Translate this page into:
Impact on cognitive functions following gamma knife radiosurgery for cerebral arteriovenous malformations
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Radiosurgery is an alternative to surgical resection of arteriovenous malformation (AVM). Very few studies have addressed the concern of radiation injury to the brain and its attendant adverse effects on cognitive function.
Materials and Methods:
This prospective study included all patients who underwent gamma knife radiosurgery (GKRS) at our institute for cerebral AVM between 2006 and December 2008 (n = 34). All patients underwent neuropsychological evaluation before the procedure. Neuropsychological evaluation was repeated in eighteen patients 2 years following GKRS. Clinical outcome, AVM obliteration, and factors influencing outcome were analyzed in these eighteen patients.
Results:
Before GKRS, more than 50% had significant impairment of neuropsychological functions compared to normal population norms. 66.6% achieved the excellent radiosurgical outcome. At 2 years follow-up, patients showed varied improvement in neuropsychological function in various categories. Pretherapeutic median value for percentage perseverative responses was 26.5 and at follow-up, it reduced to 18.2 (P = 0.039). Set shifting improved in 11 patients (61.1%), remained same in 5 patients (27.7%), and deteriorated in two patients (11.1%). Patients with a higher Spetzler-Martin grade AVM demonstrated a significantly more favorable shift in follow-up test values for set shifting function (P = 0.021). Patients with postradiation imaging changes had lesser tendency to improve in neuropsychological performance at follow-up.
Conclusions:
GKRS has no clinically harmful effect on cognitive and neuropsychological functioning in patients with brain AVM. On the contrary, there is an improvement in majority of patients at 2 years following radiosurgery when nidus is obliterated.
Keywords
Arteriovenous malformation
cognitive effects
outcome
postradiation edema
radiosurgery
Introduction
With the advent of newer imaging modalities and their widespread availability, brain arteriovenous malformations (AVMs) are being increasingly diagnosed. Even though microsurgery is advocated as the definitive treatment modality, radiosurgery is commonly performed, as an alternative to surgical resection in many centers.[1] The AVM situated in and around the eloquent regions of the brain and those in the deeper regions of the brain are favored for radiosurgery.[2345] The principle of stereotactic radiosurgery is to accurately deliver a high dose of precise conformal radiation to an imaging-defined target in a single fraction. Nonetheless, the tissue adjacent to a radiosurgical target does receive a dose of radiation, albeit being a very small fraction of the total dose. Given the fact that majority of the patients with AVM are young, with long years of productive life ahead, the concern of radiation injury to the brain and its attendant adverse effects on cognitive function arise. Very few studies have addressed the issue of the possibility of cognitive dysfunction in patients who undergo radiosurgery.[678910] The present study evaluated a cohort of patients with brain AVMs prospectively and compared the pretherapeutic neuropsychological scores with 2 years posttreatment scores. To the best of our knowledge, this study represents one of the largest series where cognitive outcome after 2 years of patients with AVMs treated with gamma knife radiosurgery (GKRS) has been evaluated. Various factors affecting the changes in neuropsychological scores were analyzed.
Materials and Methods
Study design and patients
This prospective study included all the patients who underwent GKRS at our institute for AVM of the brain between 2006 and December 2008. The patients were followed up for 2 years. Inclusion criteria included the age range of 16–55 years. Only patients who were alert and amenable for neuropsychological evaluation were selected. Patients who had also undergone other modalities of treatment like embolization or surgery prior to GKRS were excluded.
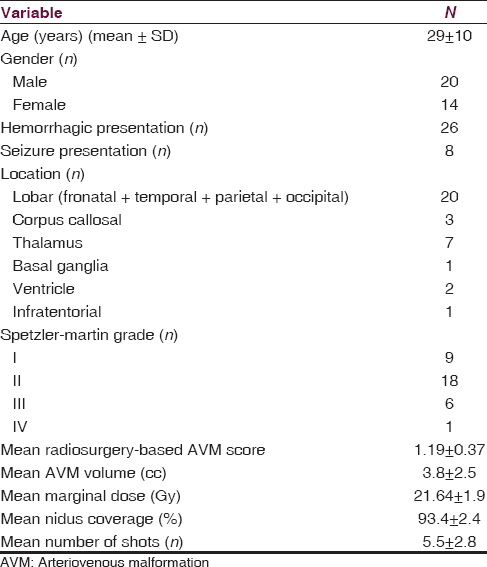
In the pretreatment period, neuropsychological evaluation was performed in 34 patients. A repeat neuropsychological evaluation 2 years following GKRS could be performed on 18 patients by the same examiner. We present in detail the comparative data of these 18 patients who were evaluated before GKRS and at 2 years follow-up period. The study was approved by the Ethics Committee of the Institute. Patient characteristics are given in Table 1.
