Translate this page into:
Unusual supratentorial complication following posterior fossa surgery
Address for correspondence: Dr. Alugolu Rajesh, Department of Neurosurgery, Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad - 500 082, Andhra Pradesh, India. E-mail: drarajesh1306@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Postoperative hematoma distant from the primary surgical site is a rare entity, with a reported incidence of 0.8-1.3%.[12] These have been reported to occur both ipsilaterally and contralaterally in the supratentorial compartments.[34] However, occurrence of hematoma across the tentorium has been sparingly reported, with just nine cases reported in the literature.[567] However, we have not come across any case in the English language wherein there was development of extradural hematoma on one side and subdural hygroma on the contralateral side following primary decompression of the posterior fossa tumor. Development of EDH on an intact side as compared to the side where a burr hole was made for placement of reservoir stimulates us to ponder over the possible inciting factor.
A 13-year-female child was brought with complaints of visual disturbances for 10 months, gait swaying for 3 months, and headache and vomiting for 2 months duration. Neurological examination revealed a conscious child with preserved higher mental functions. Vision acuity was perception of hand movements at 1 m. Fundus examination showed bilateral florid papilledema. Gait was ataxic. MRI brain showed a well-defined lesion of size 6 × 6 × 5.5 cm in the midline fourth ventricle with solid-cystic components extending into brainstem and middle cerebellar peduncle with hydrocephalus. The lesion was heterogeneously hyperintense on T1W, T2W, and FLAIR images. On gadolinium contrast T1W imaging, the lesion was enhancing heterogeneously. There was gross dilatation of the lateral and third ventricle with periventricular lucencies suggestive of raised ICP [Figure 1]. Our provisional diagnosis was pilocytic astrocytoma. With the patient in the prone position, and head fixed in the Mayfield head clamp with pediatric pins, a suboccipital craniectomy was performed. Following craniectomy, the dura was very tense, and hence, a burr hole at Frazier's point on the left side was made for placing an Ommaya reservoir. Guarded aspiration of CSF was done. Following drainage of approximately 30 cc of CSF, the posterior fossa dura was lax. The tumor was approached through the telo-velar approach. A near total excision of the lesion was performed and the CSF pathway was restored by confirming free flow of CSF from aqueduct. Because of poor respiratory efforts, the patient could not be weaned off the ventilator. As a precautionary measure, we connected the reservoir to drain CSF at a pressure more than 12 cm of H2O. In approximately 3 h after surgery, 50 mL of CSF was drained. There was no improvement in the sensorium and hence a CT scan of brain was performed which showed a large extradural hematoma in the right parietal region measuring 5 × 5 × 4 cm with compression of the ipsilateral lateral ventricles, midline shift of the brain parenchyma, and subdural hygroma in the contralateral side with catheter in the left ventricle [Figure 2]. Penetrations of the pin into the calvarium and coagulation abnormalities were considered to be the possible causative factors and were actively sought after. The coagulation factors were all within the normal limits (bleeding time/clotting time/prothrombin time/activated partial thromboplastin time). There were no pin marks even on the outer table. No obvious bleeding source was found following evacuation of extradural hematoma, which was controlled by placement of dural hitch stitches. The patient improved in sensorium in the immediate postoperative period to E3 M4 Vt with left hemiparesis. She, however, could not be weaned off the ventilator and succumbed to respiratory failure on postoperative day 4.
Development of extradural hematoma is a known complication due to stripping of dura from the bone following craniotomy, as is constant bleeding from the marrow breached by pins of the clamps.[16] Occurrence at a place distant to the operative site is quite puzzling, especially on the side contralateral to the placement of a burr hole and reservoir placement.
