Translate this page into:
Psychiatric disorders revealing multiple sclerosis after 20 years of evolvement
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Previous research indicates that the onset of psychiatric disorders is sometimes associated with multiple sclerosis (MS) evolving several years later. However, information on why this might occur, and on the outcomes of such patients, is still lacking. We aim to discuss these limitations with the current paper. We describe a 51-year-old female who demonstrated severe anxiety disorder and depression years before developing MS neurological symptoms. The patient was treated for these psychiatric disorders over 20 years. In the last 3 years of her treatment, the patient demonstrated a choreic-type of movement disorder in all her limbs. This disorder is consistent with relapsing-remitting MS. Clinical and magnetic resonance imaging (MRI) examinations demonstrated aspects of MS, without MS being diagnosed conclusively. The visual evoked potential indicated a diagnosis of conduction abnormalities. The established diagnosis was slow relapsing MS. The patient underwent methylprednisolone bolus (1 g/day). This case-study suggests that health professionals should conduct a full neurological assessment when they find atypical psychiatric symptoms in a patient. This would make sure that patients receive a better standard of care, and thus experience a better quality of life.
Keywords
Lengthy and very slow evolvement
multiple sclerosis
psychiatric disorders
Introduction
Psychiatric disorders associated with the onset of multiple sclerosis (MS) have already been reported and studied. However, information on the outcome of such patients is still lacking.[123] Indeed specific psychiatric symptoms and the long-term evolution of psychiatric disorders could be caused by the development of either asymptomatic or symptomatic MS.[123456] Extensive study of patients with established MS diagnoses demonstrates that such patients might develop psychiatric disorders at any stage of the evolving MS pathology.[25] However, psychiatric disorders occurring several years before MS diagnosis has already been described in the literature, but the phenomenon is still not understood clearly. We describe a patient who demonstrated severe anxiety disorder and depression for a number of years prior to the onset of MS neurological symptoms.
Case Report
A 51-year-old female is being treated for anxiety and depression for the past 20 years without any improvement. Six years ago, the patient presented bilateral reduced vision to a 2 inch scale of 10 units. Three years ago, the patient demonstrated a choreic-type movement disorder in all her limbs, as well as weakness down the right side of her body. These symptoms had a relapsing then remitting pattern. One year ago, the patient showed sphincter disorders with uncontrolled urine outflow, dysarthria, and impairment of short-term memory. The patient did not have any history of bipolar aphthosis. Neurological examination demonstrated extrapyramidal syndrome in all limbs, pyramidal syndrome, cerebellar syndrome, deep sensitivity disorders, and amnesia of fixation with neuropsychological disturbance (with an EDSS Expanded Disability Status Scale (EDSS) score of 7.5).
The cerebral and medullar magnetic resonance images (MRI; Figures 1 and 2) showed multiple hyperintensities in the T2-weighted image, and FLAIR images in the periventricular and subcortical white matter, brainstem, corpus callosum, and spinal cord. The gadolinium injection did not show any contrast enhancement. The Barkhof criteria were fully filled.

- FLAIR MRI images demonstrating hyper-signal in the tentorial area and central gray nucleus
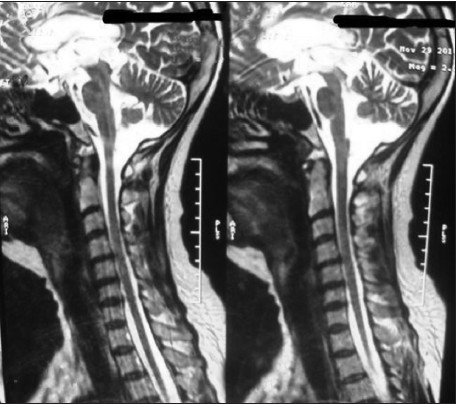
- T2-weighted MRI images demonstrating hyper-signal in the brain stem, medullar, and dorsal spinal cord
Cerebrospinal fluid (CSF) study demonstrated a normal protein rate of 0.43 g/l. Meningitis test was negative, while the electrophoresis study of synthetic proteins in the blood and CSF demonstrated the presence of immunoglobulin G. The antibodies’ antinative DNA and antinuclear antiphospholipid investigation both demonstrated search negative results. The human immunodeficiency virus (HIV) serology, Lyme serology, and Whipple were all negative. The salivary gland biopsy result was normal, while the visual-evoked potential showed conduction abnormalities with a latency delay of P100.
The final diagnosis was slow relapsing MS. The treatment consisted of methylprednisolone bolus of 1 g/day for 5 days while a more general treatment protocol using mitoxantrone was discussed. Since the patient could not afford this treatment, cyclophosphamide (Endoxan) was prescribed every 2 months.
