Translate this page into:
Impact of psychoeducation intervention module on parents of children with autism spectrum disorders: A preliminary study
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
Parents of children with autism spectrum disorders (ASD) in India face a host of challenges, while seeking care which ranges from unavailability of information to difficulty in availing services.
Aims:
To develop a psycho-education intervention module for parents of children with ASD and to study its impact on parent stress and knowledge.
Settings and Design:
Child Guidance Clinic Department of Psychiatry, Government Medical College and Hospital, Chandigarh. Interventional study.
Methodology:
Parents of children diagnosed with ASD as per Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criteria, recruited through consecutive sampling. Total number of 18 participants participated in the two phase study. Phase I included preparation of a parent training module through a four stage process and Phase II was evaluation of impact of the final version of the module on parental stress and knowledge.
Statistical Analysis:
Wilcoxon Signed-Rank test using SPSS version 17.0.
Results:
There was an improvement in all the domains of parenting stress and knowledge. Social stress score and total stress score showed significant improvement.
Conclusions:
Parent psycho-education intervention module on ASD decreases parenting stress, and improves knowledge about ASD. Psycho-education intervention module is a feasible and acceptable way of parent empowerment.
Keywords
Autism spectrum disorders
module
parent interventions
psycho-education
Introduction
Parents of children with autism spectrum disorder (ASD) experience stress and face challenges, while caring for their children in India. The reported stress is related to low awareness about the disorder, inadequate provisions for services, and difficulty in accessing them.[1]
Intensive behavioral and structured educational interventions remain the mainstay of ASD management. Their availability is limited to few apex centers in India which limit access and utilization with obvious adverse impact on follow-up rates and limitations in outcomes.[2]
Parents are important collaborators in planning for and implementing interventions for ASD. Training of parents as a therapist has been known to decrease parental stress[34] and improve child intelligence quotient (IQ), adaptive behavior, language, and socialization-communication.[5678] Evidence base of the effectiveness of parent mediated interventions in the well-educated and resourceful community has been established resulting in recommendations of their involvement.[9] Recent randomized controlled trials in resource-poor community settings have reported positive outcomes.[10] In India, parent-mediated behavioral interventions has shown encouraging results in a resource-poor setting.[11]
To strengthen support to parents seeking care for their children with ASD and to devise intervention plan sensitive to their needs it was envisaged to prepare a module incorporating elements of psycho-education and home-based interventions. The study was aimed at:
-
Development of a parent psycho-education intervention module for ASD
-
Measuring the impact of the module on parental stress and knowledge on ASD.
Methodology
Study participants
Parents of children diagnosed with ASD, recruited through consecutive sampling, from September 2011 to March 2012 in Child Guidance Clinic of Government Medical College and Hospital Chandigarh. Diagnosis was made by as per Diagnostic and Statistical Manual of Mental Disorders, 4th Edition[12] after parent and child interviews and play observation of children by trained psychiatrists and psychologists. Children with comorbid neurological disorders were excluded. Both parents of 6 children, fathers of 4 children and mothers of two gave consent and participated in the study. A total of 18 parents of 12 children meeting the inclusion criteria were enrolled.
Study design
Qualitative and quantitative methods were used for the two objectives. Nominal group technique was used to identify the felt needs of parents of children with ASD. Based on these needs and recommendations of expert team psycho-education intervention module was prepared through four staged process. The module was administered and impact on parent stress and knowledge was then evaluated.
Study procedure
A training module was developed by involving all the stakeholders including experienced psychiatrists, psychologists, special educators, social workers, and parents of children with ASD. The process involved free-listing of felt needs of parents which were then converged to a list of common needs. Keeping the felt needs of parents in view the module was prepared by experts based on available scientific literatureand incorporating suggestions from parents.
The module was then presented to the parents group in 12 parts, each session lasting about 2 h at a fortnightly interval. Impact of this module on parent stress and knowledge was then assessed using structured questionnaire.
