Translate this page into:
Myoarchitectonic advancement of the C2 spinous process for C1-C2 posterior fusion: A novel technique
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Study Design:
Retrospective descriptive study of an innovative surgical technique.
Objective:
To assess the feasibility of using a large C2 spinous process as a vascularized bone graft donor with muscles attached to it in C1-C2 posterior fusion with evaluation of post operative fusion and pain in these cases.
Summary of Background Data:
C1-C2 posterior fusion essentially requires a bone graft and for this a separate incision is needed at the donor site with its associated morbidity. The procedure also entails detachment of muscles attached to the C2 spinous process. Due to the detachment of these muscles with important functions, postoperative nuchal pain is common in these patients. We developed a novel technique of harvesting the vascularized C2 spinous process as a bone graft to minimize the above-mentioned complications.
Materials and Methods:
Five patients with atlanto-axial dislocation due to various pathologies underwent C1-C2 posterior arthrodesis with the present technique. They were followed up for 6 to 18 months and were evaluated for feasibility of procedure, post operative fusion and post operative complications, especially pain.
Results:
The procedure was accomplished successfully in all patients without any perioperative complications. All patients were pain free 3 months after surgery—mean Visual Analogue Scale (VAS) was 0.4. Fusion (confirmed by plain radiography in three and by CT scan in two patients) was achieved in all five patients (100%).
Conclusion:
Myoarchitectonic advancement of C2 spinous process is a novel technique of C1-C2 posterior fusion in which a local vascularized bone graft is used avoiding donor site morbidity and at the same time preservation of dynamic function of muscles attached reduces the post operative pain.
Keywords
Atlanto-axial
bone graft
C1-C2 posterior fusion
CV junction
myoarchitectonic
Introduction
Atlanto-axial arthrodesis is indicated in atlanto-axial instabilities of different etiologies whether congenital, traumatic, inflammatory, infective or degenerative. Posterior C1-C2 arthrodesis has essentially two components–fixation and fusion. For fixation we are dependent on wires, screws and rods in various combinations as described in well-established techniques (Goel’s, Harm’s).[12] For fusion, in all the above-mentioned techniques, bone graft is needed which could be autologous graft, allogenic graft or artificial bone substitute.
Use of autologous bone graft from iliac crest bone for fusion is a common and accepted technique. However, harvesting of this bone graft is not risk free and both major and minor complications have been reported.[34567] The spinous process of the axis vertebra is a bulky, strong bone with both cancelous and spongious components. More than posterior two thirds of it can be utilized as a strong graft. Also, part of the vascularity of the spinous process comes from the muscles attached to it, so harvesting an osteoplastic C2 spinous process graft is technically possible.
The strong semispinalis cervicis muscle attached to the C2 spinous process serves important functions of extension and rotation. Only 58% rotation take place at the C1-C2 joint and rest at the subaxial spine, while extension mainly occurs at the C0-C1 joint.[8] Hence, detachment of semispinalis cervicis from its most strong and bulky insertion to the C2 spinous process will lead to dysfunction in rotation and extension which is still required at subaxial cervical spine. This detachment will possibly also lead to post operative neck pain.
