Translate this page into:
Early management of traumatic brain injury in a Tertiary hospital in Central Kenya: A clinical audit
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Traumatic brain injury (TBI) is a major cause of death and disability worldwide and is mostly attributed to road traffic accidents in resource-poor areas. However, access to neurosurgical care is poor in these settings and patients in need of neurosurgical procedures are often managed by general practitioners or surgeons.
Materials and Methods:
A retrospective clinical audit of the initial management of patients with TBI in Thika Level 5 Hospital (TL5H), a Tertiary Hospital in Central Kenya. Seventeen audit criteria divided into five clinical domains were identified and patient case notes reviewed for compliance with each criterion. Data were analyzed separately for those below 13 years owing to differences in response to brain trauma in those below this age.
Results:
Overall, there was poor compliance with audit criteria in both groups. Among those below 13 years of age, only 3 out of 17 criteria achieved compliance and 4 out of 17 criteria achieved compliance for those above 13 years of age. Assessment for the need for a cervical radiograph (7.1% and 8.8% compliance) and administration of oxygen (21.4% and 20.6% compliance) had the worst performance in both groups.
Conclusion:
Poor compliance to audit criteria indicates the low quality of care for patients with TBI in TL5H. Quality improvement strategies with follow-up audits are needed to improve care. There is a need to develop and enforce evidence-based protocols and guidelines for use in the management of patients with TBI in sub-Saharan Africa.
Keywords
Clinical audit
head injury
traumatic brain injury
Introduction
Traumatic brain injury (TBI) is defined as an acute brain injury resulting from the mechanical energy applied to the head from external physical forces. It is characterized by any one of disorientation, loss of consciousness, posttraumatic amnesia, or other neurological abnormalities.[1] TBI is estimated to affect approximately 10 million people worldwide every year[23] and it is predicted to be the major cause of death and disability worldwide by the year 2020.[3] In Kenya, it accounts for up to 7% of all surgical admissions majority of which are due to road traffic accidents.[4]
In order to avoid mortality, optimal management of TBI at the first point of contact with the healthcare system entails prevention or early correction of cerebral edema due to hypoxia, hypoglycemia, hyperthermia, infection, and hypovolemia.[567] However, owing to an increase in motor vehicles, the morbidity and mortality attributed to TBI is set to increase in low and middle-income countries (LAMICs)[38] where access to neurosurgical care remains very limited.[910] As such, there is an urgent need to enhance the quality of care offered at first point of contact. We conducted a clinical audit of the care delivered to patients with TBI at a busy regional hospital in Central Kenya with the aim of assessing the quality of initial care offered and identifying areas in need of improvement.
Materials and Methods
Setting
The project was carried out in the casualty department of Thika Level 5 hospital (TL5H), located in Kiambu County in Central Kenya. TL5H is a government hospital which serves a mixed rural and urban population offering both outpatient and inpatient services. The casualty department serves as the emergency department and attends to a wide variety of surgical emergencies. It is staffed by nursing officers, medical officer interns (MOI), MO and consultant surgeons. All patients admitted to the casualty department are regularly reviewed by the MOIs and MOs as well as by the surgeon on call. The department has prompt access to basic laboratory services as well as radiological services including X-ray and ultra-sonography. Computed tomography (CT) scan is not immediately available within TL5H, but can be obtained within Thika town at the patient's own cost. A well-equipped ambulance is readily available in case there is a need for referral.
Study participants
Adult and pediatric patients admitted to the casualty department of TL5H with a diagnosis of TBI as defined by the World Health Organization[1] were included in the study.
Study design, data collection, and analysis
This was a retrospective clinical audit project. Permission to conduct the audit was granted by the TL5H Ethics and Research Committee. A standard approach for conducting clinical audits was followed.[11] The first step was the identification of standard audit criteria through literature review and a focused group discussion. Five domains relevant to the early assessment and management of patients with TBI were identified: Primary survey, history, neurological assessment, radiological investigation, and management plan. Thereafter, case notes for all patients admitted to the casualty department with a diagnosis of TBI within the previous 3 months were retrieved. A data extraction form was designed and used to collect data by examining patient case notes for demographic characteristics and indicators that audit criteria had been met. Compliance with each criterion was recorded as a categorical variable (yes/no). Percentage compliance with each criterion was calculated as the proportion of selected patient case notes in which the criterion was fulfilled. In order to judge a criterion as complied with, there had to be at least 90% compliance. Due to a difference in response to brain trauma, data for patients below 13 years of age were analyzed separately. Epi Info 7 (CDC, Georgia) was used for data analysis.[12]
Results
Patient selection
A total of 93 case notes with a diagnosis of TBI were identified for review from the casualty admissions register. Of these, 5 case notes could not be retrieved, and 6 case notes were subsequently found not to be TBI cases. Therefore, 82 case notes were analyzed.
