Translate this page into:
Posterolateral approach in a neurofibromatosis type-I patient with severe dystrophic thoracic kyphoscoliosis: A case report, cadaver study, and literature review
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neurofibromatosis type-I (NF-I) is an autosomal-dominant hereditary disorder, in which spinal skeletal deformities are one of the manifestations and manifest as acquired abnormalities and present as short, sharp, and angular (usually thoracic) curves. The scoliosis can be severe requiring surgical intervention. The surgical procedure can be difficult because of scalloping of the vertebral bodies and dural ectasia. We state that in selected cases of severe thoracic dystrophic kyphoscoliosis in NF-I, the posterolateral approach is the only possible method to visualize the anterior thoracic spinal cord, perform anterior decompression, and to stabilize the thoracic deformity, because of the anterior dural ectasias and the kyphosis limiting an anterior procedure.
Keywords
Dystrophic kyphoscoliosis
neurofibromatosis type-I
surgical treatment
Introduction
Neurofibromatosis type-I (NF-1, von Recklinghausen's disease) is an autosomal-dominant single-gene hereditary disorder of neural crest cells, involving neuroectoderm, mesoderm, and endoderm.[123]
It affects 1:3000-4000 individuals and is caused by a defect in the gene responsible for the production of the protein neurofibromin: The NF-1 gene. The NF-1 gene is a tumor suppressor gene linked to the long arm of chromosome 17.[3]
The clinical manifestations of NF-1 are as follows: Cafè-au-lait spots, axillary or inguinal freckling, Lisch nodules of the iris, neurofibromas, optic gliomas, and spinal skeletal deformities. The latter manifest as acquired short, sharp, and angular (usually thoracic) scoliotic curves. Dystrophic changes such as rib-penciling, vertebral scalloping, transverse process spindling, apical wedging, foraminal enlargement, and dural ectasia are classic features.[1234]
The scoliosis and dystrophy can be severe and progressive requiring surgical intervention.[1234]
The literature is unclear regarding the ideal surgical treatment. Various procedures have been reported and entail anterior, posterior, and combined anterior/posterior approaches to establish arthrodesis and prevent curve progression.[1234]
We describe a case that highlights the operative management of an NF-1 patient with severe dystrophic thoracic kyphoscoliosis treated by a posterolateral spinal approach.
Case report
A 44-year-old patient with NF-1 presented to the Department of Neurosurgery with myelopathy caused by a 93° thoracic (T5-T9) kyphoscoliosis, thoracic vertebral scalloping leading to a severe thinning of the vertebral bodies, profound stenosis by a bony ridge between two dural ectasias at T4-T5 anteriorly and auto fusion of T4-T7 [Figures 1 and 2].
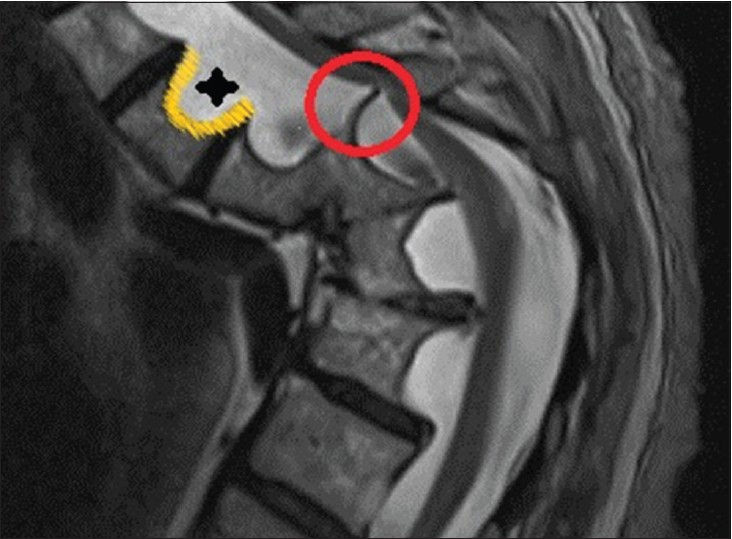
- Magnetic resonance image of a 93° thoracic kyphoscoliosis and stenosis due to a bony ridge (red circle) between two dural ectasias at T4-T5 anteriorly and an autofusion of T4-T7. Note the dural ctasias (asterix) and the vertebral scalloping (yellow curve)

- Computed tomography image of the thoracic spine with a 93° kyphoscoliosis. Note the bony anterior autofusion of T4-T7
Clinically, she had progressive sensory disturbances and upper motor signs. Operative intervention, performed using intraoperative neuromonitoring, consisted of a posterolateral approach with posterior thoracic cord exposure, anterior decompression of the bony ridge on T4-T5 by a right costotransversectomy [Figure 3] at T4 and posterior fusion of C6-T12 with bilateral pedicle screws at the C6, T11, and T12 level as well as bilateral bridging rod instrumentation [Figures 4 and 5]. The deformity was not corrected but stabilized. At followup, the patient was asymptomatic with a lasting curve stabilization.

