Translate this page into:
Indiscriminate Use of Antibiotics in Neurotrauma Patients Referred for Expert Neurosurgical Care in a Developing Country
Amos O. Adeleye, MBBS, FWACS, FACS Department of Neurological Surgery, University College Hospital UCH, Ibadan Nigeria femdoy@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background In Nigeria, pre-neurosurgical care of most neurotrauma patients usually involves administration of many empirical agents including antibiotics with no apparent indications. This practice is fraught with two particular dangers: increase in health care costs and development of drug resistance. This study aimed to interrogate antibiotic stewardship in the pre-neurosurgical care of neurotrauma patients referred to our practice.
Materials and Methods This 7-month prospective descriptive study was performed in one University Teaching Hospital of a developing country. Clinical data on all admitted neurotrauma patients with information on the pre-neurosurgical treatment received were captured and analyzed.
Results There were 113 patients, 87(77.0%) males; 103(91.2%) had head injury, and 10(8.8%) spinal cord injury. Associated systemic injuries occurred in 47(41.6%): 40 involved skeletal and soft tissue systems, and 12(10.6%) presented with aspiration pneumonitis. These patients were referrals from public health facilities including primary health facilities (PHF), secondary (SHF), and tertiary (THF), as well as private clinics (PC). Antibiotics were given to 74 (65.5%) patients, with a probabilistic indication in only 17.6% (13/74) of these. The proportional distribution of this antibiotic administration according to the referral base was not statistically significant (χ2 =6.87, p = 0.3): 70% (14/20) from PHF, 56% (14/25) from SHF, 71% (23/32) from THF, and 63% (23/36) from PC. The antimicrobial agent administered was specified in 40 cases: Ceftriaxone was the commonest antibiotic agent implicated.
Conclusion There is apparent unnecessary exposure of patients to antibiotics in the pre-neurosurgical care of neurotrauma in this study. There is, therefore, need for education on antibiotic stewardship to the group of health workers involved.
Keywords
neurotrauma
antibiotic stewardship
pre-neurosurgical care
developing countries
Introduction
Antibiotic stewardship, that is the proper use of antibiotics in medical practice, has been a point of discussion as well as of many studies in recent years.1 2 3 4 5 When correctly deployed, the benefits of antibiotics in both prophylactic and therapeutic capacity are not in doubt.1 6 7 This is even more so in neurosurgical practice where consequences of infection can be devastating in traumatic and nontrauma-related conditions. Neurotrauma is a pandemic with significant economic burden.8 9 10 Its financial burden on the victim is perhaps worse in the developing countries where in the absence of health insurance payment for health care is funded privately by the individuals, out of pockets. Also, as a consequence of a dysfunctional health referral system, majority of neurotrauma patients in Nigeria are first seen at facilities where neither specialist service in management of neurotrauma patients nor a standardized protocol for care of such patients exists. In these settings, several and varied drug and nondrug medical agents including antimicrobials/antibiotics are routinely used in the care of these patients.
This holds great practical significance in many respects, not the least with respect to increase in the cost of care, promotion of development of drug resistance, and potentially Clostridium difficile infection, as well as unnecessary exposures to the possible risks of these agents.2 11
Our neurosurgical unit is the premier referral center for neurotrauma and other neurosurgical pathologies in our country, a large one in sub-Saharan Africa.1 In this service, referral for neurosurgical care of neurotrauma cases, especially head injury (HI), is a daily feature of our practice, sometimes coming in a deluge. Many of these referred cases of neurotrauma, including isolated, closed HI arrive from other health facilities, including tertiary hospitals, with evidence of exposures to many antimicrobials. Not only do we frequently fail to find any probabilistic reason for this use of the drugs, the antibiotics are usually those at the high end of the spectrum, especially third-generation cephalosporins. The aim of this study, therefore, is to interrogate antibiotic stewardship in the pre-neurosurgical care of neurotrauma patients referred to our practice.
