Translate this page into:
Infratentorial posterior circulation stroke in a Nigerian population: Clinical characteristics, risk factors, and predictors of outcome
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Posterior circulation stroke (PCS), though less common, differs from stroke in anterior circulation in many aspects. Relatively, it portends a poorer prognosis. However, there is a paucity of data from African countries, in particular, where stroke is a menace.
Objective:
The study aimed to evaluate the etiology, clinical characteristics, outcome, and predictors of outcome in a cohort of patients with IPCS in Northwestern Nigeria.
Materials and Methods:
Out of 595 patients with stroke, we prospectively analyzed 57 patients with PCS in a Tertiary Care Center in Kano, Northwestern Nigeria. Patients were analyzed for demographic data, risk factors, clinical characteristics, stroke subtypes, mortality, and predictors of mortality.
Results:
Posterior circulation ischemic stroke accounted for 57 (9.6%) of 595 of all strokes seen in the study period. They comprised 44 males (mean age 47.8 ± 17.7) and 13 females (mean age 46.3 ± 13.7). Overall, their age ranged between 24 and 90 (mean age 47.4 ± 16.7). However, 52.7% of the patients were < 45 years of age. The most common site affected was the cerebellum seen in 33 (57.9%) patients. Hypertension was the most common risk factor (86%). Headache and vertigo were the most common features accounting for 83.6% and 86.3%, respectively. Thirty-eight (66.7%) patients had an ischemic stroke. Twenty-one (36.8%) of the patients died during the 1-month period of follow-up. Independent predictors of death in the study were hyperglycemia on admission and hemorrhagic stroke.
Conclusions:
IPCS occurred in a relatively younger age group. Headache and vertigo were the most common symptoms. The independent predictors of death in the study were hyperglycemia at presentation and hemorrhagic stroke.
Keywords
Infratentorial
posterior circulation
stroke
Introduction
Posterior circulation stroke (PCS) is less common than stroke involving the anterior circulation stroke (ACS). PCS, which can be infratentorial (IPCS) or supratentorial (SPCS), account for 10–15%[1] of all types of strokes. The area includes brainstem, cerebellum, occipital lobes, and thalamus and is supplied by 2 vertebral arteries, 1 basilar artery, and 2 posterior cerebral arteries.[23]
IPCS differs from ACS in the area of etiology, clinical features as well as associated morbidity and mortality. Its manifestations may include brief or minor brainstem symptoms and are more difficult to diagnose than ACS. Common infratentorial posterior circulation symptoms include visual disturbance, vertigo, and ataxia.[4]
Delayed or incorrect diagnosis of this stroke subset may have devastating consequences such as potentially preventable death or severe disability.[4] Therefore, healthcare professionals in the emergency settings and outpatient clinics need to be acquainted with the features of the acute neurological deficits associated with IPCS.
However, there is a scarcity of hospital statistics available for IPCS in Nigeria. Against this background, we evaluated the clinical characteristics, risk factors, outcome, and predictors of outcome of PCS in Northwestern Nigeria.
Materials and Methods
Out of all stroke patients seen from June 2007 to June 2013, persons with IPCS presenting in the emergency unit and a neurology clinic of a tertiary hospital in Kano were recruited for the study. All the patients enrolled were assessed by clinicians experienced in the subtlety of stroke diagnosis, typing, and management. Classification of stroke into hemorrhagic and infarctive subtypes was based on computed tomography brain and/or brain magnetic resonance imaging (MRI). The diagnosis of posterior circulation was made when the patient had a clinical stroke syndrome compatible with the involvement of posterior circulation territory and neuroimaging evidence. Patients with neuroimaging that showed recent infarction or hemorrhage in the ACS, SPCS, and other nonvascular lesions were excluded from the study. Patients with ambiguous clinical and/or radiological diagnosis of stroke were also excluded from the study. A detailed history was obtained from the patient or a close relative regarding the onset of stroke, demographic data, risk factors and family history, risk factors, clinical characteristics, stroke subtypes, and mortality. A detailed physical examination was carried out in accordance to the proforma, including vital signs and detailed examination of other systems. The patients were managed based on the stroke guideline of the hospital. Each diagnosed patient was followed up for 30 days until either death at the hospital or discharge.