We describe a novel technique of C1-C2 posterior fusion that we performed in five patients [Table 1], where the spinous process of C2 was used as a bone graft donor. The semispinalis cervicis muscles are kept attached to the advanced C2 spinous process so that the myoarchitecture of the neck region is preserved to the maximum. Since the attachment of the muscle is preserved and its dissection is avoided, this technique may lead to less post postoperative pain and preservation of part of muscle function.[9]
Materials and Methods
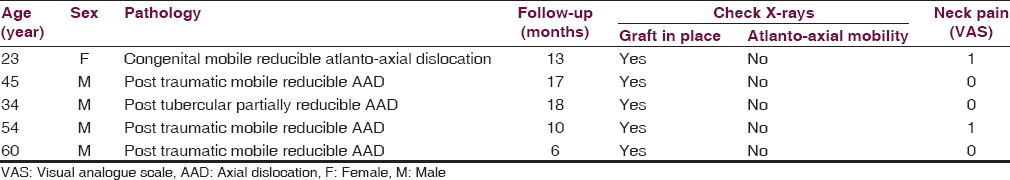
Five consecutive patients with C1-C2 instability were treated from September 2011 to 2013 [Table 1]. The male to female ratio was 4:1 with age group ranging from 23 to 60 years (mean age 43.2 years). Only patients with C1-C2 reducible axial dislocations with no component of rotational instability were considered for treatment with above technique. The instability was confirmed on plain radiography [Figure 1] (lateral flexion, extension view, anteroposterior and open mouth view). Also, CT scan of CV junction was performed to look for any additional deformity. MRI was performed to look for neural compression.
- X-ray lateral view flexion and extension of the patient with post tubercular atlanto-axial dislocation
Operative technique
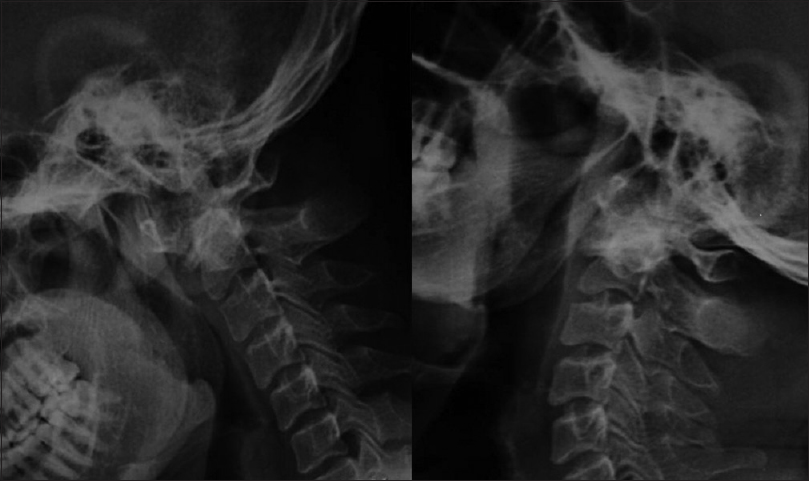
After oral intubation and general anesthesia, the patients were positioned in a prone position on bolsters and were well padded at the pressure points with head resting on the horseshoe head rest. A midline incision to achieve adequate exposure from the suboccipital region to the C3 spine is then made. After the skin, subcutaneous tissue, fascia and ligamentum nuchae are incised, part of subocciput, C1 posterior tubercle, posterior ends of the C2 spinous process and C3 spinous process were exposed. Muscles were not detached from the C2 spinous process. The strong and bulky attachment of semispinalis cervicis to the C2 spinous process was identified and hooked in slings bilaterally [Figure 2]; however, C2 lamina was cleared of soft tissues paramedially.
- Intraoperative picture of the C2 spinous process (marked in asterisk) dissection with attached semispinalis cervicis hooked in slings (arrows). Patient in a prone position; midline skin incision
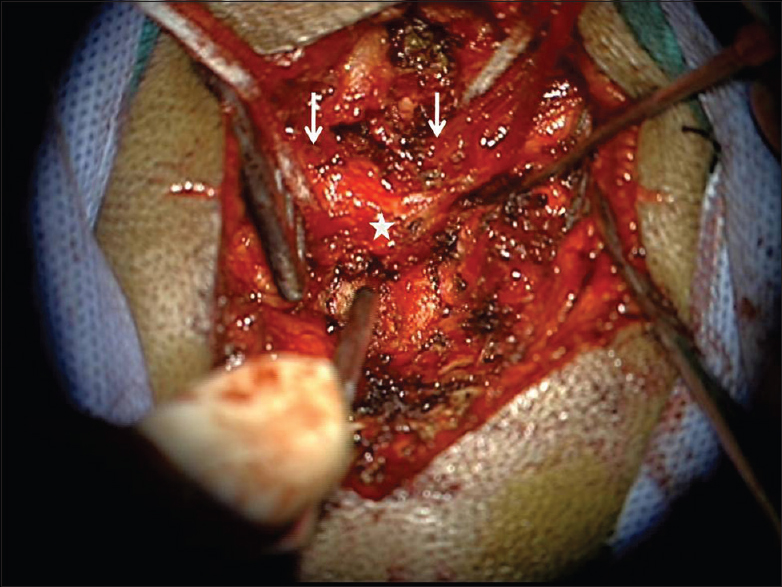
Then under fluoroscopic guidance, using a right-angled spine cutter or bone saw, the posterior 3/4th of the C2 spinous process was cut from the lamina from the superior to inferior direction [Figure 3]. Now the detached C2 spinous process is displaced caudally to create room for further steps.