Phase I: Development of module
Step 1: Identification of content areas for the module: We conducted semi-structured interviews with parents to identify their needs: Perceived problems of child; knowledge about diagnosis, symptoms, course, prognosis, and available treatment and expectations from health care providers. Nominal group technique was then employed to prioritize the parents’ concerns and reach a consensus. This is a small group structured technique which is carried out to obtain multiple inputs from several people on a particular problem. This method provides equal opportunity for participation to each participant and is based on voting resulting in preparation of a prioritized list of solutions. This method was chosen to ascertain maximum diversity of opinions and to incorporate the items with consensus.[13]
Total number of needs voiced by the parents was 51, which included perceived problem areas of the child: Inability of the child to speak, difficulty in making the child understand abstract concepts, difficulty in understanding the emotions and motives of behavior of the child, over familiar behavior with unknown people; inability to behave appropriately in parties, difficulty in managing behavior in shops, repetitive movements of fingers, and rocking movements of body. Queries like: “What are the causes of autism,” “are there any blood tests or brain scans which diagnose autism,” whether “cure” was possible, did “it” run in families, can they prevent “it,” would their second child also suffer from autism, can they plan for another baby, would their child grow into a “normal adult” in the future, and “what they can do to bring improvement in their child” pointed toward the need for general information about ASD.
Step 2: Needs with similar concepts were merged, irrelevant needs eliminated. The needs were categorized into different domains pertaining to ASD: General information about ASD, intervention for socialization, communication, behavioral problems, and sensory difficulties of the child. A draft module was prepared based on domains of needs [Figure 1]:

- Steps of nominal group technique
-
The general information chapter was prepared which included meaning/definition of ASD, various forms in which ASD presents, early symptoms, prevalence, causes, course, diagnosis, prognosis, and some frequently asked questions regarding these. It also included information on concomitant medical and psychiatric disorders
-
Home- based interventions were incorporated in the draft module that can be taught to parents which can be used during daily routine and activities at home
-
Section on social interaction and communication: A brief description of the types of deficits in social interaction and communication, followed by the four core skill areas identified: Social engagement, language, social imitation, and play were described. Interactive teaching techniques for parents to develop the capacity of the child to engage were mentioned based on project impact which is an evidence-based intervention[8]
-
Section on Behavioral problems: Behavioral problems like tantrums, aggression, self-stimulation, and self-injury were described and principles of behavior therapy stated. Use of principles of behavior therapy to develop desired behaviors and reduce the undesired behaviors was demonstrated.[14]
-
Step 3: A half-day workshop was held during which the various stakeholders were presented with the prefinal version of the module. The 15 member team was divided into three groups to work independently on separate sections of the module: Socialization, communication, and behavioral problems. After discussion in small groups, these interventions were discussed with the members of the whole group collectively and specific home based interventions finalized:
Socialization and communication
Interventions like animation, imitation, and play were suggested which can be used to improve core skills of socialization [Table 1].

Communicative temptations which encourage a child to communicate were mentioned [Table 2].
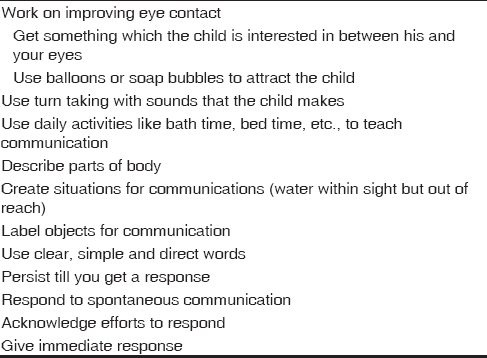
Techniques for improving the language by modeling and expanding language were elaborated [Table 3].

