Translate this page into:
Guillain-Barré syndrome following acute viral hepatitis A
Address for correspondence: Dr. Sujit Abajirao Jagtap, Department of Neurology, Sree Chitra Tirunal Institute for Medical Sciences and technology, Trivandrum, Kerala - 695 011, India. E-mail: sujitjagtap@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
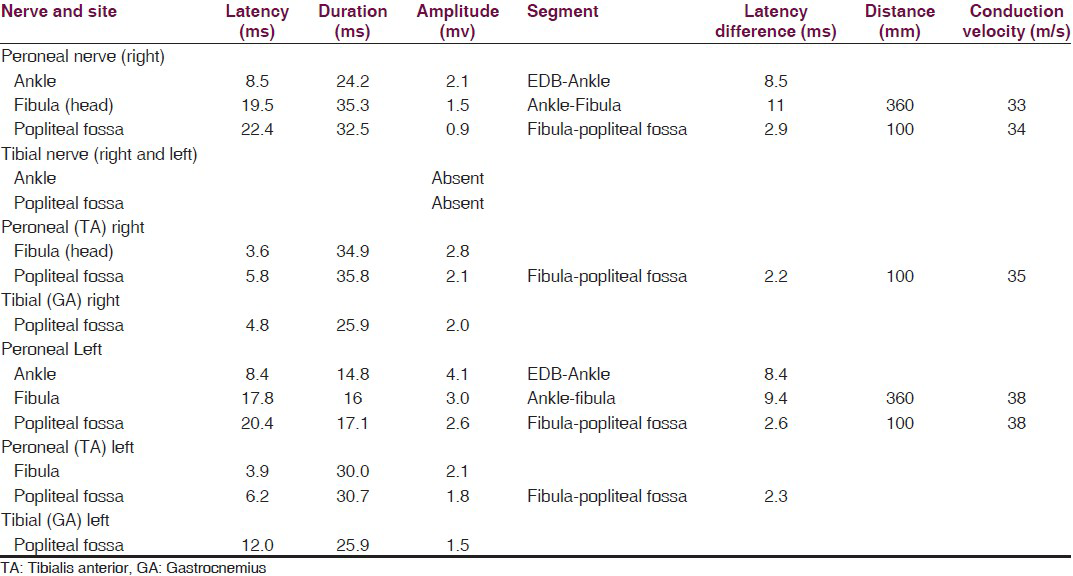
A 28-year-old male patient presented with progressive symmetric ascending distal followed by proximal weakness over two days, preceded by low grade fever, malaise, nausea and vomiting along with anorexia of two week duration. His initial evaluation at local hospital revealed features of acute hepatitis with rising levels of serum bilirubin (5.6 mg/dl), transaminitis (SGOT/SGPT - 1877/3058) without any features of hepatic decompensation. He was conscious, alert with jaundice and hepatomegaly without features of hepatic failure. His neurological examination revealed bifacial lower motor neuron weakness, generalized hypotonia with areflexia, neck muscle weakness, and upper and lower limb power of medical research council grade (MRC) 2 with distal more than proximal weakness. In view of rapidly progressive ascending flaccid areflexic quadriparesis along with bifacial weakness, the diagnosis of Guillain-Barré syndrome (GBS) was considered. His motor nerve conduction study showed significantly reduced or inelicitable CMAP from bilateral tibial and peroneal nerves without any improvement on proximal stimulation with mild prolongation of distal latencies and conduction velocities but not amounting to a coexisting demyelinating process. The F waves were either inelicitable or prolonged from all four limbs. Sensory nerve conduction study showed inelicitable SNAP amplitudes from all tested nerves except from bilateral median nerves, consistent with acute motor and sensory axonal neuropathy (AMSAN) [Table 1]. He was treated with IV IgG of 400 mg/kg/day. His biochemical evaluation showed high IgM hepatitis A antibody titer by ELISA in serum and negative serological investigations for hepatitis B, hepatitis C, hepatitis E and negative anti-ganglioside antibody. His CSF showed albuminocytological dissociation with protein of 90 mg%. After admission, he developed respiratory weakness requiring prolonged mechanical ventilation. In view of strong serological positivity for hepatitis A, the diagnosis of GBS with acute viral hepatitis A (HA) was made for which he was managed supportively. He improved slowly and is asymptomatic at 12 months follow-up.
GBS has been reported with acute viral hepatitis B, acute hepatitis C, hepatitis D, hepatitis E and rarely with HA.[1] The proposed pathology, as in C.jejuni, is that HA infection evokes an immune response, which in turn cross-reacts with peripheral nerve components because of the sharing of cross-reactive epitopes (molecular mimicry).[2] Xie et al., had considered a possible association between the GBS and HAV as out of 292,301 cases of HA in Shanghai between January and March 1988 during an epidemic, 8 had GBS.[3] A review of literature revealed only 15 reports of GBS following hepatitis A infection in adults, majority of the cases were AIDP variant, only two cases consistent with AMSAN.[45] GBS with HAV is associated with male preponderance, younger age of onset and has an overall better prognosis.[4] Although few patients have fulminant hepatitis, it did not seem to correlate with the severity of neurological symptoms. The good outcome in cases of GBS with preceding infection with HA could be a marker of a favorable prognosis unlike C. Jejuni.
References
- The spectrum of antecedent infections in Guillain-Barre syndrome: A case-control study. Neurology. 1998;51:1110-5.
- [Google Scholar]
- Guillain-Barre syndrome and hepatitis A. Lack of association during a major epidemic. Ann Neurol. 1988;24:697-8.
- [Google Scholar]
- A case of acute hepatitis a complicated by Guillain-Barré syndrome. Korean J Hepatol. 2007;2:228-33.
- [Google Scholar]
- Guillain-Barre Syndrome following fulminant viral hepatitis A. Intern Med. 1994;33:799-801.
- [Google Scholar]