Neuropsychological assessment
Neuropsychological evaluation was performed using NIMHANS Neuropsychology Battery,[11] with various tests as outlined in Table 2. All the tests were administered by a single examiner. The session for a patient ranged about 90–180 min for the completion of all tests.

Finger tapping tests and digit symbol substitution tests were used to assess motor speed and mental speed, respectively. Tests of attention included color trails test, digit vigilance test, and Triads test. Tests of executive functions included controlled oral word association test, animal names test, design fluency test, N-back tests (verbal and visual), the Tower of London test, Wisconsin card sorting test (WCST), and Stroop test. The first three of these tests evaluate fluency. The N-back tests were used to assess working memory. The Tower of London test was used to measure planning capability. WCST details concept formation and set shifting ability while Stroop test was used as an index of response inhibition. Auditory verbal learning test and Rey's complex Figure test were used to assess verbal and visual learning and memory respectively. A similar follow-up neuropsychological evaluation was performed after 2 years following GKRS.
Radiosurgery
Radiosurgery was performed with Leksell Gamma knife 4C system. In brief, patients underwent magnetic resonance imaging (MRI) of the brain and biplanar digital subtraction angiography (DSA) after fixation of Leksell stereotactic frame. Images were imported to GKRS planning system. A conformal GKRS plan with the prescription isodose, maximum dose, and dose to the margin was determined [Figure 1g]. Treatment details are given in Table 3. Follow-up consisted of a 6 monthly neurological examination and MRI of the brain. A DSA was performed after obliteration was diagnosed on MRI. Obliteration is defined as the complete absence of pathological vessels in the former nidus of the AVM, and the disappearance or normalization of afferent and efferent pathological vessels and a normal circulation time. Subtotal obliteration implies complete angiographic disappearance of the nidus, but the persistence of an early draining vein, as defined previously.[12]
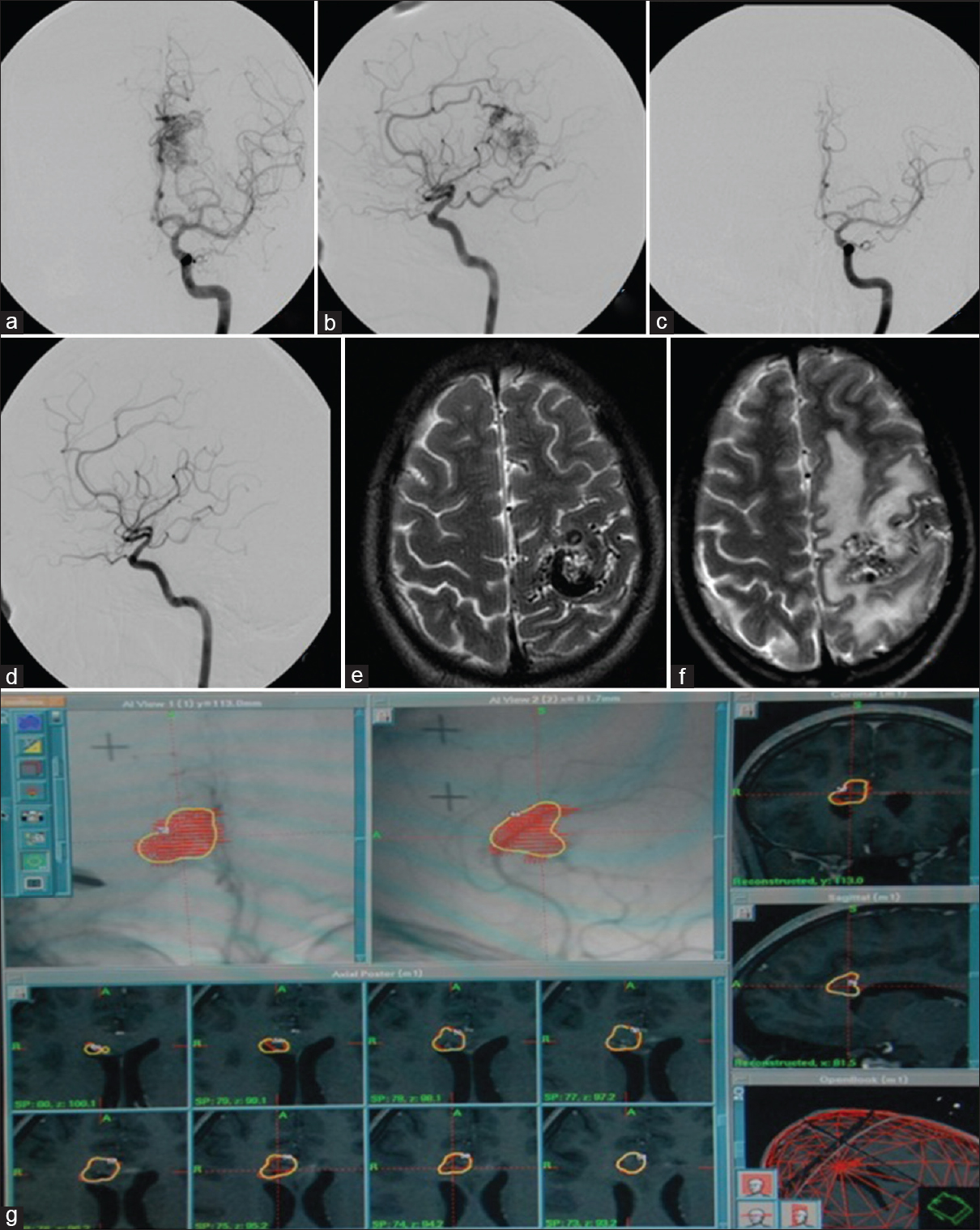
