Translate this page into:
Shunt malfunction due to proximal migration and subcutaneous coiling of a peritoneal catheter
Address for correspondence: Dr. Amit Agarwal, Professor and Head Department of Neurosurgery, MM Institute of Medical Sciences & Research, Maharishi Markandeshwar University, Mullana- Ambala, 133-207, Haryana, India. E-mail: dramitagrawal@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Proximal upward migration of the shunt catheter is a rare complication of the ventriculo-peritoneal shunt for con-genital hydrocephalus.[1–15] A 5-month-old male child underwent right ventriculo-peritoneal shunt for the congenital hydrocephalus at the age of 3 months. He was doing apparently well after surgery. However, again his head started to increase in size . Also, prior to that, the mother noticed swelling over the shunt chamber region [Figure 1]. Computed tomography (CT) scan showed that the shunt was malfunctioning [Figure 2]. Repeat X-ray showed coiling of the shunt use at the level of scalp and neck [Figure 3]. The shunt revision was performed and the child is doing well. The entire length of distal tubing from a ventriculo-peritoneal shunt can migrate into the subgaleal space, and can result in shunt obstruction.[1113] The peritoneal catheters can lie in a subgaleal pocket in the occipital region in a tightly coiled fashion,[9] in the subgaleal space,[69] scalp,[2] into the scalp and the clavicular area,[2] in the subcutaneous tissues at the supraclavicular region,[16] and the thoracic wall.[15] As in the present case, it has been found that coiling of catheter takes place in the loose part of the skin[2] and most migrations occur in the early postoperative period up to 3 months.[1718] Many factors have been proposed for the development of upward migration, including the gradient between intracranial and intra-abdominal pressure as the cause of catheter displacement, the course of subcutaneous tract of the tube not being straight, incorrect fixation of the ends of the system,[19] vigorous flexion-extension movement of the head acting as a windlass and facilitating upward movement of the peritoneal catheter (windlass effect).[2612] A mechanism of “retained memory” of the shunt tubing has also been proposed as the appearance of the coiling is similar to that in the supplied packaging.[9] Tortuous subcutaneous tract associated with neck movements, negative sucking intra-ventricular pressure and positive pushing intra-abdominal pressure also have been thought to contribute to upward migration of shunt catheter.[17] A large dural hole (in the present case, this cortical mental provided more space) around the ventricular catheter may predispose to periventricular CSF collection and easy migration of the valve system,[2] and further the obstruction of the catheter allows continuous CSF flow through the dural opening leading to the formation of subcutaneous tract, which helps in the migration of the catheter and subsequent coiling.[14] The diagnosis can easily be accomplis-hed by palpation of the integrity of the drainage system and may be confirmed by shunt radiographs.[16] The treatment recommended for ventri-cular shunt migration is removal of the migrated shunt tube and replacement,[18] and this complication can be prevented by securing the shunt near the site of motion.[11]