- Intraoperative picture of posterior 3/4th of the C2 spinous process (in asterisk) after being cut with the attached muscles hooked in slings. Patient in a prone position; midline skin incision
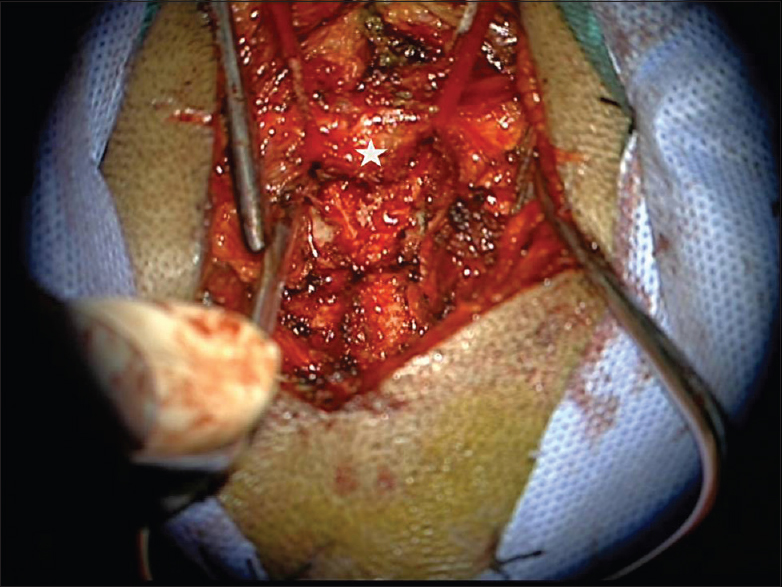
Sublaminar C1-C2 cables (Atlas Cable, Medtronic Sofamer Danek, Memphis, TN, USA) were passed and the C1-C2 reduction was achieved which was confirmed by using C-arm. Posterior and inferior surface of C1 posterior arch along with superior surface of C2 lamina were then decorticated using the high speed drill. The wire is then passed through the posterior part of the detached bone graft so that on crimping it gets snugly jammed in the C1-C2 interval. The C2 spinous process with semispinalis cervicis attached was then advanced superiorly and anteriorly to wedge it into the C1 and C2 interlaminar space. The cables were then tightened in crisscross fashion to keep the graft in place after crimping of the cables which was again confirmed on fluoroscopy [Figures 4 and 5]. The retractors were removed; fascia and skin were closed using standard techniques.