- (a and b) Left internal carotid angiogram demonstrating an arteriovenous malformation in the left splenial region being fed by the distal anterior cerebral artery and the posterior choroidal branches of the posterior cerebral artery. (c and d) Follow-up digital subtraction angiography after gamma knife radiosurgery shows complete obliteration of the arteriovenous malformation. (e) Magnetic resonance imaging brain T2 axial sequences show an arteriovenous malformation in the left precentral gyrus. (f) Magnetic resonance imaging brain T2 axial sequences following gamma knife radiosurgery showed partial obliteration of arteriovenous malformation with extensive hyperintensities suggestive of postradiosurgery imaging changes. (g) A screen shot of the gamma plan of a corpus callosal arteriovenous malformation being treated with gamma knife radiosurgery
Analysis
Initial data obtained after pretreatment evaluation were screened to look for general cognitive deficits seen in this patient group. The 2 years posttreatment test evaluation was compared with pretreatment data using Wilcoxon Signed Ranks Test. Nonparametric tests were applied because the data did not follow a normal distribution. Further factors influencing cognitive outcome were analyzed using Spearman's rho correlations. All statistical analysis was performed using Statistical Package for Social Sciences v. 15 (SPSS Inc., Chicago, IL, USA).
Results
Pretreatment neuropsychological evaluation
The present study noted that, out of the total patient cohort with AVM (n = 34), more than half had a significant deviation of neuropsychological functions from the normal population norms. The functions of attention, verbal learning, and memory and visual working memory were commonly affected. The present study noted that impairment in motor speed in 26.5% of patients, mental speed in 28.6%, focused attention in 36.7%, sustained attention in 58.3%, verbal fluency in 29.4%, response inhibition in 24.4%, visual working memory in 100%, and verbal working memory in 37.5% of patients. In verbal learning and memory, deficits were noted for verbal encoding in 56.2%, verbal retrieval in 56.2%, and verbal recognition in 72%. Impairment was noted in planning in 35.4% and set shifting in 21.9%.