Materials and Methods
This was a cross-sectional study performed at a University Teaching Hospital from a prospective database of HI for the period January-July 2016. All neurotrauma patients with referral letters to our center, in which treatment given was stated, were recruited using a previously designed proforma. We obtained information on the age and gender of the patients, the referring hospital type, administration or otherwise of antibiotics, the type of antibiotics administered, and the need or otherwise for the antibiotic administration. Patients with isolated, uncomplicated closed HI and who had no other significant extracranial injuries were deemed to have been ill-exposed if given antibiotics from the referral units.12 The patients who presented without a referral letter or in whom treatment given at the referring hospital was not stated were excluded. The data was analyzed using SPSS version 22 (SPSS Science Inc., Chicago, Illinois, United States).
Results
One hundred and thirteen patients, 87 males (76.99%), were recruited. The male to female ratio was 3.35: 1. HI accounted for 91.2% (103/113) of the patients, while 8.8% (10) had spinal cord injury. Forty-seven (41.6%) patients had associated extracranial injuries; 40 of these involved the skeletal and soft tissue systems. The sources of referrals of these patients included primary health facilities (PHF) in 20/113 (17.7%), secondary health centers in 25/113 (22.1%), tertiary hospitals in 32/113 (28.3%), and privately owned clinics in the rest 36/113 (31.9%). Twelve patients (10.6%) had clinical evidence of aspiration pneumonitis at presentation. This, usually in the presence of fever, included perturbation of the respiratory pattern, the air entry in the chest as well as the breath sounds on auscultation.
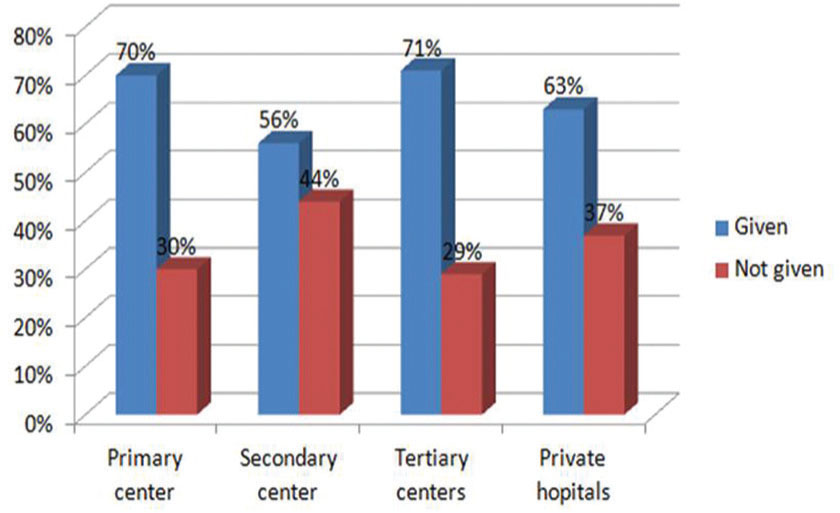
Antibiotics were reported, from the referral notes, to have been given to 74 (65.5%) patients. A probabilistic need for this administration of the antibiotics could be identified in only 13 of these (13/74) patients. The proportion of patients who received antibiotics exposure with respect to their referral sources was 14/20(70%) from primary centers, 14/25(56%) from secondary centers, 23/32(71%) from tertiary, and 23/36(63%) from private facilities, Figure 2. There was no statistically significant difference in this distribution of antibiotic use among all types of health facilities (p = 0.333). The need for the antibiotics was identified in only three patients each from primary, secondary, and tertiary centers and four patients from private facilities.
-
Fig. 2 The proportion of antibiotic administration vis-à-vis the patients' sources of referrals.
Fig. 2 The proportion of antibiotic administration vis-à-vis the patients' sources of referrals.
