Translate this page into:
Giant osteoid osteoma of the ethmoid bone with unusual large nidus
Address for correspondence: Dr. Ahmet Murat Müslüman, Avrupa Konutları TEM, B 22 Blok D: 50, Gaziosmanpaşa, Istanbul, Turkey. E-mail: mmusluman@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Osteoid osteoma (OO) is a benign bone neoplasm which is seen in the long bones of appendicular skeleton. It is rarely seen in the cranium. Ethmoid bone OO has been very rarely reported so far. We report another case of giant osteoid osteoma involving the ethmoid bone with intraorbital and intracranial extension in a 3O year old female patient. This case with unusual anatomical location was presented. It is first time reporting a giant osteoid osteoma of ethmoid bone with such a large nidus.
Keywords
Ethmoid bone
Frontobasal-transcranial approach
giant
osteoid osteoma
Introduction
Osteoid osteomas (OOs) are rare benign, slow-growing, often asymptomatic bone neoplasms, which also may involve the orbital bones. It comprises 12% of the benign osseous tumors.[1] Cranial involvement has been mainly localized in the skull vault, and OO of the cranial base is a rare entity.[2] They may occasionally grow rapidly affecting not only the paranasal sinuses but also the surrounding structures.[3] In this article, we report a case of giant ethmoid bone OO that presented with an unusually large nidus; a differential diagnosis problem was posed with osteoblastomas. The controversy on the surgical approach used was resolved after multidisciplinary evaluation, and the patient was sent to neurosurgical department for intervention through transcranial frontobasal route.
Case Report
A 30-year-old woman presented to our clinic with a 3-year onset of right proptosis and intermittent right periorbital pain, diplopia at lateral gaze, and blurred vision. The patient had no history of head trauma or paranasal sinusitis. The ophthalmological examination revealed an induration of the right medial canthal area with inferolateral displacement of the right eye with limitation of its action in lateral gaze and a slight proptosis. The right eye visual acuity was decreased to 0.4, and a deficit was observed at visual field examination. Axial and coronal computed tomography (CT) images revealed a 3 × 3– and 5 × 5–cm centrally hypodense lesion, with well-defined margins and bone density, originating from the left ethmoid sinus [Figure 1].
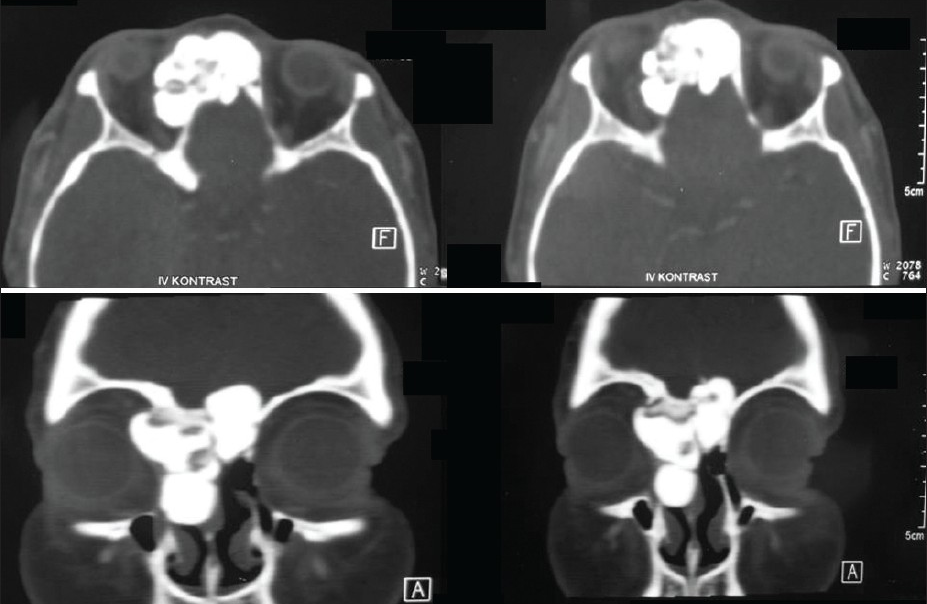
- Axial and coronal computed tomography revealed a 3 × 3, 5 × 5cm centrally hypodense lesion, with well-defined margins and bone density, originating from the left ethmoid sinus, in the right nasal cavity bounded by a septum and extending to the right orbit with destruction of lamina papyracea. By extending to and destructing the medial orbital wall, the defined mass was displacing the medial and superior rectus muscle laterally and globe anteriorly behind the equator. A mass lesion invading frontonasal commissura which transversed the median line extending into cranium was seen.