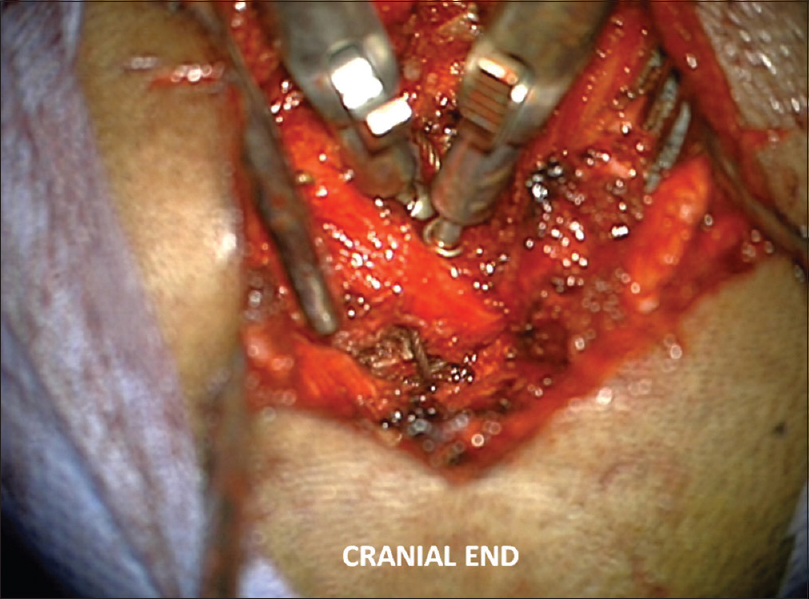
- Intraoperative picture showing advanced C2 with attached muscles wedged in place using sublaminar polybraided titanium cables. Patient in prone position; midline skin incision
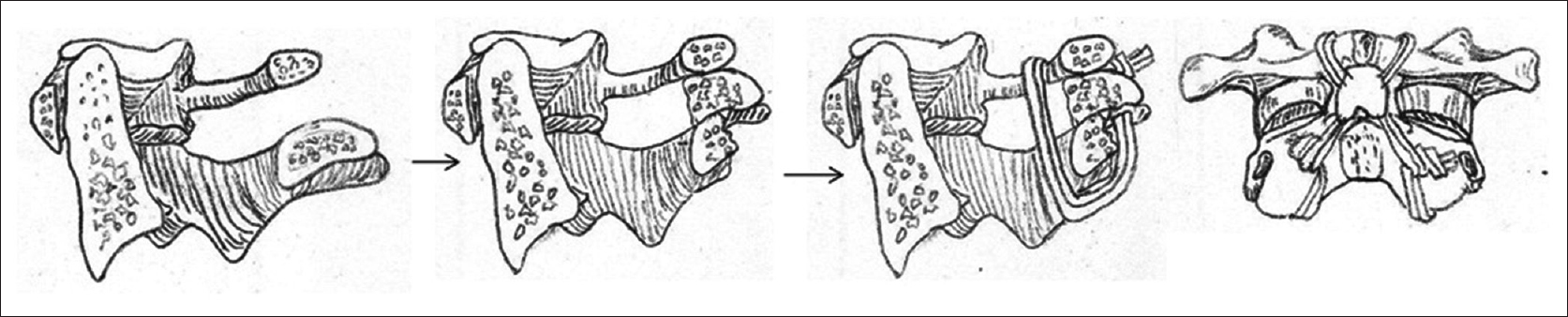
- Hand drawing showing the concept of advancement of posterior 3/4th of C2 spinous process as bone graft and wedged using sublaminar titanium cables (saggital and anteroposterior drawings)
As this technique was used only in patients with mobile reducible axial dislocation, it was not combined with other stabilizing procedures. However, in other cases with rotational instability, supplementary fixation technique can also be used in combination with the above procedure.
Results
The procedure was accomplished successfully in all patients without any operative complications. There were four male patients and one female patient with a mean age of 43.20 years. They were followed for various intervals with the longest follow up of 18 months, with a mean follow up of 12.80 ± 4.96 months. In all patients (100%), the bone graft was in place and all patients demonstrated good fusion at the end of 6 months on cervical spine X-ray [Figure 6]. CT scan of the craniovertebral junction [Figures 7 and 8] was done in first two patients at the end of 6 months which demonstrated callus formation in both and was thus not routinely done for rest of the patients. Post operative pain was evaluated using VAS at the end of 3 months. All patients had VAS score of 0 or 1 (mean VAS score of 0.4) signifying considerable reduction of post operative pain.