Of the total population (74/113) of the study subjects exposed to antibiotics before referral, the agents administered were specified in 40/74 (54.05%) cases. The commonest was ceftriaxone, a third-generation cephalosporin. It was administered as a single agent in 14 cases and in combination with other antibiotics in another 11 cases. Ceftazidime, another third-generation cephalosporin, as well as cefurox-ime, (this, a second-generation cephalosporin) was each administered once. This meant third-generation cephalosporins were administered to 65% (26/40) cases. Metronidazole, an antianaerobic antimicrobial, was the next most commonly used agent; it was administered on 45% (18/40) of the occasions (Table 1). Augmentin, an Amoxicillin/Clavulanate combination antibiotic agent, was administered in five cases.
|
Antibiotics type |
Number |
|---|---|
|
aSome of the agents were used in several combinations, especially metronidazole. |
|
|
bAmoxicillin/clavulanate. |
|
|
cEach drug used once. |
|
|
Ceftriaxone |
14 |
|
Ceftriaxone + metronidazole |
9 |
|
Augmentinb |
5 |
|
Metronidazole |
2 |
|
Ciprofloxacin + metronidazole |
2 |
|
Levofloxacin + metronidazole |
2 |
|
Ceftriaxone + gentamicin + metronidazole |
1 |
|
Ciprofloxacin + metronidazole + gentamicin |
1 |
|
Gentamicin + metronidazole |
1 |
|
Cefuroxime, ceftazidime, gentamicinc |
1 |
Discussion
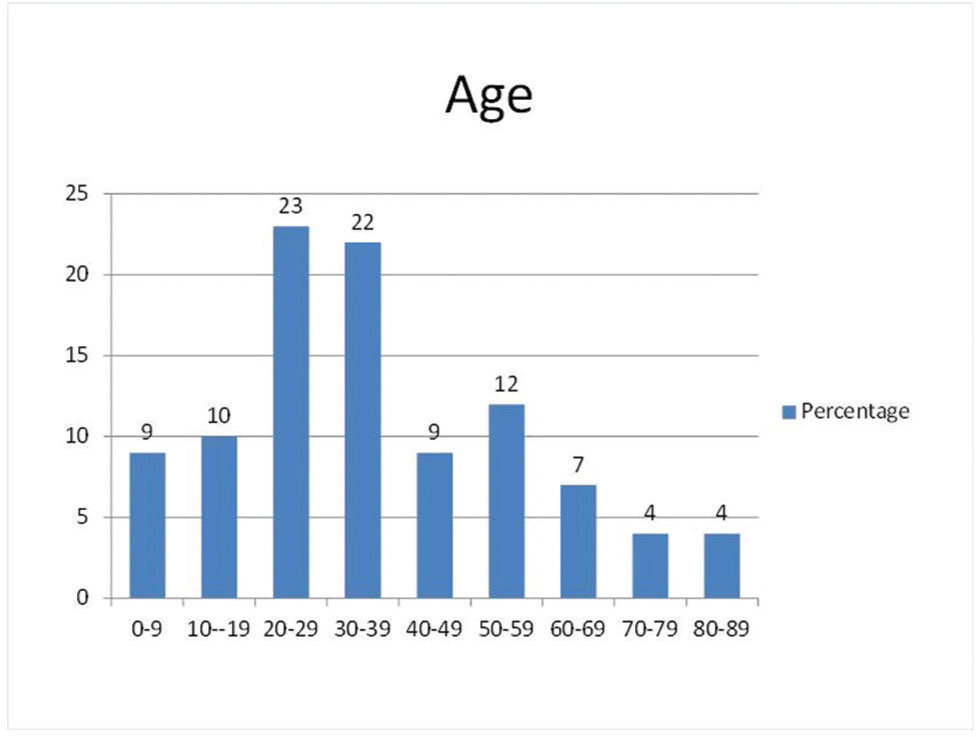
Head- and spinal cord injuries are two of the most devastating injuries following trauma,8 10 with significant attendant morbidity and mortality. The consequences of infection in this patient population can be devastating especially in the resource-poor settings of the developing countries. Isolated HIs without associated scalp wounds, as well as closed cranial calvarial vault fractures should not, other things being equal, require antibiotic treatment.13 These patients are, however, often subjected to unnecessary antibiotic administration with potentially inimical unintended consequences. We evaluated 113 patients referred with neurotrauma over the study period: 103 of the patients had HI, while 10 patients had spinal cord injury. Sixty four percent of the patients were between 20 and 49 years (Fig. 1). This is in agreement with the predominance of neurotrauma in the economically productive age groups as widely reported in the literature.8 9 10 The gender distribution of the patient showed a male predominance with male to female ratio of 3.35:1 in accordance with various previous reports.8 10
-
Fig. 1 The age distribution of the patients in this study.