Surgical approach
A transcranial frontobasal approach was used for the removal of giant frontoethmoidal and orbital OO. Histopathological examination of the specimen verified the diagnosis of an OO [Figures 2a and b]. The postoperative course of the patient was uneventful. The headache complaint of the patient improved immediately after the surgery, and the ocular symptoms resolved completely in seven days so that she had no need to use spectacles. Coronal cranial CT images six months after the surgery demonstrated a minimally defective lamina papyracea in the right side and anterior cranial fossa and no sign was associated with recurrence [Figure 3]. At present, the patient has been symptom-free for two years.
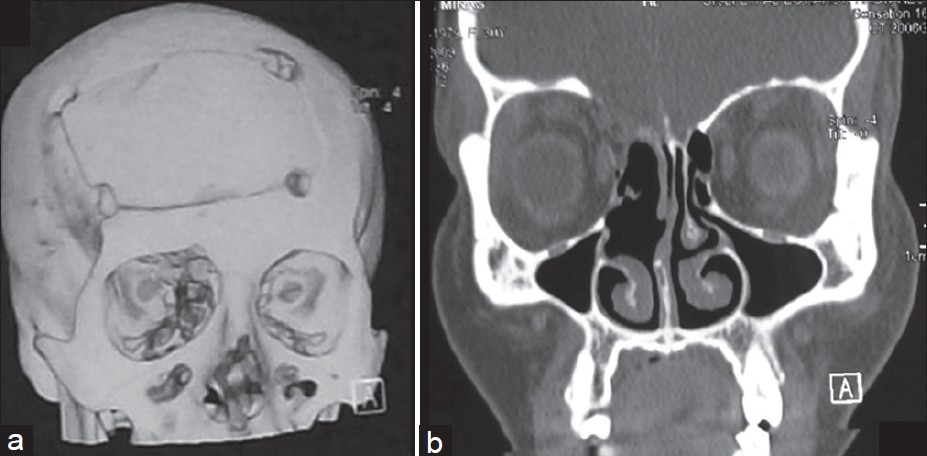
- Postoperative coronal and 3D CT demonstrated a minimally defective lamina papyracea in the right side and no sign associated with recurrence.
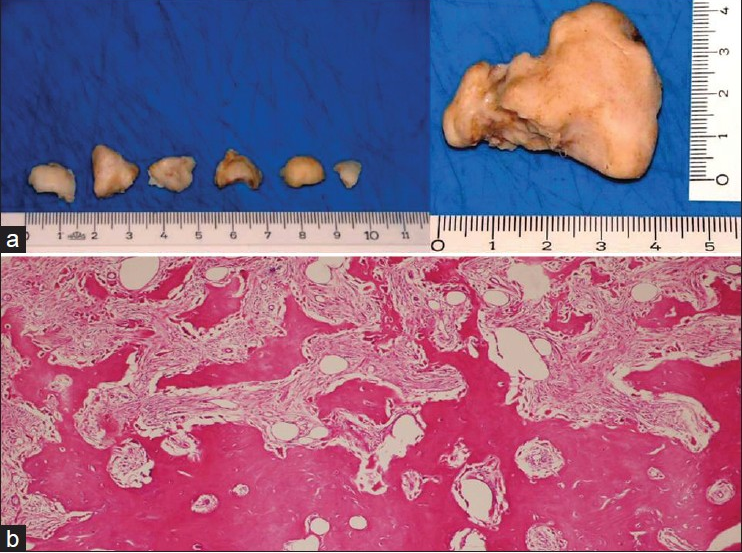
- (a) Osteoma removed en bloc and partially fragmented via transcranial frontobasal approach. (b) The specimen verified the osteoid osteoma composed of mature bone lamels and nidus which is composed of small bone trabeculae surrounded by osteoblasts.
Discussion
Surgery for osteoid osteoma
There are many operative approaches for frontoethmoidal OO. The traditional approach to small ethmoid OO is through a curvilinear medial orbital incision.[4] The transcoronal approach and a lateral rhinotomy approach to ethmoid OO extending into the orbit provide wide exposure for orbital exploration and controlled access to the superior border of the tumor and sinus.[24] The alternative approach to ethmoid osteoma is via the endoscopic route. With its recent advent, endoscopic sinus surgery is successfully used in the removal of OO in paranasal sinuses with low morbidity, superior cosmetic results, and greater experience.[5] The multicompartmental involvement warranted a multidisciplinary evaluation. Because frontoethmoidal OO had intraorbital and intracranial extensions, we previously planned to excise the osteoma via the transcranial approach and, if required, to excise the underlying part via the transethmoidal route. We achieved total excision of the OO without the aid of an otorhinolaryngologist or ophthalmologist.