Discussion
Psychiatric symptoms are common in MS pathology. However, it is uncommon for psychiatric symptoms to lead to the onset of MS.[78] Indeed, psychiatric disorders may occur many years before the onset of neurological symptoms. This delay might range from a few to 25 years.[9] Blanc et al. studied 18 MS patients who showed psychiatric disorders corresponding to their first or second demyelinating event;[9] these psychiatric disorders were various and included delusions of persecution, manic episodes, melancholy, hysteric conversion, and obsessive compulsive disorder.[7] This study included 13 patients who showed psychiatric symptoms, which were the first signs of MS.[7]
The patient described in the present paper demonstrated severe anxiety, depression, and behavioral disorders for 14 years before the onset of MS neurological symptoms. These psychotic episodes appear to have been the signs of MS-related events. This patient presented with progressive MS with relapsing-remitting symptoms. Indeed the cerebral and medullar MRI fully filled the Barkhof criteria of space distribution. Reports of psychiatric disorders leading to the onset of MS are rare in the literature, while the onset of psychiatric disorders in MS patients is a common reality.[10] In an attempt to better understand the relationship between psychiatric clinical pathology symptoms and MS, the authors suggest that MS lesions are perhaps not strictly restricted to the regions of the brain that are commonly observed during MS-related brain imaging. Instead, it might be the case that disconnection phenomena occur in the white matter of MS patients. These disconnections are actually highly correlated with cognitive impairment in MS patients.[11] Methodology-wise, diffusion tensor MRI, functional MRI and electroencephalogram (EEG) would be the best approaches for understanding the brain tissue network involved in this association between psychiatric disorders and MS tissue impairment. Disconnection in the white matter certainly seems to play a major role, especially in early stages of MS.[12]
Nonetheless, the psychiatric disorders associated with white matter disconnection are not completely understood, hence subjecting MS patients with psychiatric disorders to diffusion tensor MRI would also help to increase understanding of this phenomenon, especially in the context of studies involving large numbers of participants. Such imaging would also mean that individual patients receive better levels of care.[12]
In practical terms, the long-term psychiatric symptoms presented by our patient suggest that psychiatrists should regularly carry out MRI scans (including diffusion tensor imaging of the brain) on their patients. Doing so would enable any neurological symptoms to be detected and treated earlier, thus enhancing patients’ quality of life.
Conclusion
There appears to be an important relationship between chronic psychiatric disorders and later MS onset, which may be due to disconnection in the white tissue. This implies that patients with psychiatric symptoms should receive a full neurological assessment, including brain imaging investigations. Such an initiative would allow for a better understanding of any psychiatric disorders occurring before and/or during MS onset, and would also provide patients with a better quality of life.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Similar autobiographical memory impairment in long-term secondary progressive multiple sclerosis and Alzheimer's disease. Mult Scler. 2013;19:225-32.
- [Google Scholar]
- Outcome of psychiatric symptoms presenting at onset of multiple sclerosis: A retrospective study. Mult Scler. 2010;16:742-8.
- [Google Scholar]
- Changing associations between cognitive impairment and imaging in multiple sclerosis as the disease progresses. J Neuropsychiatry Clin Neurosci. 2013;25:134-40.
- [Google Scholar]
- Treatment with edaravone, initiated at symptom onset, slows motor decline and decreases SOD1 deposition in ALS mice. Exp Neurol. 2008;213:448-55.
- [Google Scholar]
- How long can you keep working with benign multiple sclerosis? J Neurol Neurosurg Psychiatry. 2011;82:78-82.
- [Google Scholar]
- Depression-like changes of the sleep-EEG during high dose corticosteroid treatment in patients with multiple sclerosis. Psychoneuroendocrinology. 2003;28:780-95.
- [Google Scholar]
- Inaugural psychotic events in multiple sclerosis? Rev Neurol (Paris). 2010;166:39-48.
- [Google Scholar]
- Patients with multiple sclerosis presenting to psychiatric hospitals. J Clin Psychiatry. 1995;56:297-308.
- [Google Scholar]
- Bipolar affective disorder prior to the onset of multiple sclerosis. Acta Neurol Scand. 1993;88:388-93.
- [Google Scholar]
- Sequential magnetic resonance imaging follow-up of multiple sclerosis before the clinical phase. Mult Scler. 2005;11:395-7.
- [Google Scholar]
- Disconnection as a mechanism for cognitive dysfunction in multiple sclerosis. Brain. 2009;132:239-49.
- [Google Scholar]
- Cognitive dysfunction in patients with mildly disabling relapsing-remitting multiple sclerosis: An exploratory study with diffusion tensor MR imaging. J Neurol Sci. 2002;195:103-9.
- [Google Scholar]






