Translate this page into:
Meningoencephalitis, myositis, and rash-neurological presentation of Indian tick typhus
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Recent reports from India and other neighboring countries suggest that rickettsial diseases are one of the most surreptitious re-emerging infections associated with significant mortality and morbidity. Untreated cases can have fatality rates as high as 30–35%; however, when diagnosed promptly, they are often easily treated. Here, we narrate our encounter with a primarily neurological presentation of this new addition to the list of great mimickers in clinical medicine.
A 55-year-old homemaker from outskirts of Delhi with no known comorbidities stopped interacting with her relatives and started behaving abnormally after 3 days of high-grade intermittent fever followed by progressive drowsiness and a few episodes of vomiting. There was no history of seizures, rash, bleeding, polyarthralgia, jaundice, redness of eyes, headache, or exposure to pets. However, the patient had visited her village 1 week ago. General and systemic examination were unremarkable. Her Glasgow Coma Scale (GCS) was E3V2M5 with no apparent focal neurological deficits.
Investigations showed hemoglobin of 9.9, total leukocyte count 11,300/mm3 with neutrophilia, platelet count of 28,000. Erythrocyte sedimentation rate and prothrombin time/international normalized ratio were normal. Mild elevation of transaminases (aspartate aminotransferase (54), alanine aminotransferase (62)) and alkaline phosphatase (359) was noted while renal functions were normal. Serology for HIV, hepatitis B surface antigen, hepatitis C virus, and dengue was negative. Dengue NS1 and malaria antigens were not detected.
Contrast-enhanced magnetic resonance imaging (MRI) of the brain on admission was normal. Examination of the cerebrospinal fluid (CSF) revealed lymphocytic pleocytosis (total leukocyte count of 30/mm3, 90% lymphocytes) with high protein (148 mg/dl) and normal sugars (104 mg/dL). CSF adenosine deaminase levels were not raised; polymerase chain reaction for Mycobacterium tuberculosis and herpes simplex virus serotypes 1 and 2 and bacterial/fungal cultures were negative.
After 48 h, the patient's GCS dropped (E1V1M2) and she was mechanically ventilated. She developed new-onset generalized macular rash and was empirically started on doxycycline. Serum samples for West Nile, Japanese encephalitis, Nipah virus, and serology for rickettsial infections were sent. Electroencephalogram showed generalized non-specific disturbance of electrocerebral function. Repeat MRI of the brain showed acute infarcts in the left midbrain, right caudate, and subcortical white matter [Figure 1]. The GCS improved gradually and she was eventually extubated after 7 days. On repeat neurological examination, the patient had grade 2 power of all four limbs with diminished reflexes. A 2 Hz repetitive nerve stimulation test and nerve conduction studies did not unravel any clues. Creatine kinase levels were mildly raised (156). An MRI of the spine incidentally revealed evidence of diffuse myositis and subcutaneous edema [Figure 2]. IgM antibodies to Rickettsia conorri, the causative agent for Indian tick typhus (ITT), were identified in the patient serum sent for analysis at the National Institute of Communicable diseases. She made a slow yet steadfast recovery in her muscle power and cognitive abilities over a month's time.
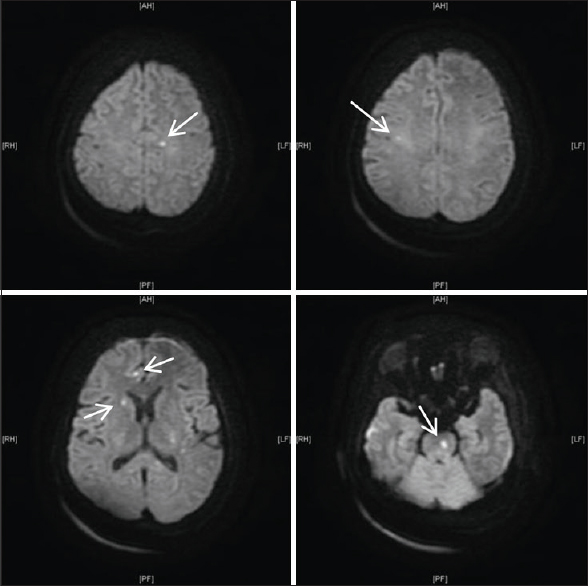
- Diffusion weighted MRI bain showing infarcts in the midbrain, caudate and subcortex
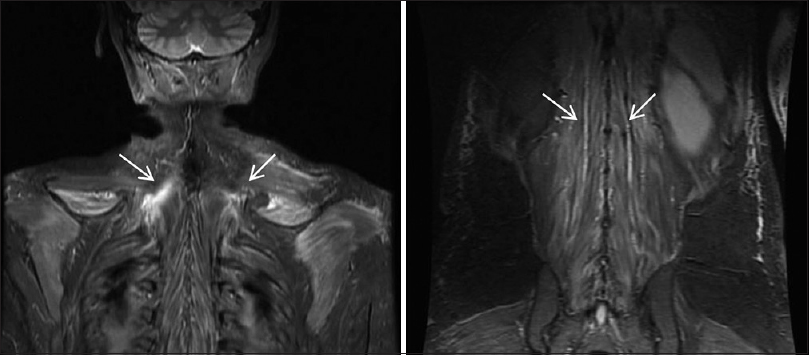
- MRI showing diffuse myositis and subcutaneous oedema
ITT caused by Rickettsia conorii subsp. indica is a disease of the spotted fever bio-group of Rickettsia, spread by the bite of an infected tick occasionally reported from Northern India.[123]
Early signs and symptoms are nonspecific. Rash which appears 5–7 days after onset can be macular, maculopapular, petechial, or hemorrhagic and rarely palpable purpura. Eschar can be single or multiple or may not be seen at all as in our case, hepatosplenomegaly, generalized lymphadenopathy, gangrene, purpura fulminans, and multisystem involvement can occur.[4] Neurological manifestations include encephalopathy, culture-negative meningitis, and myositis. However, this report is the first time that there has been an MRI documentation of cerebral infarction (as a result of infective vasculitis) and myositis.[5] Immunofluorescence assay is the recommended diagnostic test as the Weil-Felix test has low sensitivity.
Doxycycline and tetracyclines are drugs of choice while azithromycin, clarithromycin, and ciprofloxacin serve as useful alternatives
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Tick-borne rickettsioses in Pune district, Maharashtra, India. Int J Zoonoses. 1984;11:45-52.
- [Google Scholar]
- Spotted fever group rickettsioses in Himachal Pradesh. J Assoc Physicians India. 2007;55:868-70.
- [Google Scholar]
- First documentation of Rickettsia conorii infection (strain Indian tick typhus) in a traveler. Emerg Infect Dis. 2001;7:909-10.
- [Google Scholar]
- Gangrene in cases of spotted fever: A report of three cases. BMJ Case Rep 2012 2012:pii: Bcr2012007295.
- [Google Scholar]
- A case series of spotted fever rickettsiosis with neurological manifestations in Sri Lanka. Int J Infect Dis. 2012;16:e514-7.
- [Google Scholar]