Transcranial surgical approach for giant osteomata offers a safe and effective alternative with a low morbidity to the other open and endoscopic surgery used alone.
Differential diagnosis
Several problems arose in ascertaining the differential diagnosis of this case. The OO must be differentiated from osteoblastoma, sclerosing forms of osteomyelitis, ossifying fibromas, fibrous dysplasia, and osteosarcoma.[6] Osteomyelitis may form a localized abscess termed “Brodie's abscess,” which, on X-ray, can simulate the appearance of OO. However, histopathologically, Brodie's abscess shows inflammation and not a bony nidus. In our patient, there was no inflammation, and she has had large nidus [Figure 1]. To the best of our knowledge, an OO of ethmoidal bone with a large nidus has never been reported in the literature.
Radiographically, OOs exhibit a central lucency (the nidus) with patchy mineralization located centrally. The nidus is surrounded by a zone of sclerosis (the reactive zone) that can be so extensive as to obscure the underlying lesion.[7]
Radiographically, they may be indistinguishable because ossifying fibroma usually presents well-delineated radiolucency with varying amounts of radiopaque material. The difficulty arises when the tumor shows marked osteoblastic activity. In ossifying fibroma, the intertrabecular spaces should not reveal the large plump osteoblasts seen in osteoblastoma.[8] In our case, the lesion has well-demarcated margins on CT; therefore, sharpness of the borders cannot be regarded as a differentiating feature.
Histologically, OOs have variable degrees of calcification and are impossible to differentiate from osteoblastomas. Several authors have stressed the fact that the two are identical histologically, and the differentiation between them, if any, can only be on the basis of size.[9] In these cases, diagnosis is based on the size of the nidus and the presence of reactive bone formation; although active osteoblasts are more numerous, the stroma is richly vascularized, and extravasated blood with large number of multinucleated giant cell macrophages are noted. In practice, a lesion smaller than 1.5 cm is considered as OO, and a lesion larger than 1.5 cm is considered as osteoblastoma.[10] Our case is histologically unusual. The histopathological diagnosis was not based on the size of the lesion, which was more than 1.5 cm (2 × 2 × 1.5 cm), as well as on the presence of reactive dense sclerotic bone formation. In our patient, although the tumor was large, none of the abovementioned histological features of a benign osteoblastoma could be noted. We used the clinical history combined with radiographic and microscopic findings to finalize the diagnosis of OO originating from the ethmoid bone.
Conclusion
OO should be considered in differential diagnosis of the osteoblastic lesions of the ethmoid bone. Surgical management of cranial base OO may be challenging because of its proximity to vital structures, access, and hard consistency. We believe that neurosurgical transcranial approach was the best alternative for our patient for radical tumor removal, knowing that the challenging multicompartmental localization of the tumor might lead to recurrence. The interesting point of our study was the association with large nidus, which is not usual in OO, and to best of our knowledge, this is the first reported case of its kind.
Source of Support: Nil
Conflict of Interest: None declared
References
- Osteoid osteoma of the ethmoid bone associated with dacryocystitis. Head Face Med. 2006;2:23.
- [Google Scholar]
- Indications for the surgical treatment of osteomas of the frontal and ethmoid sinuses. Clin Otolaryngol Allied Sci. 1990;15:397-404.
- [Google Scholar]
- Transcoronal removal of an atypical orbitoethmoid osteoma. Plast Reconstr Surg. 1983;72:874-7.
- [Google Scholar]
- Endoscopic resection of a sphenoethmoid osteoma: A case report. Ear Nose Throat J. 1994;73:598-600.
- [Google Scholar]
- Osteoid osteoma of the zygoma: Report of an unusual case. J Am Dent Assoc. 2007;138:793-7.
- [Google Scholar]
- Update on bone forming tumors of the head and neck. Head Neck Pathol. 2007;1:87-93.
- [Google Scholar]
- Difficulty in diagnosing atypical osteoblastoma of the face: Case report. Int ArchOtorhinolaryngol. 2010;14:131-5.
- [Google Scholar]
- Osteoid osteoma. In: In Bone tumors, diagnosis, treatment and prognosis. Philadelphia: WB Sounders Company; 1991. p. :49-66.
- [Google Scholar]