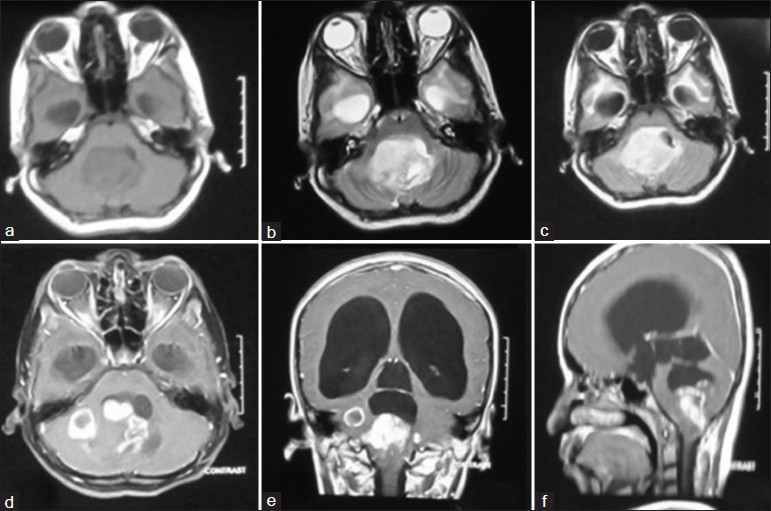
- MRI brain (axial) sections T1W (a), T2W (b), and FLAIR (c) showed a well-defined heterogeneously hyperintense lesion in the midline fourth ventricle with solid-cystic components extending into brainstem and middle cerebellar peduncle. On gadolinium contrast T1W imaging (d-f), the lesion was enhancing heterogeneously. There was gross dilatation of the lateral and third ventricles with periventricular lucencies suggestive of raised ICP
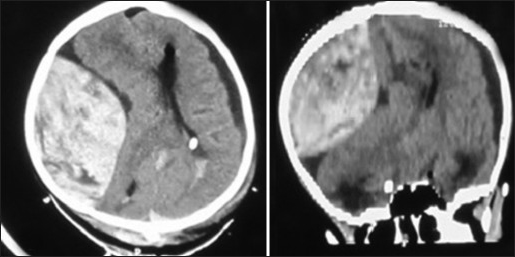
- CT scan brain axial and sagittal (reformatted) images showing a large extradural hematoma in the right parietal region with compression of the ipsilateral lateral ventricle, midline shift of the brain parenchyma. Subdural hygroma is noted on the left side
Causative factors described for development of hematomas following craniotomies are:
-
Venous rupture following snapping of subdural/extradural bridging veins, especially in the sitting position[510]
-
Intraoperative hemodynamic changes.[11]
Tsugane et al., reported five cases of extradural hematoma following posterior fossa exploration, wherein they hypothesized sudden lowering of ventricular pressure as the inciting factor.[1] Another well-known documented cause is the pin site EDH, caused by penetration of pins of the head fixation clamps.[510] However, we had used pediatric pins of the Mayfield three pin rigid fixation clamps. Moreover, there was no breach of the calvarium.
Sudden lowering of intracranial pressure following CSF drainage causes stretch on the bridging veins. Snapping the veins may cause development of extradural/subdural hematoma.[412] However, it is not clear as to what mechanisms favor a hematoma on one side and hygroma contralaterally. A possible explanation/hypothesis that can be thought off is that following tumor excision and restoration of CSF flow, negative pressure was created on either side supratentorially. On the right side, this negative pressure might have caused stripping of dura with consequent formation of extradural hematoma. While on the left side, the shrinkage might have caused peri-tubal seepage of CSF into the subdural space, leading to hygroma. Nonrecovery following a brainstem surgery could be attributed to surgical insult, and supratentorial EDH might have added to the poor outcome. Postoperative hematomas in extra-axial locations are well-known dreaded complications and can happen even across the tentorium.
References
- Extra Dural hematoma complicating ventricular decompression during posterior fossa exploration. Neurochirurgie. 1978;2:137-9.
- [Google Scholar]
- Supratentorial extradural hematomas following posterior fossa craniectomy. No Shinkei Geka. 1976;4:401-3.
- [Google Scholar]
- Multiple supratentorial epidural haematomas after posterior fossa surgery. Neurosurg Rev. 2004;27:128-32.
- [Google Scholar]
- Epidural and subdural haematomas as a complication of internal drainage of cerebrospinal fluid in hydrocephalus. Acta Neurochir (Wien). 1974;30:85-93.
- [Google Scholar]
- Remote supratentorial extradural hematoma following posterior fossa surgery. Childs Nerv Syst. 2008;24:851-4.
- [Google Scholar]
- Supratentorial hematoma during infratentorial surgery: A short series of three cases. Indian J Neurosurg. 2012;1:155-7.
- [Google Scholar]
- Supratentorial intracerebral hemorrhage following infratentorial surgery. J Clin Neurosci. 2004;11:762-5.
- [Google Scholar]
- Factor XIII deficiency as a potential cause of supratentorial haemorrhage after posterior fossa surgery. Acta Neurochir (Wien). 2010;152:529-32.
- [Google Scholar]
- Spontaneous epidural hematoma following a shunt in an infant with congenital factor X deficiency. Case report and literature review. Neurosurg Rev. 1999;22:226-9.
- [Google Scholar]
- Supratentorial intracerebral haemorrhage following posterior fossa operation. Neurol India. 2006;54:220-1.
- [Google Scholar]
- Supratentorial intracerebral hemorrhage after posterior fossa surgery. J Neurosurg Sci. 1991;35:221-4.
- [Google Scholar]
- Massive epidural haemorrhage as a complication of ventricular drainage. J Neurosurg. 1960;17:49-54.
- [Google Scholar]