Fig. 1 The age distribution of the patients in this study.
Among the patients with HI, more than half (57.28%) of the patients suffered severe HI, while additional 31.07% suffered moderate HI. This study's predominance of severe HI is at variance with most of the other reports in which mild injury is most prevalent/predominate.8 We have no practical explanation for this discrepancy but surmise that this may be a reflection of the category of patients with HI that is more likely to be referred to a specialist center, our unit being the premier national neurosurgical referral center.1 It may also be a mere reflection of the temporary, cross-sectional nature of the data capture for the study.
These patients were referrals from public health facilities including primary PHF, secondary (SHF), and tertiary (THF), as well as private clinics (PC). Twenty patients (17.7%) were referred from the PHF, while 22.1% (25), 28.3% (32), and 31.9% (36) patients were referred from the SHF, THF, and the PCs, respectively. In an earlier series on patients with mild HI from a similar setting to this study, only 39% of the patients were referred from secondary and tertiary centers, a figure that is lower than the 50.4% from the same sources in this study.14 This suggests that more severe HIs are the ones more likely to be referred for neurotrauma care in our unit, our country's national neurosurgical referral center. In another light, the relatively large percentage of patients referred from other tertiary hospitals in our country may in part be explained by absence of neurosurgeons and computed tomography scanner in some of these tertiary centers as well as the inadequate number of beds for inpatient care of these patients in some of the centers.
Antibiotics were reportedly given to 74(65.5%) patients, a probabilistic indication for which we could ascertain in only 17.6% (13/74) of these lot. A wide variety of antibiotics were administered singly or in combinations (Table 1). Ceftriaxone, a third-generation cephalosporin, was the commonest antibiotic agent implicated. It was used as a single agent in 35% (14/40) of the cases and was combined with metronidazole in another 22.5% (9/40). In actual fact, more than 65% of the patients concerned received high-generation cephalosporins without any obvious clinical justification for this. Metronidazole was especially the agent most commonly used in sundry combinations with other antimicrobial agents.
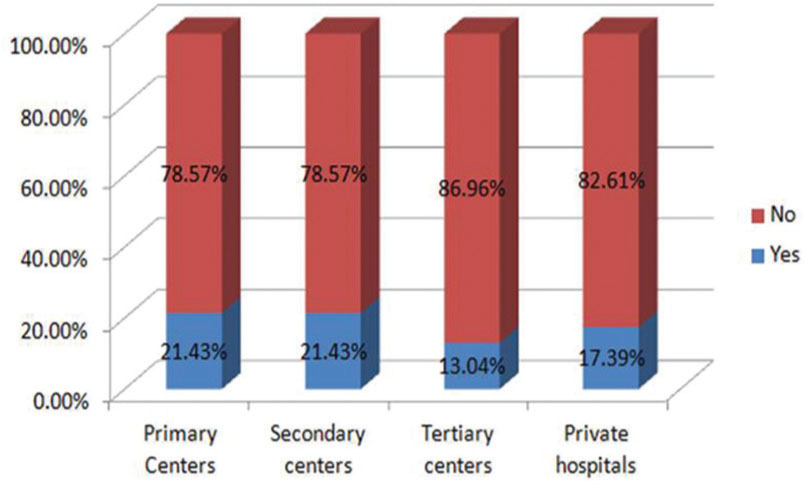
This high rate of unjustifiable administration of ceftriaxone and metronidazole noted in this study is, sadly, revealing of a high prevalence of poor antibiotic stewardship in our environment where high-grade antimicrobials are routinely prescribed by significant numbers of the practitioners without taking cognizance of the possible offending organisms or of the possible antibiotic sensitivity patterns. Augmentin (an amoxycillin/clavulanate agent targeted against penicillinase resistance) was the next commonly employed single antimicrobial, deployed in 12.5% of the cases. Levofloxacin with metronidazole and ciprofloxacin and metronidazole combination were each implicated in 5% of the cases. The proportion of patients given antibiotics, with no apparent justifiable reason, was remarkably the same for all the health institutions respectively, from the least to the greatest- the tertiary hospitals (Fig. 3). One might have expected more responsible antibiotic stewardship from the presumably more academic settings of the tertiary and/or the secondary health centers. It appears sadly, however, that changing prescribing behaviors can truly be extremely challenging among health workers.12 This particular finding of this study suggests, therefore, that there is a great deal of misuse of antibiotics going on in the care of the neurotrauma patients in our environment. The possible deleterious implications of this fact on the in-hospital outcome for such ill-exposed patients need no gainsay,15 let alone that on the efforts to combat the current global pandemic of nosocomial infections.12
-
Fig. 3 The probabilistic need for the antibiotics.