- Clinical photograph showing the swelling at the site of shunt chamber
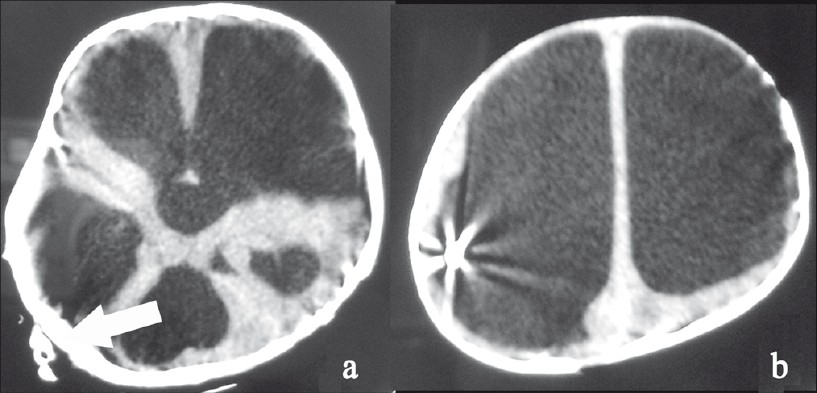
- CT scan showing subgaleal coiling of the shunt tube
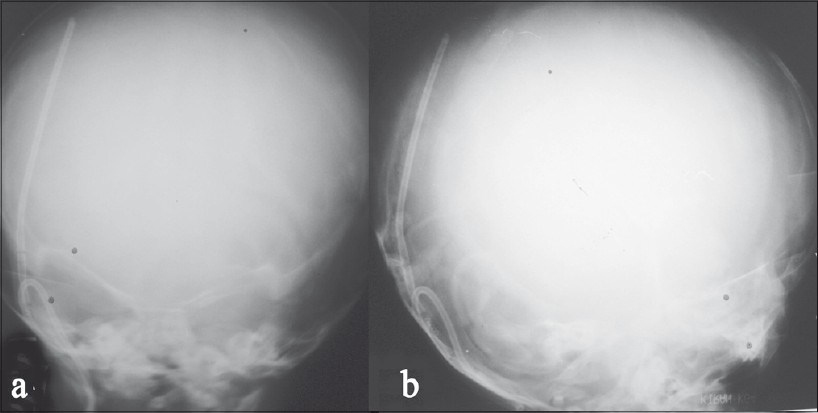
- Plain radiograph showing subcutaneous coiling of the peritoneal catheter in the patient's neck (arrows)
References
- Proximal migration and subcutaneous coiling of a peritoneal catheter: Report of two cases. Childs Nerv Syst. 1995;11:428-31.
- [Google Scholar]
- An attempt to prevent the problem of shunt-tube migration. Childs Nerv Syst. 1988;4:50-1.
- [Google Scholar]
- Extrusion of peritoneal catheter through abdominal incision: Report of a rare complication of ventriculoperitoneal shunt. Neurosurgery. 1979;5:504-6.
- [Google Scholar]
- Migration of ventriculo-peritoneal shunt into lateral ventricle of an adult. Surg Neurol. 1979;11:399-400.
- [Google Scholar]
- Retrograde migration of the venous catheter as a complication of ventriculoatrial shunts in adults. J Neurosurg. 1971;35:348-50.
- [Google Scholar]
- Sub-galeal coiling of the proximal and distal components of a ventriculo-peritoneal shunt. An unusual complication and proposed mechanism. Childs Nerv Syst. 2000;16:493-5.
- [Google Scholar]
- Duplicated peritoneal catheter as a cause of shunt malfunction. Case report. Neurosurg Rev. 1991;14:149-50.
- [Google Scholar]
- Complete migration of peritoneal shunt tubing to the scalp. Childs Nerv Syst. 1994;10:399-400.
- [Google Scholar]
- Observations on ventricular and lumbar subarachnoid peritoneal shunts in hydrocephalus in infants. J Neurosurg. 1955;12:165-75.
- [Google Scholar]
- Subgaleal migration of the distal catheter of a ventriculoperitoneal shunt. Acta Medica (Hradec Kralove). 2009;52:77-9.
- [Google Scholar]
- Upward migration and subcutaneous coiling of the ventriculo-peritoneal shunt catheter: A case report. Internet J Neurosurg. 2006;3
- [Google Scholar]
- Retrograde migration of the abdominal catheter as a complication of ventriculoperitoneal shunts: The fishhook sign. Childs Nerv Syst. 1993;9:425-7.
- [Google Scholar]
- Retrograde migration of ventriculoperitoneal shunt to the neck. Case report. Neurocirugia (Astur). 2006;17:450-2.
- [Google Scholar]
- Total intraventricular migration of unisystem ventriculo-peritoneal shunt. Acta Neurochir (Wien). 1995;136:217-8.
- [Google Scholar]
- Total migration of a ventriculo-peritoneal shunt into the ventricles. Br J Neurosurg. 1999;13:73-4.
- [Google Scholar]
- Modified method for prophylaxis against unishunt system complications with presentation of total intraventricular migration of unisystem ventriculoperitoneal shunt. Childs Nerv Syst. 1988;4:116-8.
- [Google Scholar]