Analysis of data was carried out using the “Statistical Package for Social Sciences” (SPSS) program for Windows version 16.0 (SPSS Inc., Chicago, IL, USA). Mean and standard deviation were used to describe quantitative variables. Bivariate analysis was carried out using Pearson Chi-square or Fisher exact test for categorical variables. Student's t-test was used to compare the means of continuous variables and scores on Glasgow coma scale (GCS) were compared using a Mann–Whitney U-test. Multiple logistic regression model was used and the covariates were adjusted for each independent (regression) variable to find independent predictors of in-hospital mortality. P < 0.05 was considered as a statistically significant level.
Result
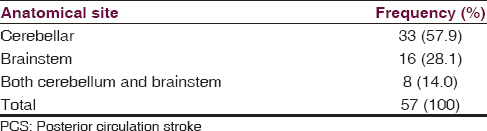
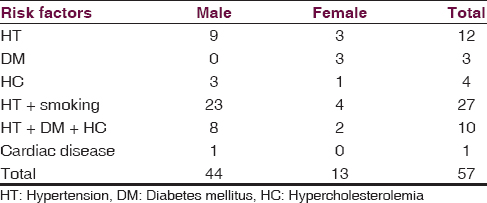
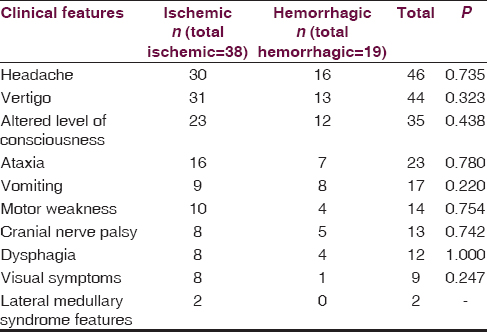
IPCS accounted for 57 (9.6%) of 595 of all strokes seen in the study period. They comprised 44 males (mean age 47.8 ± 17.7) and 13 females (mean age 46.3 ± 13.7). Overall, their age ranged between 24 and 90 (mean age 47.4 ± 16.7). However, 52.7% of the patients were < 45 years of age. The most common anatomical site affected was the cerebellum, which was seen in 33 (57.9%) patients [Table 1]. Hypertension was the most common risk factor (86%) but the majority (54.4%) of the patients had more than one risk factor [Table 2]. Headache and vertigo were the most common features accounting for 83.6% and 86.3%, respectively; however, none of the features in the study had significant association with the type of stroke as the P value was > 0.05 across all the clinical features [Table 3]. Thirty-eight (66.7%) patients had an ischemic stroke. Twenty-one (36.8%) patients were died.
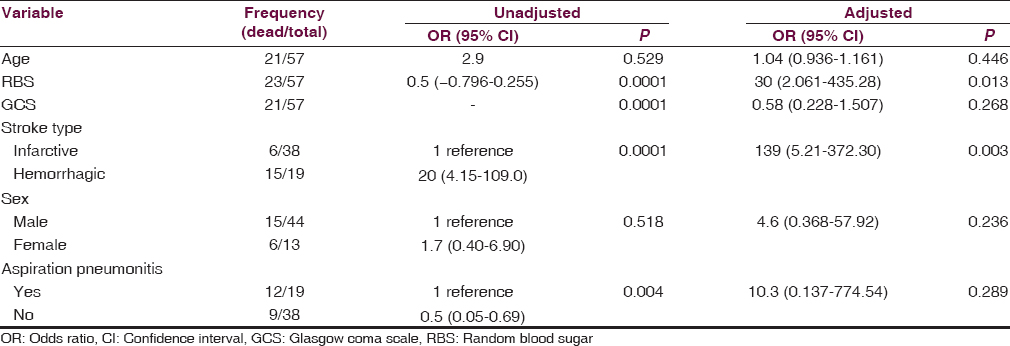
Factors associated with death in the patients were hyperglycemia, high GCS, hemorrhagic stroke, and aspiration pneumonitis [Table 4]. However, independent predictors of death in the study were hyperglycemia on admission and hemorrhagic stroke [Table 4].
