when they develop symptoms, Course of the disease process is usually benign. Patients present with seizure, hemorrhage, and focal neurological deficit. Our case is very special in terms of short clinical history that can make clinician in dilemma about such a rare and benign pathology. Patients having CM typically presents in 2–4 decade but also present in pediatric age group.[1] In contrast to adult patients, pediatric patients have more risk of hemorrhage.[45] Prevalence of CM in males and females is equal.[6] In some patients, CM acquired large size (i.e. giant cavernomas) because of repeated hemorrhage, followed by clot formation and organization that leads to the formation of pseudocapsule and secondary expansion.[1]
Unlike giant aneurysm, there is no precise definition of giant CM. Lawton et al.[3] first proposed an arbitrary definition of giant CM as any lesion of more than 6 cm in size. In his case report with review of literature, he describes a giant CM of 13 cm in size. Since then this criterion is accepted by world scientific community. Mottolese et al.[7] in a case series of pediatric patients describes two cases of giant CM. He described one patient with CM of 10 cm in diameter, and another of 11 cm. In India, the largest reported CM is about 5 cm.[8] These giant cavernomas are similar to average size cavernomas in clinical, surgical, and histopathological profile but different in radiological presentation[9] as these large lesions can mimic a neoplasm or an AVM bleed and even sometimes they can simulate a ruptured aneurysm with an intracranial hematoma.
Imaging of giant CM is not different from a typical size CM except that giant CM may have more heterogeneous appearance. Margins are usually well defined on imaging; rarely CM may have infiltrating margins and these lesions are termed as giant infiltrating CM.[3] In his classical case Lawton et al.[3] found similar MRI features on the initial evaluation of the patient, but gradually his patient's CM evolved into something atypical in later MRI scans, there were no large cavernous spaces; instead a speckled, heterogeneous pattern was revealed and at surgery the malformation lacked the classic mulberry appearance.
CT scan of CM usually shows blood, but MRI is the imaging modality of choice. While there are characteristic features of CMs on MRI, they are not pathognomonic. Hemorrhagic and calcified neoplasms, inflammatory/infectious nodules, or granulomas can have a similar appearance. In the case of a giant CM, the differential diagnosis may include neoplasm[10] and thus, pathologic confirmation or stability with repeat imaging over time may be needed. Giant CM may also appear cystic in nature.[9] Venous anomalies are well associated with giant CM, and this association is very important for neurosurgeons as an attempt to the removal of such venous anomaly along with CM can cause devastating venous infraction.[11]
The genetic origin and pathogenesis of giant CM is being elucidated. Integrins play major role in the pathogenesis of giant CM. Integrins are necessary for cell to cell and cell to extracellular matrix interaction in vivo. The identification of KRIT1 as a binding partner of ICAP1α[1213] suggests that KRIT1 may compete with β1 integrin for ICAP1α binding, which may then interfere with normal integrin signaling.[14] The presence of a phosphotyrosine-binding domain in malcavernin enables it to interact with KRIT1 and the cytoplasmic tail of β1 integrin, implicating it in competition for ICAP1α binding and disruption of integrin signaling. A clear understanding of these mechanisms has yet to emerge, but they may be analogs to the abnormalities of cellular signaling identified in AVMs.
Complete surgical excision is the treatment of choice of giant CMs irrespective size of lesion. The indications for surgical removal are recurrent hemorrhage, intractable seizure, and focal neurologic deficit.[15] When CM is associated with venous anomaly, only the part having CM should be removed.[9] In this case, surgery also allowed the establishment of the correct diagnosis.
Conclusion
Giant CMs are rare vascular malformations of the brain. Our case highlights that these lesions may be “giant” (>6 cm) and could be mistaken for neoplastic disease or AVM with bleed or sometimes ICH due to a ruptured aneurysm. Close surveillance of such lesions or surgical removal can help distinguish the two. Our case is unique and reaffirms that, in the large hemorrhagic lesions of the brain, CM should consider in differential diagnosis apart from above-mentioned lesions. Our case is the largest reported CM in Indian population and suggest chronic nature of disease as despite huge lesion with mass effect, the patient was relatively stable.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Giant cavernous malformation: A case report and review of the literature. J Korean Neurosurg Soc. 2008;43:198-200.
- [Google Scholar]
- Huge cavernoma with massive intracerebral hemorrhage in a child. Turk Neurosurg. 2007;17:23-6.
- [Google Scholar]
- Giant infiltrative cavernous malformation: Clinical presentation, intervention, and genetic analysis: Case report. Neurosurgery. 2004;55:979-80.
- [Google Scholar]
- Giant cavernous angioma of the temporal lobe: A case report and review of the literature. Acta Radiol. 2005;46:310-3.
- [Google Scholar]
- The natural history of intracranial cavernous malformations. Neurosurg Focus. 2011;30:E24.
- [Google Scholar]
- Central nervous system cavernomas in the pediatric age group. Neurosurg Rev. 2001;24:55-71.
- [Google Scholar]
- Cavernous angioma associated with developmental venous anomaly. J Korean Neurosurg Soc. 1997;26:1371-8.
- [Google Scholar]
- KRIT1 association with the integrin-binding protein ICAP-1: A new direction in the elucidation of cerebral cavernous malformations (CCM1) pathogenesis. Hum Mol Genet. 2002;11:389-96.
- [Google Scholar]
- Interaction between krit1 and icap1alpha infers perturbation of integrin beta1-mediated angiogenesis in the pathogenesis of cerebral cavernous malformation. Hum Mol Genet. 2001;10:2953-60.
- [Google Scholar]
- Vascular morphogenesis: Tales of two syndromes. Hum Mol Genet. 2003;12(Spec No 1):R97-112.
- [Google Scholar]
- An analysis of the natural history of cavernous angiomas. J Neurosurg. 1991;75:702-8.
- [Google Scholar]






