Translate this page into:
Neurogenic pulmonary edema due to acute respiratory distress syndrome after status epilepticus
*Corresponding author: Teruyoshi Amagai, Department of Clinical Engineering, University of Jikei Health Care Sciences, Osaka City, Japan. amagaipedteruyoshi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yoshizawa Y, Hirashima O, Uramoto S, Amagai T. Neurogenic pulmonary edema due to acute respiratory distress syndrome after status epilepticus. J Neurosci Rural Pract 2023;14:196-2.
Dear Editor,
Neurogenic pulmonary edema (NPE) is characterized by acute onset pulmonary edema after an injury to the central nerve system (CNS). The CNS insults as the cause of NPE involve traumatic brain or spinal cord injury, subarachnoid or intracranial hemorrhage, meningitis, and status epilepticus.[1] NPE is non-cardiogenic pulmonary edema that occurred after significant central nervous system insults with mortality between 60 and 100%.[2] A pathophysiology of NPE still remains unclear. The relationship between head insults and NPE might exist because increase of intracranial pressure is associated with bilateral pulmonary edema.[3]
The patient is a 34-year-old man presented to the emergency department after status epilepticus. A plain chest x-ray revealed diffuse bilateral infiltrates on both lung fields with normal sized heart [Figure 1]. As PaO2/FiO2 (= PF Ratio: Abbreviated to PFR) was 91 mm Hg <100 [Figure 2], acute respiratory distress syndrome (ARDS) was finally diagnosed using Berlin criteria. With mechanical ventilatory managements, his ARDS has been rapidly recovered under managements with mechanical ventilation and empirical broad-spectrum antibiotics [Figure 2]. P/F ratio was continuously improved and discharged 6th day without neurological impairments.

- Plain chest x-ray images. With mechanical ventilatory managements, his plain chest x-ray images revealed gradual improvement with disappearing of bilateral consolidations consistent with acute respiratory distress syndrome (ARDS). (a) on day 1, (b) day 2, and (c) day 5.
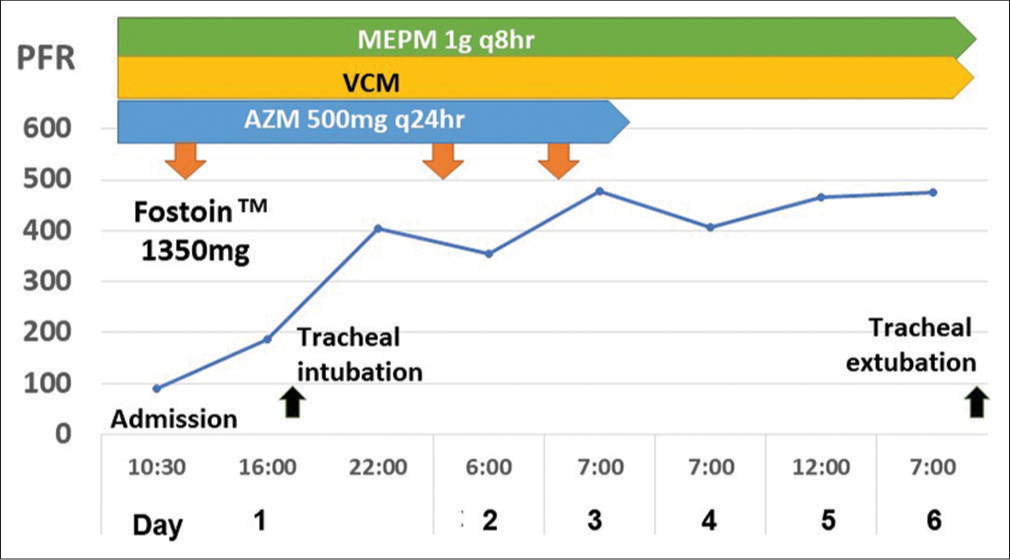
- Clinical course showing gradual neurogenic pulmonary edema due to ARDS after general convulsion. The respiratory status revealed gradual improvement from aspects of his PaO2/FiO2 ratio (PFR) during consecutive 6 days after an initiation of medical treatments. X-axis represents time in days after initial treatment with mechanical ventilatory managements, Y-axis represents respiratory oxygenized parameter using PFR in mmHg. Upper three lines represent intravenously administered antibiotics for treatment of coexisting bacterial pneumonia. AZM: Azithromycin, FiO2: Fraction of inspiratory oxygen, MEPM: Meropenem hydrate, PaO2: Partial oxygen pressure (mmHg), PFR: PaO2/FiO2 ratio, VCM: Vancomycin.
The presented patient is informative for clinicians to remind that an early diagnosis of NPE after status epilepticus must be considered to commence early treatment of ARDS and to prevent high mortality.
Acknowledgment
The authors would like to express their gratitude to the patients and their family.
Authors’ contributions
All authors contributed equally (Y.Y: literature search, discussion, and first draft; Y.F and T.A: literature search, discussion, and critical comments).
Declaration of patient consent
Informed consent was obtained from the patient for the publication of this case report. This case report was approved by the hospital ethic committee and the approval number was 2202–02.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Neurogenic pulmonary edema. Am J Emerg Med. 2021;45:678.e3-678.e5.
- [CrossRef] [PubMed] [Google Scholar]
- Neurogenic pulmonary edema in fatal and nonfatal head injuries. J Trauma. 1995;39:860-6.
- [CrossRef] [PubMed] [Google Scholar]






