Translate this page into:
Neurocysticercosis: About 5 reported Thai cases
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Human cysticercosis occurs when an individual with taeniasis brings his unwashed hands to his mouth (self-infection) or by the ingestion of contaminated food, water, fruits, and vegetables from orchards and gardens fertilized or irrigated with material that have been contaminated with Taenia solium eggs (hetero-infection). The increase of migration, immigration, tourism, and globalization also strengthens this dissemination. Neurocysticercosis (NCC) is globally spreading because infection of the taeniasis/cysticercosis complex is becoming widely endemic, particularly in the rural areas of Central and South America, Asia, and Africa.[1] In accordance with the criteria of the World Health Organization, endemic regions for the taeniasis/cysticercosis complex are those regions where the contamination rate of the population is above 1% for taeniasis, 0.1% for human cysticercosis, and 5% for animal cysticercosis. In Asia, the endemic countries are China, Taiwan, India, Vietnam, Myanmar, Nepal, and the numerous islands of Indonesia. However, it is less common in Thailand, South Korea, Philippines, Malaysia, and Bangladesh.
Because of the communication difficulties arising from language and the wide discrepancies in the availability of laboratory resources, data on NCC incidence continue to be underestimated. The need to diagnose NCC, the knowledge of its epidemiology, and the natural evolution of the disease is often the only element available to most neurologists in developing countries.
In general, NCC is more frequent (51–80%) among males; however, female predominance (53–75%) has been observed, particularly in more severe manifestations.[2] Deaths due to NCC range from 4.8 to 25.9% patients with NCC and in neurosurgery patients, this rate is 0–60%.[2]
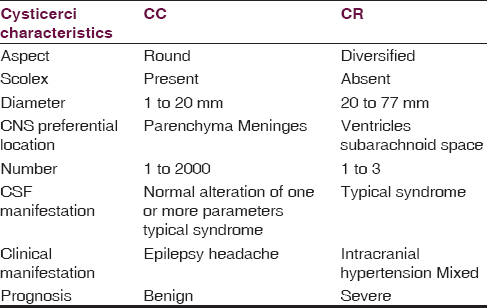
In the central nervous system, the cysticerci are fundamentally present in two forms [Table 1]: The simple larval form (Cysticercus cellulosae = CC) and racemose cysts (Cysticercus racemosus = CR).[3] The CC presentation is more frequent and usually associated with the benign clinical or asymptomatic form and can be located anywhere in the brain. The CR, represented by cysts or multiloculated clusters that resemble “bunches of grapes,” and is responsible for the most severe clinical forms. It is located in the cerebrospinal fluid (CSF) space, where it can develop. Studies suggest the existence of two other forms of cysticerci that are infrequent and rarely used in the denomination: The acephalic (multilobulated) and intermediate (large cyst with scolex) forms.[4] The unique CR form occurs in 4–25% of cases.[2]
One significant characteristic of NCC is the lack of a typical syndrome as we can see in Wiwanitkit and Wiwanitkit summary.[5] May be asymptomatic, symptomatic or fatal; have an acute, sub-acute or chronic picture; or may be in remission or exacerbated. Moreover, neurological examinations are normal in 25–83% of patients.[2] Rare manifestations are described in the literature like Parkinson's syndrome always associated with the presence of CC and not to the CR, as reported by Wiwanitkit A and Wiwanitkit V[25] Asymptomatic form may be considered as a natural evolution of a clinical or sub-clinical manifestation, and its diagnosis may be an accidental laboratory or autopsy finding. All clinical manifestations of NCC can mimic other pathologies, mainly infectious and parasitic diseases, which complicate diagnosis. The CSF may be normal, even in patients with viable cysticerci. Computed tomography and magnetic resonance imaging have allowed noninvasive diagnoses but can lead to false negatives.
In an attempt to standardize the diagnostic criteria of the NCC, diagnostic criteria were initially proposed in 1996 and revised in 2001, based on objective clinical, imaging, immunological, and epidemiological data.[6]
Treatment is a highly controversial issue. Based on the great differences in clinical presentation, pathogenesis, natural history, and treatment options for the different forms of NCC, a consensus of recommendations has been established.[7] Two drugs are commonly used praziquantel and albendazole. The choice of anti-inflammatory drugs includes steroids and dextrochlorpheniramine. Surgical treatment is still very controversial. Surgical removal has been recommended in cases of intraventricular cysticercosis and intraparenchymatous solitary giant cysts, provided there is no pericystic inflammatory reaction. The neuroendoscopic resection is the recommended procedure for intraventricular and subarachnoid basal cisterns cysts.[8] In NCC, shunts have frequent obstructions and may require multiple revisions. The recommendation is that this surgery must be performed before the introduction of cysticidal treatment.
The progression of NCC may be simple or complicated, have remission with or without treatment, and may exhibit symptoms that can disappear for long periods of time or persist until death. In other words, NCC may be asymptomatic, symptomatic or fatal; have an acute, sub-acute or chronic picture, or may be in remission or exacerbated.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Control of Taenia solium taeniasis/cysticercosis: From research towards implementation. Int J Parasitol. 2005;35:1221-32.
- [Google Scholar]
- Neurocysticercosis: The enigmatic disease. Cent Nerv Syst Agents Med Chem. 2011;11:261-84.
- [Google Scholar]
- Morphological evidence indicating that C. cellulosae and C. racemosus are larval stages of Taenia solium. Arch Invest Med (Mex). 1985;16:81-92.
- [Google Scholar]
- Molecular determination of the origin of acephalic cysticercus. Parasitology. 2005;130:239-46.
- [Google Scholar]
- Racemose cysticercosis: A summary of 5 reported Thai cases. J Neurosci Rural Pract. 2015;6:451.
- [Google Scholar]
- Current consensus guidelines for treatment of neurocysticercosis. Clin Microbiol Rev. 2002;15:747-56.
- [Google Scholar]
- Intraventricular and subarachnoid basal cisterns neurocysticercosis: A comparative study between traditional treatment versus neuroendoscopic surgery. Childs Nerv Syst. 2009;25:1467-75.
- [Google Scholar]