Discussion
In the present study, the incidence of PCS was 9.6%. This figure was comparable with the report of Kora et al.[2] In their report, IPCS accounted for about 10% of the total stroke patients seen during the study period.[2] This figure was, however, lower than that reported by Jones et al. (17%)[5] and Macdonell et al. (14.8%).[1] The variations may be largely ascribed to differences in methodological approaches and to the fact that the focus of the current study was an infratentorial stroke.
The majority (67%) of the patients had an ischemic stroke. This finding, which was a reflection of the pattern of the type of stroke in the population studied,[67] is compatible with reports from elsewhere.[2] A study showed that out of the different anatomical sites involved in PCS, infratentorial ischemic stroke was the most common (63%).[28] However, a study in which only brain MRI was used for identification reported a relatively higher figure (70%).[28]
In the current study, mean age of the patients was 47.4 years. This figure, though similar to what is obtainable in other developing countries,[2] is lower than that reported in studies from the Western countries.[9] This disparity could be attributed to a higher incidence of stroke in the young adult in Northwestern Nigeria.[67]
In general, the risk factors for posterior circulation infarction do not differ from those for ACS. The present study showed that hypertension, diabetes mellitus, smoking, and hypercholesterolemia were the most common risk factors. This pattern is comparable to what was reported in studies by Ratnavalli et al.,[10] Kora et al.,[2] Caplan et al.,[11] and Sundar and Mehetre[8] The rarity of alcohol consumption, as a risk factor for IPCS, that was strikingly low when compared to the studies elsewhere[1245] probably reflects oddity of alcohol consumption in the predominantly Muslim community where the study was conducted.
Headache and vertigo were the clinical features mostly encountered in the patients. The clinical features are comparable to report elsewhere.[1213] These features are more frequently seen in PCS than in ACS.[14] The relatively low frequency of visual impairment observed in the current study was because of the fact that the current study focused on infratentorial stroke thereby excluding occipital and thalamic strokes. The organization of the brainstem relative to its vascular supply tends to lead to a number of well-recognized syndromes when occluded. Consequently, infarctive lesions in the territory supplied by posterior inferior cerebellar artery territory may result in the lateral medullary syndrome (Wallenberg's syndrome) that as exemplified by two of the patients in the current study, is characterized by ipsilateral facial sensory disturbances, nystagmus, dysphagia, dysarthria, contralateral dissociated hemi-sensory disturbances, and Horner's syndrome. It should be noted, however, that none of the clinical features observed in the patients in the current study could distinguish between ischemic or hemorrhagic stroke.
The 1-month hospital mortality rate recorded in this study was 36.8%. This figure was comparable to that (35%) reported by Jones et al., but it is higher than that reported by Sundar and Mehetre (17%),[8] Patrick et al. (25.6%),[15] and 4% in a Korean study.[16] The care of patients with stroke within the limited health budgets of most African countries offers a major and increasing challenge, therefore, the higher figure recorded in current study can be partly ascribed to delayed presentation, inadequate health infrastructure, nonexistent of stroke unit, and inadequacy of intensive unit.
Nonetheless, like in many hospital-based studies, the patients recruited during the study period may not be entirely representative of all stroke cases occurring in the community as those with severe stroke, such as primary brainstem and cerebellar hemorrhage would cause early death and hence, were less likely to have reached the hospital.
As reported in studies elsewhere,[1718] hyperglycemia, low GCS score, hemorrhagic stroke, and aspiration pneumonitis were found to be associated with 1-month mortality in our study, nevertheless, hemorrhagic stroke type and hyperglycemia emerged as independent predictors of death. This observation may be attributed to the fact that intraparenchymatous bleeding in the posterior fossa is usually a medical emergency, as pontine hemorrhages are lethal in 60–90% of cases, depending on the extent of hemorrhage and location.[121319]
Moreover, this finding, which was consistent with the reports from studies conducted on stroke in general,[121319] has significant implication for treatment in resource-poor setting. Identification of predictors of death is of paramount importance for clinicians, so that specific therapies and management strategies can be applied to patients at high-risk of dying.
