Translate this page into:
Anterior temporal lobe involvement: Useful magnetic resonance imaging sign to diagnose Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
We report a 32-year-old male who was admitted with speech disturbance. The patient presented to us with confusion, headache, and urinary incontinence. On examination, patient had no deficits except for aphasia. We proceeded with investigations. Magnetic resonance imaging (MRI) brain revealed extensive white matter ischemia and acute infarcts in both centrum semiovale regions. Fluid-attenuated inversion recovery (FLAIR) images showed anterior temporal lobe and external capsule involvement bilaterally [Figures 1 and 2]. Cerebrospinal fluid analysis done to rule out encephalitis was normal. After the investigations, we reviewed the history and found that the patient had recurrent episodes of migraine for several years, and his mother and maternal uncle had repeated episodes of the stroke leading to dementia. We suspected the inherited cause for stroke. We tested the blood for NOTCH 3 gene mutation. It was sequenced from exons 2, 3, 4, 5, and 6 and patient was found to be heterozygous for p.C144s mutation confirming the diagnosis of Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leucoencephalopathy (CADASIL).
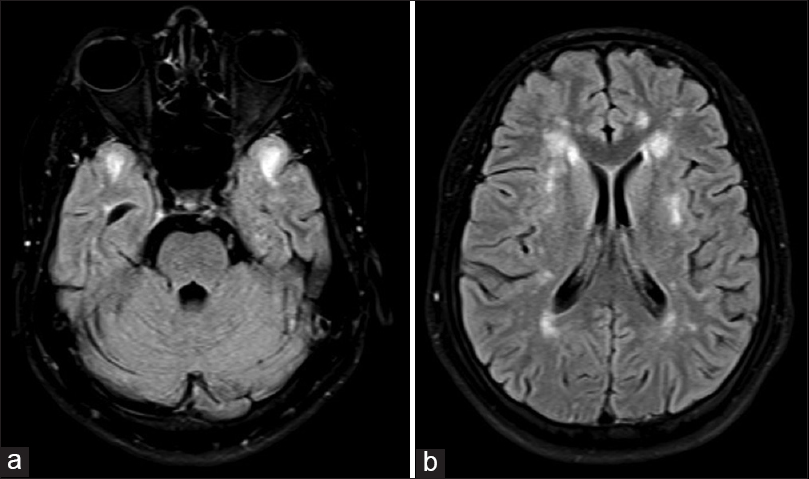
- (a) Magnetic resonance imaging brain axial fluid-attenuated inversion recovery image shows anterior temporal lobe involvement characteristic of Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy, (b) magnetic resonance imaging brain axial fluid-attenuated inversion recovery image shows external capsule involvement
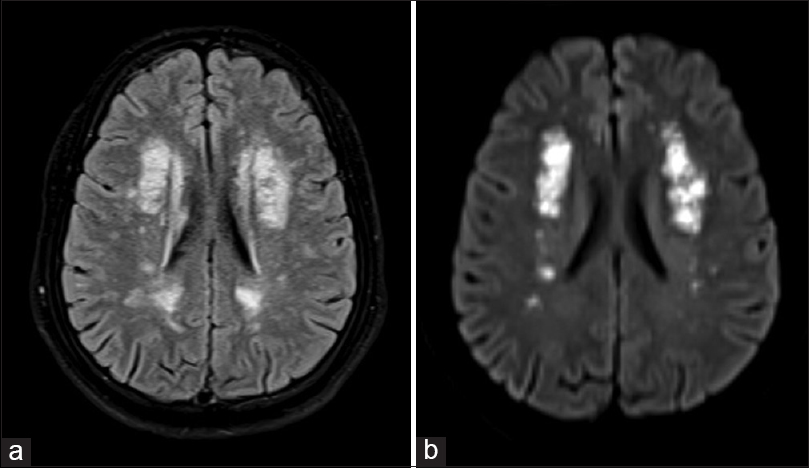
- (a) Magnetic resonance imaging brain axial fluid-attenuated inversion recovery image shows extensive periventricular white matter hyperintense signals, (b) magnetic resonance imaging brain axial diffusion weighted imaging image shows acute infarcts in both centrum semiovale regions
CADASIL is an acronym for Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy. CADASIL is a hereditary disease of small vessels predominantly affecting middle-aged individuals. It has been reported in nearly 500 families, but the actual prevalence is unknown.[1] The most frequent and earliest abnormalities are a hyperintense signal on T2-weighted/FLAIR appearing as punctiform lesions, in periventricular areas and in the centrum semiovale, which later become diffuse and symmetrical. Lacunar infarcts of basalganglia, thalamus, pons and cerebral microbleeds are also seen frequently.[2] Involvement of the anterior part of the temporal lobes and the external capsule is highly suggestive of CADASIL. According to Markus et al., anterior temporal lobe involvement has nearly 100% specificity as opposed to 45% specificity for external capsule involvement and both have sensitivity of around 90%.[3]
The gold standard for diagnosis of CADASIL is genetic analysis, but it is expensive and may be false negative if only a cluster of most probably affected exons is examined. MRI involvement of the anterior temporal lobes is a useful sign to suspect CADASIL in patients with an appropriate history and clinical findings. However, this could be false positive, and CADASIL is a diagnosis of exclusion in the absence of genetic testing.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical spectrum in CADASIL family with a new mutation. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2013;157:379-82.
- [Google Scholar]