Clinical and radiological outcome
Clinical and neuropsychological outcomes were evaluated for 18 patients and compared with pretreatment status. Complete angiographic obliteration could be achieved in 15 out of 18 patients. Three other patients had subtotal obliteration. Based on the criteria defined by Pollock and Flickinger[13] 12 patients (66.6%) achieved an excellent outcome, i.e. obliteration of nidus and no new deficits [Figure 1a-d]. Two patients had a good outcome (obliteration but a minor deficit). The outcome was fair in one patient (obliteration and a major deficit). In three patients with subtotal obliteration, the outcome was unchanged (residual AVM and no deficit). None of the patients had a poor outcome. All the patients were functionally independent. All except three could continue the previous occupation including those involved in skilled employment. Two patients required a change in the occupation because of hemiparesis. One other patient, who is a housewife who had transient hemiparesis, could resume light household activities.
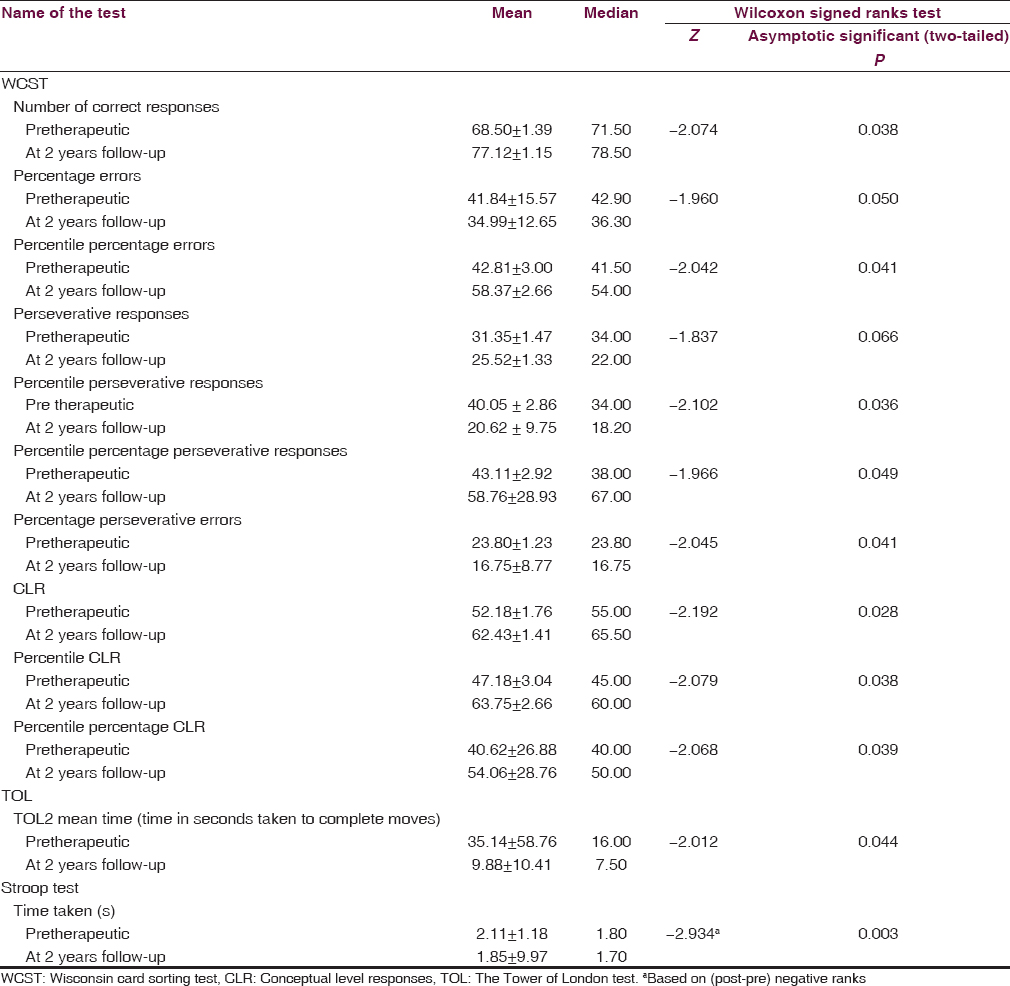
Neuropsychological outcome at follow-up
The neuropsychological outcome was compared in those 18 patients who had evaluation both preprocedure and at the 2 years follow-up. No global deterioration was noted in any of the patients. On the contrary, patients showed an improvement in neuropsychological function at various categories. Among them, the prominent statistically significant improvement was noted for set-shifting ability. Patients’ tendency for perseverance was found to be less at follow-up. Pretherapeutic median value for percentage perseverative responses was 26.5 and at follow-up, it reduced to 18.2 (P = 0.039). Set shifting improved in 11 patients (61.1%), remained same in 5 patients (27.7%), and deteriorated in two patients (11.1%). Other notable improvement was an increase in efficiency of planning in reduced time (tested by the Tower of London test). Patients took a median time of only 7.5 s as opposed to 16 s for successfully completing the 2 moves a section of the test (P = 0.044). Patients also showed improved ability for response inhibition at follow-up (P = 0.003). The tests in which patients showed improvement are tabulated in Table 3.