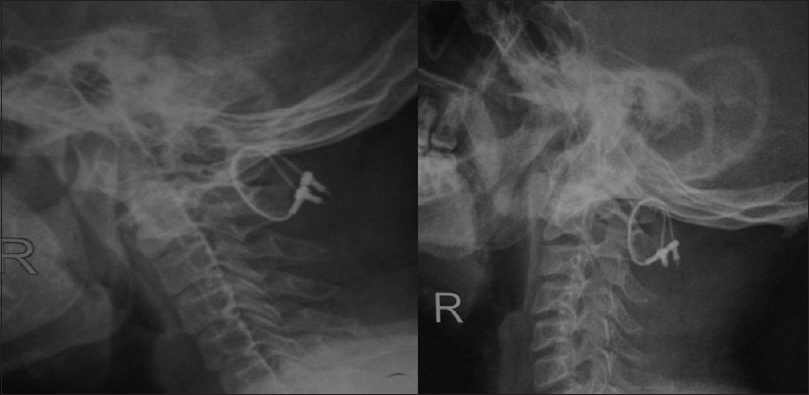
- X-ray lateral view in flexion and extension after fixation showing no dislocation with the wedged C2 spinous process which was mobilized as the vascularized bone graft

- CT scan of CV junction after fixation showing the wedged C2 spinous process with evidence of fusion

- CT scan (axial section) showing fused graft with C1
Discussion
Atlanto-axial arthrodesis has evolved to accommodate an increased spectrum of anatomical variation with basic intention to stop the mobility of atlanto-axial dislocations. Various techniques have been described to achieve good fusion and stabilization.[1011]
C1-C2 arthrodesis using graft and wire were first described by Gallie,[12] and then there were modifications including Brooks, modified Brooks and interspinous technique.[131415] Later on Magrel's techniques of C1-C2 transarticular screws, Goel's technique, Harm's technique of C1-C2 distraction and fixation came into the picture and have been tested and accepted reasonably well.[1] In all these cases, the bone graft was acquired either from the iliac crest or the ribs or allograft and bone substitutes were used. Rarely the use of vascularized fibular graft is also described for the fusion.[16] Autologus graft is preferred because of its superiority. To procure graft another incision is required and which sometimes leads to bone graft donor site morbidity.
The bone graft donor site morbidity is a well-described complication. Banwart et al.,[4] in their series of 261 patients, reported 10% major complication rate. Cockin,[17] in his review of 118 cases of iliac crest bone grafts, found minor complication in 6% cases and reported one case of herniation through bone graft donor site.
Arrington et al.,[3] in their analysis of 414 consecutive cases of iliac crest bone graft procedures, had 10% minor and 5.8% major complications.
The present technique offers the advantage of avoidance of another incision for bone graft harvesting by utilizing the locally available bone in the form of the C2 spinous process, which has not been proposed in the literature before.
The strong spinous process of C2 gives attachment to inferior oblique and rectus capitis posterior major, bulky portions of the semispinalis cervicis, spinalis cervicis, interspinalis and multifidus. Detachment of these muscles not only hampers the function of these muscles but is also a source of considerable post operative pain. Strong semispinalis cervicis attached to the C2 spinous process forms the long arms with important function of extension and rotation. It is common practice to detach the C2 spinous process of all its muscle attachments in C1-C2 posterior arthrodesis.
The concept of preserving the posterior muscular attachment has not been described for atlantoaxial arthrodesis; however, similar work has been done by Kim et al.,[9] in cervical myoarchitectonic spinolaminoplasty (MSLP), where after preserving the posterior muscular attachments to spinous processes of cervical vertebrae, they were able to demonstrate at 1 year follow up no wasting in neck extensor musculature while reducing postoperative neck pain and shoulder strain. In the present series, authors utilized the same concept of muscular preservation (especially bilateral semispinalis cervicis attachment to the C2 spinous process) to reduce post operative discomfort without compromising the chances of fusion. Also, since the semispinalis cervicis is still attached to C2 spinous graft, this works as vascularized graft with better chances of survival and fusion.