It is noteworthy that none of the patients seen in the course of the study had thrombolytic therapy. Like other centers in Nigeria, thrombolytic therapy for infarctive stroke is not received in our center. One of the most important barriers to thrombolysis therapy in the developing world is a prehospital delay. The other factors militating against the use of thrombolytic therapy in developing countries includes financial constraints and lack of the necessary infrastructures. Therefore, until a cheaper thrombolytic agent and the proper infrastructure for utilization of thrombolytic therapy is available, in developing countries where such is not available, focusing on primary and secondary stroke prevention strategies will be potentially rewarding.[620]
In order to reduce the incidence, mortality, and morbidity associated with PCS, effort should be geared toward developing robust screening and control programs on hypertension. Furthermore, health education with an emphasis on control of other predisposing factors such as diabetes mellitus, avoidance of smoking and fatty foods, as well as regular exercise, should be embarked upon.
Apart from the earlier mentioned limitation encountered in the course of this study, the absence of magnetic resonance angiography for further localization of the vascular territory involved in the IPCS is also worthy of mention. Nonetheless, the data generated in this study have implications for clinicians and could serve as the basis for a large hospital- and community-based study in Nigeria.
Conclusion
Our study showed the occurrence of IPCS in a relatively younger age group. Headache and vertigo were the most common symptoms. Independent predictors of death in the study were hyperglycemia at presentation and hemorrhagic stroke subtype.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cerebellar infarction: natural history, prognosis, and pathology. Stroke. 1987;18:849-55.
- [Google Scholar]
- Clinical profile of posterior circulation stroke in a tertiary care center in Southern India. J Clin Diagn Res. 2011;5:217-21.
- [Google Scholar]
- Temporal profile (clinical course) of acute vertebrobasilar system cerebral infarction. Stroke. 1980;11:173-7.
- [Google Scholar]
- Stroke in developing countries: Experience at Kano, Northwestern Nigeria. Sudan J Med Sci. 2012;7:9-14.
- [Google Scholar]
- Stroke in young adults: a prospective study from northwestern Nigeria. ISRN Neurol 2012 2012:468706.
- [Google Scholar]
- Etiopathogenesis and predictors of in-hospital morbidity and mortality in posterior circulation strokes – A 2 year registry with concordant comparison with anterior circulation strokes. J Assoc Physicians India. 2007;55:846-50.
- [Google Scholar]
- Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ. 1980;58:113-30.
- [Google Scholar]
- Stroke in the posterior circulation territory – A clinical and radiological study. JAPI. 1995;43:910.
- [Google Scholar]
- New England medical center posterior circulation stroke registry II. vascular lesions. J Clin Neurol. 2005;1:31-49.
- [Google Scholar]
- The etiology of posterior circulation infarcts: a prospective study using magnetic resonance imaging and magnetic resonance angiography. Neurology. 1993;43:1528-33.
- [Google Scholar]
- Differences between anterior and posterior circulation stroke in TOAST. Cerebrovasc Dis. 2001;11:311-6.
- [Google Scholar]
- Temporal profile of vertebrobasilar territory infarction. Prognostic implications. Stroke. 1980;11:643-8.
- [Google Scholar]
- Posterior circulation ischemic stroke in Korean population. Eur J Neurol. 2006;13:742-8.
- [Google Scholar]
- Stroke or transient ischemic attacks with basilar artery stenosis or occlusion: clinical patterns and outcome. Arch Neurol. 2002;59:567-73.
- [Google Scholar]
- Multiple acute infarcts in the posterior circulation. J Neurol Neurosurg Psychiatry. 1996;60:289-96.
- [Google Scholar]
- Clinical profiles predictive of outcome in pontine hemorrhage. Neurology. 1997;49:1342-6.
- [Google Scholar]