Factors affecting neuropsychological outcome
The factors which are likely to influence the neuropsychological improvement namely volume of AVM, location of the AVM in the brain, Spetzler-Martin grade, Radiosurgery based AVM score, and marginal dose were evaluated for their impact on the outcome. The effect of obliteration could not be analyzed because all AVMs showed some response at 2 years follow-up (15 patients showed total obliteration, and three had subtotal obliteration). Similarly, the presence of intracranial hematoma also could not be analyzed as only two out of 18 patients had nonhemorrhagic presentation. On analysis, only Spetzler-Martin grade showed a statistically significant correlation with the neuropsychological outcome. Interestingly, patients with a higher Spetzler-Martin grade AVM demonstrated a significantly more favorable shift in follow-up test values for set shifting function (P = 0.021). The location of AVM did not correlate with the neuropsychological outcome of the patients.
Postradiosurgery imaging changes and outcome
Post radiosurgery imaging changes have been defined as mild, moderate, and severe in previous studies.[1415] Five patients in the present series revealed imaging changes at various stages of follow-up [Figure 1e and f]. Three patients had mild changes; one had moderate PRI, and one had severe PRI. The mean duration for the appearance of PRI after treatment was 10.8 ± 5 months. On assessing individual patient's performance in relation to PRI severity, it was noted that patients with postradiation imaging changes had a lesser tendency to improve in neuropsychological performance in follow-up tests. Four out of five patients with PRI changes demonstrated some neuropyschological deterioration at follow-up evaluation. One patient with moderate PRI and two patients with mild PRI showed deteriorated conceptual responses at follow-up. One patient with severe PRI showed deteriorated set shifting function on follow-up evaluation.
Discussion
Majority of patients with cerebral AVMs become symptomatic in the second through fourth decades of life with the most common presentation being intracranial hemorrhage (50%). Seizures are the second most common presentation which occur in 25%, followed by a headache or focal deficits in 15%.[16] The management options for patients diagnosed with intracranial AVMs include microsurgical resection, stereotactic radiosurgery, and embolization of AVMs. Embolization is frequently performed in conjunction with either surgical resection or radiosurgery but is rarely curative by itself.
The adverse effects of conventional radiotherapy on cognitive functioning, when administered for cancer treatment, are addressed in many studies. A spectrum of late cognitive adverse effects can occur which include deficits in attention, working memory, learning ability, executive function in one end to incapacitating dementia in other end.[17] The effects are mediated by demyelination, microvascular injury, immunological response causing inflammatory reactions, atrophy of gray and white matter, altered neurotransmitter, and metabolites.[1819] However, the effects on cognitive functions following conformal focused radiosurgical methods are not well documented.
When radiosurgery is used to treat a benign condition like AVM, taking into the fact that majority are in their young and active phase of life, concerns arise about possible radiation injury to the brain with its attendant late clinical and cognitive complications. Of these complications, cognitive deficits may go underreported because they are not tested in detail in the routine clinical examination and are also rarely reported by patients. This prompted us to do a prospective systematic study to look for the neuropsychological outcome of patients who underwent GKRS for brain AVMs.
It is known that patients with brain AVMs have a significant reduction in cognitive abilities compared with expected levels.[682021] Wenz et al. noted on pretherapeutic evaluation that 24% of patients had deficits in intelligence, 34% in attention and 48% in memory testing.[9] Similarly, Blonder et al. in a group of 10 patients noted below normal performance in most of the tests performed.[8] On analyzing the pretreatment data of 34 patients in the present series, baseline scores showed significant reduction compared to the normal population norms in majority of tests. Main deviations were noted in domains of focused attention (by color trials in 36.7%), verbal memory (by Auditory verbal learning test in 31–72%), verbal and visual working memory (by N-back tests in 43.8% and 38.7%). All the patients who underwent GKRS did not have any preprocedural complaints of cognitive dysfunction and were declared to be normal on routine clinical examination. However, it was interesting to note that a majority of them had impaired cognitive dysfunction in one or more domains by formal neuropsychological assessment. This fact underscores the incidence of subclinical cognitive dysfunction secondary to the disease in patients with AVM, which often goes undetected.