All the patients who underwent fusion using this technique showed good fusion and significant reduction in post operative pain as measured on VAS at the end of 3 months with no morbidity arising out of donor site, thus achieving the primary objectives of this technique. Though we do not have a control group to compare pain reduction with our technique but preserving posterior spinal muscles during neck dissection in cervical laminoplasty (MSLP) has been shown to reduce postoperative neck pain and shoulder strain when compared to non-myoarchitectonic spinolaminoplasty[9] and the present technique is an application of the same concept to C1-C2 arthrodesis.
This is technical modification of providing superior quality local bone graft (vascularized part of the C2 spinous process), to achieve fusion of C1-C2 posteriorly and hence can be combined with various other well-established techniques of C1-C2 posterior stabilization (namely Goel’s, Harm’s, Magrel’s, Brook's etc).[1213] Moreover, the present technique poses no problem in use of other bone substitutes along with the vascularized C2 spinous process, thereby keeping the room open for the use of other stabilization procedures with supplementary graft materials.
In the present technique along with the preservation of strong musculature of the neck attached to the C2 spinous process, we also avoided another incision for bone graft and the morbidity associated with it. This innovative technique has never been discussed in the literature before and as described it can be combined with various other techniques of posterior fixation, thereby providing flexibility of implant usage and can be easily performed by young neurosurgeons in simple neurosurgical set up without the need of extra devices or incurring extra cost.
Conclusion
The authors described a novel technique of C1-C2 posterior fusion in which the posterior 3/4th of the C2 spinous process with muscles, mainly semispinalis cervicis, attached on it, is advanced as the vascularized bone graft for the fusion. This improves the chances of fusion and avoids the bone graft donor site morbidity. The myoarchitectonic preservation of the posterior spinal musculature would help to preserve their dynamic functions and reduce the post operative pain. This can be easily combined with most of the other established techniques of C1-C2 posterior stabilization.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Techniques in the treatment of craniovertebral instability. Neurol India. 2005;53:525-33.
- [Google Scholar]
- Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001;26:2467-71.
- [Google Scholar]
- Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res 1996:300-9.
- [Google Scholar]
- Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine. 1994;20:1055-60.
- [Google Scholar]
- Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res 1997:76-81.
- [Google Scholar]
- Harvesting autogenous iliac bone grafts. A review of complications and techniques. Spine (Phila Pa 1976). 1989;14:1324-31.
- [Google Scholar]
- Analysis of harvest morbidity and radiographic outcome using autograft for anterior cervical fusion. Spine (Phila Pa 1976). 1997;22:2222-7.
- [Google Scholar]
- Rotation of the cervical spinal column: A computed tomography in vivo study. Surg Radiol Anat. 1993;15:333-9.
- [Google Scholar]
- Myoarchitectonic spinolaminoplasty: Efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine. 2007;7:293-304.
- [Google Scholar]
- Internal fixation of cervical spine: Current indications and techniques. J Am Acad Orthop Surg. 1995;3:194-206.
- [Google Scholar]
- The evolution of posterior cervical and occipitocervical fusion and instrumentation. Neurosurg Focus. 2004;16:E9.
- [Google Scholar]
- Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60:279-84.
- [Google Scholar]
- The interspinous method of posterior atlantoaxial arthrodesis. J Neurosurg. 1991;74:190-8.
- [Google Scholar]
- Modified Gallie technique versus transarticular screw fixation in C1-C2 fusion. Clin Orthop Relat Res 1999:126-35.
- [Google Scholar]
- Microvascular free bone transfer: A clinical technique. Orthop Clin North Am. 1997;8:425-47.
- [Google Scholar]
- Autologus bone grafting: Complications at the donor site. J Bone Joint Surg Br. 1971;53:153.
- [Google Scholar]