Patient characteristics
Of a total of 82 patients, 14 (17.07%) were children aged 13 years or less. The mean age for this group was 5.1 years (standard deviation 2.8 years). For the 68 patients with age more than 13 years, mean age was 29.8 years (standard deviation 9.6 years). The cause of injury, TBI classification and patient disposition are summarized according to age in Table 1.
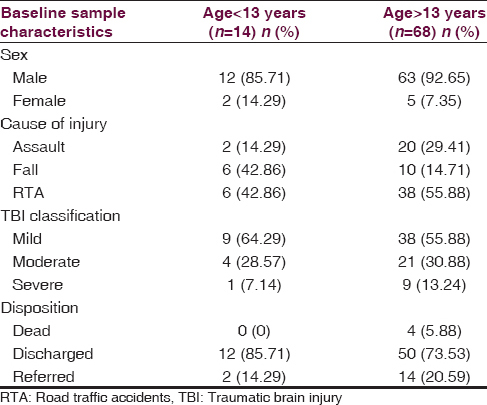
Compliance to audit criteria
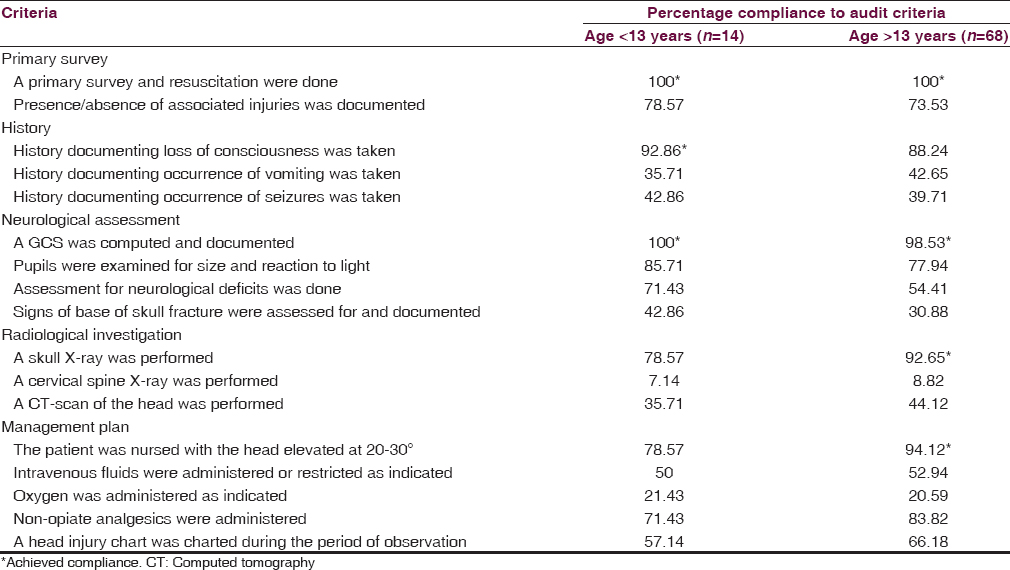
Overall, there was poor compliance with the audit criteria. Only 3 out of 17 criteria achieved compliance among those below 13 years, whereas 4 out of 17 criteria achieved compliance among those above 13 years. Table 2 shows the level of compliance to each criterion in the 5 categories assessed stratified by age. Assessment for the need for a cervical radiograph and administration of oxygen were particularly dismal in both groups.
Discussion
TBI is a major global public health problem, and LAMICs are disproportionately affected with a higher incidence of TBI compared to the rest of the world.[9] Access to neurosurgical care remains limited, and the majority of TBI patients are cared for by general practitioners and/or surgeons. In this audit, we assessed the process of care offered to patients with TBI in a busy regional hospital in Central Kenya. Seventeen criteria divided into five clinical domains were assessed. Overall, there was poor compliance with these criteria signifying a low level of quality of care. This finding is similar to that reported by Alexander et al. in KwaZulu-Natal, South Africa.[9] However, a direct comparison would be inappropriate since different criteria were employed.