Behavioral problems
Steps of behavioral analysis were enumerated:
-
Defining behavior: How to identify and define problem behavior to be targeted for intervention; target behavior should be something which would improve a child's functioning
-
Measuring behavior: Antecedent, behavior, consequences charting of the target behavior for a predetermined period. Antecedents are the circumstances which predetermine the behavior, whereas consequences are something that happens afterward. Measuring the frequency and duration of the target behavior was explained
-
Keeping data: For monitoring the child's progress, simple measures like noting down a tick for correct and a cross for incorrect on a simple table was demonstrated
-
Types of reinforcements and their effective delivery were elaborated. How to carry out a functional assessment of problem behavior was also described, and use of natural reinforcers was emphasized.
Sensory issues like hyposensitivity and hypersensitivity were described and simple and feasible measures suggested.
Prefinal version of the module was developed in English and later translated into Hindi.
Step 4: Final version was developed after incorporation of parent suggestions. The prefinal version of the module was administered in group sessions to parents: The 1st h was spent on reading out the chapter of the module and description of the techniques, and the 2nd h was devoted to parents’ clarifications and suggestions. Parents were provided with a copy of that section of the module and were asked to carry out the suggested interventions at home. The subsequent session was used to incorporate the suggestions of the parents based on their experiences of application of the interventions. Suggestions from parents on comprehensibility of the module were incorporated in the final version.
Phase II Impact of the module on parents: The intervention module was administered to eligible participants in a group size of six on a fortnightly basis, each session lasting about 2 h. The session was moderated by a psychiatrist having expertise in group psychotherapy. The various parts of the module were presented to the participants: General information, socialization, and communication were given in three sessions each, behavioral problems were given in two sessions and sensory issues were addressed in one session. During the sessions, parents were encouraged to engage and interact with each other.
Study instruments
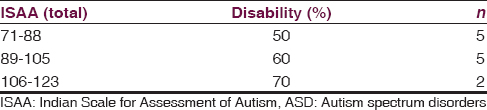
Indian Scale for Assessment of Autism (ISAA) was used for assessing the severity of autism. ISAA rates autism in six domains: Social relationship and reciprocity; emotional responsiveness; speech, language, and communication; behavior patterns; sensory aspects; and cognitive components. Items are rated from 1 to 5 and take about 15–20 min to administer.[15]
-
IQ of the children was measured using Gesell Drawing Test[16] and Vineland Social and Maturity Scale,[17] if the child was below 6 years of age. Malin's Intelligence Test for Indian children[18] and Raven's Colored Progressive Matrices Component of Raven's Educational Test,[19] were used in children above 6 years
-
Kuppuswamy socioeconomic scale was used to measure the socioeconomic status of families. The updated version of this scale has incorporated effects of inflation over monthly income ranges[20]
-
Family interview for stress and coping in mental retardation which was devised for assessment of stress and coping in families of children affected with intellectual disability was used for evaluating parent stress levels. It has four areas and 11 subscales rated on a five-point scale (no or minimal stress to very high-level stress). Authors of the scale report of face and content validity of the scale when used in parents of children with developmental disorders which justifies its use in the present study[21]
-
A pretested questionnaire consisting of six questions to quantify the knowledge of parents on various aspects of ASD like definition of autism, cause, presentation, course, prognosis, and treatment of ASD, was utilized and administered before and after presentation of module.
Statistical analysis
Data were double checked and entered into MS excel. Descriptive statistics were used and Wilcoxon Signed-Rank test was done to analyze the change in stress and knowledge improvement of parents following administration of module using SPSS version 17.0.
The study received approval from the Institutional Ethics Committee.
Results
All the children were males; their mean age was 5.92 years (range: 3–12 years). Ten were diagnosed with mild autism (70–106) whereas two had moderate autism (107–153) as per ISAA [Table 4]. Two of the children had mild mental retardation (IQ = 53, 67), one had dull average intelligence (IQ = 88). Two of them had received formal education for 6 and 8 years. Others were attending play-groups or kindergarten.