Fig. 3 The probabilistic need for the antibiotics.
Limitations
This study suffers the limitations of some of the inadequacies of its data sources in which the specific pre-neurosurgical treatments given were not stated for a significant proportion of the cases. It was also of limited duration and involved only a single unit practice in a tertiary hospital setting. The findings may, therefore, represent no more than a mere glimpse of the problem surveyed.
Conclusion
There is a high frequency of apparently unwarranted use of antibiotics in neurotrauma patients in our environment with a risk of increasing cost of care and potentially predisposing this patient population to development of drug resistance. The type of health facility, tertiary or lower ones, where these patients first present does not appear to have a bearing on this unwholesome practice. This calls for well-laid-out protocols for neurotrauma care and use of antibiotics in such patients in this environment.
Conflict of Interest
None declared.
Funding None.
References
- Pattern of referrals of head injury to the University College Hospital, Ibadan. Ann Ib Postgrad Med. 2017;15(1):34-40.
- [Google Scholar]
- Antibiotic consumption successfully reduced by a community intervention program. Isr Med Assoc J. 2007;9(1):16-20.
- [Google Scholar]
- The unintended consequences of antibiotic use. Surg Infect (Larchmt). 2016;17(6):623-624.
- [Google Scholar]
- Achievements of the Belgian Antibiotic Policy Coordination Committee (BAPCOC) Euro Surveill. 2008;13(46):19036.
- [Google Scholar]
- An antimicrobial stewardship program improves antimicrobial treatment by culture site and the quality of antimicrobial prescribing in critically ill patients. Crit Care. 2012;16(6):R216.
- [Google Scholar]
- Clinician knowledge and beliefs after statewide program to promote appropriate antimicrobial drug use. Emerg Infect Dis. 2005;11(6):904-911.
- [Google Scholar]
- STOP-IT Trial Investigators. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372(21):1996-2005.
- [Google Scholar]
- Clinicoepidemio-logical profiles and outcomes during first hospital admission of head injury patients in Ikeja, Nigeria. A prospective cohort study. Neuroepidemiology. 2009;32(2):136-141.
- [Google Scholar]
- Missing Microbes: How the Overuse of Antibiotics Is Fueling Our Modern Plagues.Hand Book of Clinical Neurology. New York: Henry Holtz and Company. L.L.C; 2014. 1st edition
- [Google Scholar]
- Epidemiology of traumatic brain injury over the world: a systematic review. Austin Neurol & Neurosci. 2016;4:e275.
- [Google Scholar]
- Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309-331.
- [Google Scholar]
- A global declaration on appropriate use of antimicrobial agents across the surgical pathway. Surg Infect (Larchmt). 2017;18(8):846-853.
- [Google Scholar]
- Antimicrobial stewardship: a call to action for surgeons. Surg Infect (Larchmt). 2016;17(6):625-631.
- [Google Scholar]
- Anticonvulsant and antibiotic prophylaxis in head injury. Ann R Coll Surg Engl. 1994;76(3):147-149.
- [Google Scholar]
- Inter-hospital transfer for neurosurgical management of mild head injury in a developing country: a needless use of scarce resources? The Indian Journal of Neurotrauma. 2011;8:1-5.
- [Google Scholar]