The key issue in the management of TBI is the prevention and early detection of secondary brain injury, and this must be adequately reflected in the patient's assessment and management plan. We divided our audit criteria into five clinical domains reflecting this process. While most of the criteria achieved more than 50% compliance, they did not reach the 90% threshold. Reasons for this may be varied, but it is possible that poor documentation is a factor, which may be corrected through regular audits with feedback to concerned clinicians. Further, given their widespread success, some studies suggest the need for protocols in order to guide clinicians in the management of TBI patients.[913]
Performance of a cervical spine (c-spine) X-ray had the poorest compliance in both groups, signifying a low level of suspicion for concomitant c-spine trauma in patients with TBI. This is not unique to our hospital as Alexander et al. report a similar finding.[9] While only 3% of patients with blunt trauma sustain spinal fracture or dislocation, any resultant neurological injury can be devastating.[14] However, determining which stable trauma patients require c-spine imaging can be difficult given that the majority of TBI patients have a mild injury. The NEXUS low-risk criteria and the Canadian c-spine rule are tools that can be used to determine the need for c-spine imaging.[1516] However, they need to be validated in resource-poor settings. Regardless, the importance of clearing the c-spine of any injury cannot be emphasized enough.
In both groups of patients, the use of oxygen was dismal. This may be explained by a number of factors. First, the majority of the patients in our series had mild or moderate TBI for which oxygen is not often required. Second, availability of oxygen is not optimal. The casualty department at TL5H lacks a system for piped oxygen, and there are few working oxygen concentrators. As such, the use of supplemental oxygen for TBI patients is erratic and inadequate as is reflected in our results. Alexander et al. also reported the poor use of oxygen among their TBI patients.[9]
Less than half of the patients in our series were assessed for basilar skull fractures. These fractures represent a surgical emergency for which immediate neurosurgical consultation should be sought. CT scan is the best modality of detecting such injuries. However, in 11–45% of cases they present with rhinorrhea and/or otorrhea, which signify a breach of the brain's dural covering with subsequent risk for meningitis.[171819] Since majority of cerebrospinal fluid (CSF) leaks resolve spontaneously within 1-week and do so without central nervous system complications,[2021] some studies suggest that antibiotics are only warranted if CSF leakage continues for more than a week.[22] However, such guidance may not be appropriate in LAMICS where infectious encephalopathies are prevalent.
CT scan is the imaging modality recommended for assessment of intracranial pathology in patients with TBI.[7923] While it is readily available within Thika town, <½ of the patients in our series had one done probably due to its great cost. Coupled to the risks of the high dose of radiation encountered, these factors have led to the proposition of CT scan rules in order to maximize utility.[24] Regardless, it would be prudent for LAMICs to invest more in CT scanners as the use of CT scan provides for optimal management.[9]
Only 64.63% of patients had a head injury chart instituted. Similar results have been reported elsewhere in Africa.[9] However, even among those patients with charts, the issue of the quality of observations and how often these observations lead to intervention arises. In our setup, the head injury chart is filled by the nurse on duty. In the absence of specially trained nurses and doctors, subtle neurological cues may be missed with consequent poor management. It would be prudent to train more nurses in neurosurgical care if the quality of observations is to be improved. Further, regular refresher courses for doctors (and nurses) involved in the care of TBI patients is important. This is of utmost importance given that access to specialist neurosurgical care in Africa is projected to remain limited.
Overall, 16 patients in our series were referred for the neurosurgical care of whom 68.8% did not have a CT scan performed, and the majority had moderate or severe TBI (results not shown). This implies that the need for CT scan prompted referral. Four patients in our series died. All were above 13 years of age, male and aged between 20 and 45 years (results not shown). The assault was the major cause of TBI. Two of these patients (one with mild TBI and the other with moderate TBI) did not have a head injury chart. As such, it is possible that the onset of secondary brain injury in these patients was not detected early enough to begin the necessary management.
Our results strongly suggest the need for quality improvement (QI) strategies in order to enhance the quality of care delivered to patients with TBI. Key among these is the development and enforcement of evidence-based TBI management protocols. Thereafter, the use of audit and feedback can be used to gauge their utilization and identify areas in need of improvement. So far, the available protocols and guidelines have been drafted for resource-rich settings[23] and it may be inappropriate to use them in LAMICs. A multidisciplinary approach involving clinicians, researchers and policy makers is required in order to develop and enforce evidence-based guidelines suited for LAMICs.