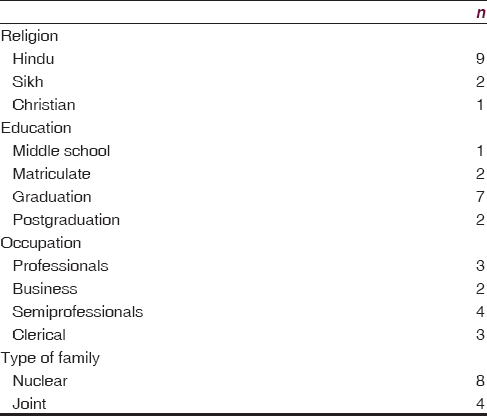
All parents belonged to middle socioeconomic status. The majority were Hindu and lived in nuclear families [Table 5]. The average family size was four (range: 3–8).
Stress was perceived in the domains of daily care by all the families. Parents reported feeling distressed due to extra care needed by children affected by ASD which put a strain on their leisure time. Emotional stress was also felt by all the families in the areas of interpersonal functioning and social relationships. Only four families reported distress in the social domain. The families reported feeling embarrassed in social gatherings due to their child who was perceived as “abnormal.” Only one family reported facing financial troubles. Administration of module reduced total stress and social stress scores reaching statistical significance [Table 6].

Scores of knowledge significantly improved after administration of the module with the median value of 26 before and 50 after administration of the module (P = 0.005) [Table 6].
Discussion
Psycho-education intervention module can be considered as a small step toward empowering Indian parents of children with ASD. The module being in a bilingual form (Hindi + English) would be useful for a large part of North India. The module has incorporated psycho-education and intervention training; both identified as important ingredients of caregiver training in ASD.[2223] The psychoeducation part has addressed the need for information, while the home-based intervention part has suggested interventions for varying needs of children.
Children spend a lot of time with their parents and are in most proximate contact with them, the involvement of parents in therapeutic interventions provides an opportunity for better acquisition and generalization of skills. Parents report feeling more at ease while using these interventions at home, as a naturalistic form of intervention is considered easier to fit into the existing family routine.[22] The elements of parent involvement in terms of duration, intensity, and content of intervention remain varied. While research is still establishing the critical elements of effectiveness of interventions for ASD, to ensure better outcome intervention plans should be sensitive to local needs and problems.
The concern of impairment in socialization voiced by parents is consistent with literature which suggests that Indian parents are more concerned about difficulties in socialization as compared to developmental difficulties which are more worrisome to western parents which can be explained by more emphasis on individualism and personal performance by western society.[22]
Parents of children with ASD face severe stress which is more than any other developmental disability owing to the uncertainty of diagnosis and prognosis.[23] Parental stress levels have been documented to be reduced when they are included in an in-home training of interventions.[42425] Improving the levels of parents’ knowledge about autism and teaching strategies to manage problem behaviors of their child is known to decrease parental stress. Our module improved parental knowledge about ASD and reduced their perceived stress levels.
The group sessions were enthusiastically attended by the parents, at least one of the parents would manage to attend the group session. During the discussions, parents provided suggestions to each other regarding utilization of home-based interventions. The process of preparation of the module has made possible to have a group of parents of children with ASD in Chandigarh which meets at regular intervals and provides support to each other through many informal ways which is gradually paving the way for a formal ASD parent group. The parental acceptability of the module demonstrates its usefulness as an adjunct to any ongoing intervention services for ASD. This module can be further modified as per region specific need and can be implemented as an integral part of service delivery.
Limitations
This is a preliminary study to see the acceptability of the module and its impact on parent knowledge and stress; hence, the effect on children cannot be commented on. The small sample size and narrow range of severity of ASD in the included group may limit generalization.
Conclusions
Parent psychoeducation intervention module developed in the present study addressed the parental need for information, lowered parental stress, and is acceptable to parents of children with ASD.
Financial support and sponsorship
Department of Science and Technology, Chandigarh Administration.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The study was supported by research grant from Department of Science and Technology, Chandigarh Administration.