- Cadaver view of the anterior thoracic spinal cord with the thoracic nerve root lifted upward (curved arrow) after a performed right costotransversectomy at T4. Note the detailed exposure of the anterior spinal cord with its epidural space (white circle), corresponding veins (black arrow), and the posterior longitudinal ligament (white arrow). Remark: The spinous process and the lamina have been removed for demonstrative purposes

- Postoperative X-ray image showing the posterior fusion from C6 to T12 with bilateral pedicle screws at the C6, T11, and T12 level and bilateral bridging rods

- Postoperative computed tomography image with posterior fusion of C6-T12. Note the pedicle screws at the C6, T11, and T12 level as well as the resection of the bony ridge at T4-T5 (red circle)
Discussion
Scoliosis is the most frequent musculoskeletal manifestation in NF-1. It occurs usually in the low thoracic region and has a prevalence ranging from 2% to 69% in the literature.[23]
Etiological theories regarding NF-1-related scoliosis include erosion or infiltration of bone by neurofibromas, primary mesodermal dysplasia, osteomalacia, and endocrine disturbances.[3]
NF-1 scoliosis has two recognized subtypes: Non-dystrophic and dystrophic curve patterns. This classification is based on the absence or presence of skeletal dysplasia, such as vertebral scalloping and associated dural ectasias, rib penciling, vertebral wedging, transverse process spindling, paraspinal or intraspinal soft tissue masses, apical rotation, foraminal enlargement, pedicle dysplasia, and widened interpediculate distance.[234] The literature states that the likelihood of curve progression and deterioration is proportional to the severity of skeletal dystrophy. Studies have shown that when a combination of three or more dysplastic features are present, the risk of curve deterioration was significantly increased in 85% of patients.[3]
Non-dystrophic curves can be managed as idiopathic scoliosis, dystrophic curves, however, need a more aggressive approach. A dystrophic curve pattern, as this was the case in our patient, classically presents as a short segment, sharply angulated, thoracic curve with three or more dystrophic elements. They require aggressive treatment as there is a strong tendency for curve progression and clinical catastrophic deterioration.[1234]
Dystrophic scoliosis less than 20° should be closely monitored at 6 month intervals. In scoliosis, measuring 20°-40° with less than 50° of kyphosis, a posterior spinal arthrodesis is feasible. However, when the scoliosis exceeds 40° and/or thoracic hyperkyphosis exceeds 50°, a combined anterior/posterior (circumferential) fusion is mandatory.[34]
Neurological deficits are usually caused by hyperkyphosis and subsequent attenuation and deformation of the spinal cord. In those cases, an anterior decompression followed by circumferential fusion should be pursued. Other contributory factors include intraspinal tumors, which have to be resected followed by a mechanical stabilization and bony fusion.[3]
One of the difficulties encountered in NF-spinal surgery is the segmental instrumentation and fusion as there can be poor anchorage points for internal fixation due to vertebral destruction. Consequently, bony autograft augmentation and postoperative bracing and/or orthostatic immobilization are necessary.[3]
Due to the high incidence of pseudarthrosis, fusion evaluation should be performed at 6 months and at regular intervals until solid arthrodesis is obtained. In case of failure, an augmentation is mandatory.[23]
In our case, the neurological deficit was caused by a 93° thoracic (T5-T9) kyphoscoliosis and stenosis due to a bony ridge between two dural ectasias at T4-T5 anteriorly [Figure 1]. Furthermore, there was an autofusion of T4-T7 [Figures 1 and 2].
Due to the anterior T4-T7 autofusion, severe kyphosis, and the presence of dural actasias, we did not perform a combined anterior/posterior approach. We choose a posterolateral approach [Figure 3] instead with thoracic cord exposure, anterior decompression of the bony ridge on T4-T5 by a right costotransversectomy at T4 and posterior fusion of C6-T12 with bilateral pedicle screws at the C6, T11 and T12 level as well as bilateral bridging rod instrumentation [Figures 4 and 5]. The deformity was not corrected but stabilized. Intraoperative neuromonitoring and postoperative recovery as well as follow up were uneventful.
We state that in selected cases of severe thoracic dystrophic kyphoscoliosis in NF-I, the posterolateral approach [Figure 3] is the only possible method to visualize the anterior thoracic spinal cord, perform anterior decompression, and to stabilize the thoracic deformity, because of the anterior dural ectasias and the kyphosis limiting an anterior procedure.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Thoracic kyphoscoliosis resembling neurofibromatosis: A case report focusing on subfascial instrumentation. Spine J. 2002;2:151-5.
- [Google Scholar]
- Neurofibromatosis type I with severe dystrophic kyphoscoliosis and its operative management via a simultaneous anterior-posterior approach: A case report and review of the literature. Spine J. 2005;5:461-6.
- [Google Scholar]
- Spinal deformity in neurofibromatosis type-1: Diagnosis and treatment. Eur Spine J. 2005;14:427-39.
- [Google Scholar]
- Dystrophic kyphoscoliosis in neurofibromatosis type I: A report of two cases and review of the literature. Eur Spine J. 1997;6:273-7.
- [Google Scholar]