Our study is not without limitations. The small sample size and the use of criteria tailored for our setup affects the external validity and generalizability of the project, even to areas within sub-Saharan Africa. Indeed, direct comparison with similar audits in Africa is hampered by the different criteria used. Further, in as much as our audit assessed the process of care offered to TBI patients, we were unable to assess the impact of our findings on the outcome of TBI. However, our audit was performed on the backdrop of clearly defined, measurable and practical criteria with relevance to the early management of TBI in resource-poor settings. As such, this study paves the way for future quality assessment and improvement initiatives for TBI management in sub-Saharan Africa. Further, our separate analysis of children below 13 years takes into account the impact of TBI on the developing brain and highlights the differences in the management of children with TBI.
In conclusion, this study reveals a low quality of care for patients with TBI in our setup. There is a need for a multidisciplinary team consisting of clinicians, researchers, and policy makers to develop and enforce evidence-based guidelines and protocols relevant to the management of TBI in LAMICs. Larger, multicenter, and prospective clinical audits with feedback (to concerned healthcare practitioners) could be a useful QI strategy in the management of TBI.
Acknowledgments
We are grateful to the Medical Superintendent of TL5H and all the staff in the Department of Surgery for the support rendered during the conduct of the audit.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Methodological issues and research recommendations for mild traumatic brain injury: The WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;43(Suppl):113-25.
- [Google Scholar]
- Examination of the management of traumatic brain injury in the developing and developed world: Focus on resource utilization, protocols, and practices that alter outcome. J Neurosurg. 2008;109:433-8.
- [Google Scholar]
- The impact of traumatic brain injuries: A global perspective. NeuroRehabilitation. 2007;22:341-53.
- [Google Scholar]
- Surgical admissions to the Rift Valley Provincial General Hospital, Kenya. East Afr Med J. 2002;79:373-8.
- [Google Scholar]
- Bailey and Love's Short Practice of Surgery. (25th ed). London: Hodder Arnold; 2008.
- [Google Scholar]
- Management of traumatic brain injury: Some current evidence and applications. Postgrad Med J. 2004;80:650-3.
- [Google Scholar]
- An audit of the quality of care of traumatic brain injury at a busy regional hospital in South Africa. S Afr J Surg. 2009;47:120.
- [Google Scholar]
- Outcome of head injuries in general surgical units with an off-site neurosurgical service. Injury. 2007;38:576-83.
- [Google Scholar]
- Using criteria-based audit to improve the management of postpartum haemorrhage in resource limited countries: A case study of Malawi. Matern Child Health J. 2009;13:873-8.
- [Google Scholar]
- Comparative genomic hybridization analysis of astrocytomas: Prognostic and diagnostic implications. J Mol Diagn. 2004;6:166-79.
- [Google Scholar]
- Effect of guidelines on management of head injury on record keeping and decision making in accident and emergency departments. Qual Health Care. 1994;3:86-91.
- [Google Scholar]
- Astrocytic gliomas: Characterization on a molecular genetic basis. Recent Results Cancer Res. 1994;135:33-42.
- [Google Scholar]
- Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-radiography Utilization Study Group. N Engl J Med. 2000;343:94-9.
- [Google Scholar]
- The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286:1841-8.
- [Google Scholar]
- Temporal bone fractures: Otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J Trauma. 1999;47:1079-83.
- [Google Scholar]
- Current perspective on temporal bone trauma. Otolaryngol Head Neck Surg. 1997;117:67-71.
- [Google Scholar]
- Cerebrospinal fluid leakage complicating skull base fractures: Analysis of 81 cases. Neurosurg Rev. 2006;29:64-71.
- [Google Scholar]
- Acute traumatic CSF fistulae: The risk of intracranial infection. Br J Neurosurg. 1990;4:381-5.
- [Google Scholar]
- Management of complications from 820 temporal bone fractures. Am J Otol. 1997;18:188-97.
- [Google Scholar]
- New Zealand Guidelines Group. Traumatic Brain Injury: Diagnosis, Acute Management and Rehabilitation. Wellington: New Zealand Guidelines Group; 2007.
- [Google Scholar]
- Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294:1511-8.
- [Google Scholar]