References
- Challenges, coping strategies, and unmet needs of families with a child with autism spectrum disorder in Goa, India. Autism Res. 2012;5:190-200.
- [Google Scholar]
- High treatment drop-out rate of children with pervasive developmental disorders. Hong Kong J Psychiatry. 2004;14:10-5.
- [Google Scholar]
- Early intensive behavioral intervention for children with autism: Parental therapeutic self-efficacy. Res Dev Disabil. 2002;23:332-41.
- [Google Scholar]
- A randomized, controlled trial of a home-based intervention program for children with autism and developmental delay. J Dev Behav Pediatr. 2007;28:308-16.
- [Google Scholar]
- Research Units of Pediatric Psychopharmacology (RUPP) autism network randomized clinical trial of parent training and medication: One-year follow-up. J Am Acad Child Adolesc Psychiatry. 2012;51:1173-84.
- [Google Scholar]
- Parent inclusion in early intensive behavior interventions for young children with ASD: A synthesis of meta-analyses from 2009 to 2011. Res Dev Disabil. 2013;34:2967-85.
- [Google Scholar]
- Medication and parent training in children with pervasive developmental disorders and serious behavior problems: Results from a randomized clinical trial. J Am Acad Child Adolesc Psychiatry. 2009;48:1143-54.
- [Google Scholar]
- Initial efficacy of project ImPACT: A parent-mediated social communication intervention for young children with ASD. J Autism Dev Disord. 2013;43:2943-52.
- [Google Scholar]
- Parent-mediated early intervention for young children with autism spectrum disorders (ASD) Cochrane Database Syst Rev. 2013;4:CD009774.
- [Google Scholar]
- Caregiver-mediated intervention for low-resourced preschoolers with autism: An RCT. Pediatrics. 2014;134:e72-9.
- [Google Scholar]
- Evaluation of a parent-based behavioral intervention program for children with autism in a low-resource setting. J Pediatr Neurosci. 2012;7:16-8.
- [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-Text Revision. (4th ed). Washington, DC: American Psychiatric Association; 2000.
- [Google Scholar]
- Building consensus in health care: A guide to using the nominal group technique. Br J Community Nurs. 2004;9:110-4.
- [Google Scholar]
- New strategies and findings for behavioral interventions in autism spectrum disorders. Ann N Y Acad Sci. 2013;1304:70-6.
- [Google Scholar]
- Use of Indian scale for assessment of autism in child guidance clinic: An experience. Indian J Psychol Med. 2011;33:217-9.
- [Google Scholar]
- Gessel's drawing test as a measure of intelligence in mentally retarded children. Indian J Ment Retard. 1972;5:64-8.
- [Google Scholar]
- Vineland Social Maturity Scale. Circle Pines, Minnesota: American Guidance Services Inc; 1965.
- [Google Scholar]
- Malin's Intelligence Scale for Indian Children. Nagpur: Child Guidance Centre; 1969.
- [Google Scholar]
- Kuppuswamy's socioeconomic scale: Updating income ranges for the year 2012. Indian J Public Health. 2012;56:103-4.
- [Google Scholar]
- Family interview for stress and coping in mental retardation (FISC-MR): A tool to study stress and coping in families of children with mental retardation. Indian J Psychiatry. 1999;41:341-9.
- [Google Scholar]
- Issues and theoretical constructs regarding parent education for autism spectrum disorders. J Autism Dev Disord. 2012;42:1218-27.
- [Google Scholar]
- Psychosocial support for families of children with autism. Asia Pac Disabil Rehabil J. 2005;16:62-83.
- [Google Scholar]
- Parent training interventions for children with autism spectrum disorders. In: Matson JL, ed. Applied Behavior Analysis for Children with Autism Spectrum Disorders. New York: Springer; 2009. p. :237-57.
- [Google Scholar]
- Effects of a father-based in-home intervention on perceived stress and family dynamics in parents of children with autism. Am J Occup Ther. 2011;65:679-87.
- [Google Scholar]