On follow-up, it was interesting to note that a statistically significant improvement was noted in certain domains of the Tower of London test, WCST, Stroop's test. No global deterioration was noted in any patient in any of these tests. By definition, planning is the identification and organization of the steps and elements needed to carry out an intention or achieve a goal.[22] Planning ability is affected by frontal lobe lesions.[23] The results in the present study indicate that patients have taken significantly less time following treatment with GKRS to plan simple tasks, as compared to their pretreatment status [Table 3, the Tower of London tests]. Impaired performance on WCST is associated with Dorsolateral Prefrontal Cortex Impairment.[24] Post-GKRS assessment indicated that the patients have significantly improved in terms of ability to form concepts as well as ability to shift sets where required [Table 3, WCST]. All these functions are essential for a skillful employment. The fact that 89% patients could return successfully to previous employment correlated well with the follow-up neuropsychological outcome. The change in an occupation which was needed in two patients were due to motor deficits. Guo et al. had previously demonstrated that AVM patients improved significantly on WCST.[7]
On outcome analysis, only Spetzler-Martin grade showed a statistically significant correlation with the outcome. Interestingly, a higher Spetzler-Martin grade was correlated with a favorable shift with improvement in follow-up test values. The neuropsychological dysfunction in patients with AVM before GKRS, mostly subclinical, can be attributed to the following factors: Mass effect of AVM, hematoma due to AVM. It can also be due to focal ischemia of the surrounding brain parenchyma due to steal phenomenon. Cognitive dysfunction can also be partly due to the use of anti epileptic drugs (AEDs) in some patients as treatment of seizures. As evidenced in the present series, more than 50% of the patients with AVM demonstrated cognitive dysfunction due to one or more of the above reasons. Most of the patients in this series had bled before presentation which can significantly contribute to the cognitive dysfunction. It was interesting to note that a significant percentage improved in cognitive function, most probably due to the restoration of normal cerebral flow and reversal of ischemia to the surrounding brain. Higher the Spetzler-Martin grade or more complex the AVM, it is more likely that cognitive deficits are due to AVM per se and hence likely to show improvement at follow-up when they are obliterated. We noted that the volume, location of the AVM, Radiosurgery based AVM score, marginal dose, the presence of postradiation imaging (PRI) changes were not found to influence the cognitive outcome.
Postradiosurgery imaging changes (PRI) is defined as development of new regions of T2 imaging changes on postradiosurgery follow-up MRI scans irrespective of the presence of associated symptoms. It may represent radiation necrosis, regional ischemia or gliosis. It is classified as mild when there is a perilesional rim of signal intensity changes, moderate when it is more than mild but less than one-fourth of the hemisphere is involved, severe when more than one-fourth of the hemisphere is involved. Severity of PRI has been correlated with permanent symptomatic neurological deficits.[15] However, the effect of these imaging changes in cognitive functions and correlation with the severity of neuropsychological deficits have not been evaluated previously. In the present study, five patients had PRI changes (three with mild changes, one had moderate PRI, and one had severe PRI). On observing individual patient's performance, it was noted that patients with PRI changes demonstrated deterioration in performance in follow-up tests. Though no statistical significance could be demonstrated in view of very small numbers, it was interesting to note that 4/5 patients with PRI revealed worsening of cognitive function, while most of the other patients indeed demonstrated improvement in cognition following GKRS, raising the possibility that the occurrence and severity of PRI probably can affect cognitive outcome at follow-up.
Overall, neuropsychological assessment indicates improvement on time taken to plan simple tasks, the formation of concepts, set shifting and response inhibition (Stroop test) in the post- GKRS evaluation. Improvement may be due to normalization of perilesional perfusion disturbances and reduction in steal phenomenon with the obliteration of nidus. Overall enhanced neuronal plasticity along with the aforementioned changes might also have helped in the recovery of functions. Since the tests are repeated only after 2 years, a possibility of practice effect accounting for apparent improvement is nullified.
Conclusions
Radiosurgery has no clinically harmful effect on cognitive and neuropsychological functioning in patients with brain AVMs. On the contrary, there is an improvement in majority of the patients at 2 years following radiosurgery when the nidus is obliterated. Functions in which significant improvement noted are the time taken to plan tasks, ability to form concepts, as well as ability to shift sets where required and in response inhibition. It is likely that that patients treated for AVM with GKRS demonstrate improvement in neuropsychological functions unless they have radiation-induced changes Effect of postradiation imaging changes on cognitive functions require further studies and such studies may have implications in calculating radiation dose for a volume, especially in repeat radiosurgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- AHA scientific statement: Recommendations for the management of intracranial arteriovenous malformations: A statement for healthcare professionals from a special writing group of the Stroke Council, American Stroke Association. Stroke. 2001;32:1458-71.
- [Google Scholar]
- Radiosurgery for arteriovenous malformations of the basal ganglia, thalamus, and brainstem. J Neurosurg. 2004;100:210-4.
- [Google Scholar]
- Radiosurgical treatment for rolandic arteriovenous malformations. J Neurosurg. 2006;105:689-97.
- [Google Scholar]
- Results of radiosurgery for brain stem arteriovenous malformations. J Neurol Neurosurg Psychiatry. 2000;68:563-70.
- [Google Scholar]
- Cognitive function in patients with cerebral arteriovenous malformations after radiosurgery: Prospective long-term follow-up. Int J Radiat Oncol Biol Phys. 2002;54:1430-7.
- [Google Scholar]
- The impact of arteriovenous malformation radiosurgery on the brain: From morphology and perfusion to neurocognition. Stereotact Funct Neurosurg. 2006;84:162-9.
- [Google Scholar]
- Short-term neuropsychological outcome following Gamma knife radiosurgery for arteriovenous malformations: A preliminary report. Appl Neuropsychol. 1999;6:181-6.
- [Google Scholar]
- Assessment of neuropsychological changes in patients with arteriovenous malformation (AVM) after radiosurgery. Int J Radiat Oncol Biol Phys. 1998;42:995-9.
- [Google Scholar]
- Radiosurgery for cerebral AVMs in children and adolescents: The neurobehavioral outcome. J Neurosurg. 1997;86:207-10.
- [Google Scholar]
- Subtotal obliteration of cerebral arteriovenous malformations after Gamma knife surgery. J Neurosurg. 2007;106:361-9.
- [Google Scholar]
- A proposed radiosurgery-based grading system for arteriovenous malformations. J Neurosurg. 2002;96:79-85.
- [Google Scholar]
- Gamma knife radiosurgery as a single treatment modality for large cerebral arteriovenous malformations. J Neurosurg. 2000;93(Suppl 3):113-9.
- [Google Scholar]
- Clinical and neuroimaging outcome of cerebral arteriovenous malformations after Gamma knife surgery: Analysis of the radiation injury rate depending on the arteriovenous malformation volume. J Neurosurg. 2008;109:191-8.
- [Google Scholar]
- Natural history, evaluation, and management of intracranial vascular malformations. Mayo Clin Proc. 2005;80:269-81.
- [Google Scholar]
- Brain irradiation: Effects on normal brain parenchyma and radiation injury. Neuroimaging Clin N Am. 2009;19:657-68.
- [Google Scholar]
- Cognitive effects of chemotherapy and/or cranial irradiation in adults. Strahlenther Onkol. 2005;181:141-56.
- [Google Scholar]
- Mechanisms of radiation-induced brain toxicity and implications for future clinical trials. J Neurooncol. 2008;87:279-86.
- [Google Scholar]
- Prospective study of neuropsychological and psychosocial outcome following surgical excision of intracerebral arteriovenous malformations. J Clin Neurosci. 2003;10:42-7.
- [Google Scholar]
- Neuropsychological effects of brain arteriovenous malformations. Neuropsychol Rev. 2008;18:167-77.
- [Google Scholar]
- Adult clinical neuropsychology: Lessons from studies of the frontal lobes. Annu Rev Psychol. 2002;53:401-33.
- [Google Scholar]
- Wisconsin card sorting test performance as a measure of frontal lobe damage. J Clin Exp Neuropsychol. 1991;13:909-22.
- [Google Scholar]






