Translate this page into:
Unusual occurrence of supratentorial medulloepithelioma in a young female
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Medulloepithelioma is an extremely rare PNET in late adolescence and adults with only two cases noted in literature. These are WHO grade IV tumors with dismal prognosis. Only few cases survived beyond 5 months. We report a rare case of supratentorial medulloepithelioma in a 17 year old girl. She had presented with right sided weakness, headache and vomiting. Imaging showed an enhancing mass lesion in left parietal region which undergone gross total resection. After surgery, her headache, vomiting and right sided weakness improved. On histopathology, the tumor had characteristic trabecular, ribbon and palisaded arrangement with brisk mitotic activity, necrosis and calcification. Immuno-histochemistry revealed positivity for Synaptophysin, Vimentin and EMA while GFAP was negative. MIB-1 labeling was very high. Patient received postoperative radiotherapy. On follow up after 14 months, she was clinically asymptomatic with no recurrence on imaging.
Keywords
Late adolescence and adults
medulloepithelioma
primitive neuroectodermal tumor
supratentorial
Introduction
Central Nervous System primitive neuroectodermal tumors (PNET) are a heterogeneous group of embryonal tumors. They have varying capacity for differentiation along neuronal, astrocytic and ependymal lines. PNETs that display features of the embryonal neural tube formation are termed medulloepitheliomas.[1] These are rare tumors with only 36 cases recorded in literature with the peak incidence between six months to five years of age.[2] Medulloepithelioma presenting in the older age group is extremely rare, and only two cases have been reported.[34] We report a rare case of supratentorial medulloepithelioma in a 17-year-old girl, the first case to be reported in late adolescence.
Case Report
A 17-year-old girl presented with a history of right-sided weakness for 30 days and headache and vomiting for 15 days. On examination, she had right hemiparesis with upper motor neuron (UMN) facial paresis and hemisensory loss. Fundi examination revealed bilateral papilledema. Her vitals were stable and her basic biochemical parameters were within normal limits. Preoperative magnetic resonance imaging (MRI) revealed a large extra-axial lesion that was hypointense on T1WI and heterogeneous on T2WI, with strong heterogeneous enhancement and necrosis on a post-contrast study. Axial fluid attenuated inversion recovery (FLAIR) images revealed perilesional edema, with partial inversion within the lesion. There was perilesional edema with a midline shift [Figure 1a–d]. DWI shows areas of restricted diffusion at the margin of the lesion [Figure 1e]. Magnetic resonance spectroscopy (MRS) revealed a markedly elevated choline peak, with decreased N-acetylaspartate (NAA) [Figure 1f]. The patient underwent left parietal craniotomy and gross total excision. Intraoperatively, the tumor was grayish, minimally vascular, soft, and lobulated, with a good plane of cleavage from the normal brain. A postoperative computed tomography (CT) scan of the brain confirmed complete tumor removal. Her headache, vomiting, and right-sided paresis improved in the subsequent days.
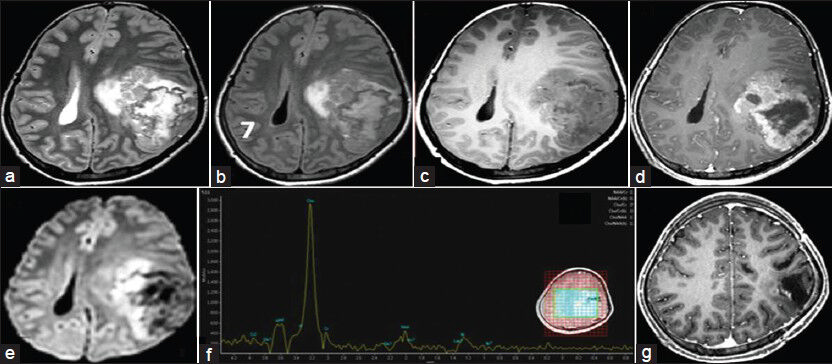
- (a and b) The axial T2W/FLAIR image shows a large extra-axial mass lesion with heterogenous signal intensity and edema of the adjacent brain parenchyma; (c and d) The axial T1W image shows a hypointense lesion, which shows strong heterogeneous enhancement; (e) DWI shows areas of restricted diffusion; (f) MRS shows elevated choline; (g) Postoperative T1W images reveal no residual mass lesions
On histopathology, the tumor had solid nests of immature neuroepithelial cells in characteristic ribbons, tubules, trabaculae, and palisaded arrangement, with an external limiting membrane reminiscent of an embryonic neural tube [Figure 2a–c]. The mitotic activity was brisk, with large zones of necrosis and dystrophic calcification [Figure 2d]. Immunohistochemistry revealed diffuse positivity for Vimentin, while focal expression of synaptophysin was seen to be limited to the ribbons and trabeculae, reflecting neuroepithelial derivation, mimicking the neural tube [Figure 2e]. It showed focal positivity for the Epithelial Membrane Antigen (EMA) [Figure 2f], while the Glial Fibrillary Acidic Protein (GFAP) was negative [Figure 2g]. MIB-1 labeling was very high, exceeding 25% [Figure 2h]. INI-1 expression was retained, excluding the possibility of an atypical rhabdoid teratoid tumor, with divergent lines of differentiation. No teratomatous component was detectable. The histopathological features were diagnostic of medulloepithelioma.

- The tumor shows immature neuroepithelial cells in papillary (a) and trabecular arrangement (b), with a PAS positive external limiting membrane (c), and necrosis and calcification (d). The tumor cells show strong synaptophysin (e) and focal EMA positivity (f), while GFAP is negative (g). MIB-1 labeling is high (h). [a and b: H and E, ×Obj.10, c: PAS ×Obj.20, d: H and E, ×Obj.20, e: Synaptophysin ×Obj.20, f: EMA ×Obj.40, g: GFAP ×Obj.10, h: MIB-1 ×40]
The patient received postoperative radiotherapy. On follow-up, after 14 months, the patient was clinically asymptomatic and MR imaging confirmed the absence of cranial and spinal recurrence [Figure 1g].
Discussion
Medulloepitheliomas are rare childhood embryonal tumors, with a peak incidence between six months and five years of age, with no specific sex predilection.[25] However, their occurrence beyond this age range has also been reported.[34] This tumor was initially classified as the most primitive neoplasm of the Central Nervous System (CNS) in 1926, by Bailey and Cushing, and later as a medulloepithelioma not otherwise specified, or a medulloepithelioma with differentiation by Rorke et al.[2] The 2007 World Health Organization (WHO) Classification of Tumors of the CNS reclassified embryonal tumors as Medulloblastoma, CNS Primitive Neuroectodermal Tumor (PNET), and Atypical Teratoid/Rhabdoid Tumor (AT/RT). CNS PNET includes CNS Neuroblastoma, CNS Ganglioneuroblastoma, Medulloepithelioma, and Ependymoblastoma (Supratentorial PNET). These are WHO grade IV tumors, showing a tendency for widespread infiltration of the surrounding tissue and craniospinal dissemination.[1] PNETs constitute only about 3.6% of all brain tumors and 22% of primary childhood and adolescent CNS tumors.[5] Medulloepitheliomas are mostly supratentorial lesions commonly found in the periventricular location, which suggests that they might arise from primitive undifferentiated matrix cells. They are mostly supratentorial in the periventricular location, involving in order of frequency, the temporal, parietal, occipital, and frontal lobes, however, peripheral locations like the cauda equina, sciatic nerve, and orbit have rarely been reported in literature.[2678] They display a highly malignant behavior, with early progression or recurrence and dismal prognosis. Most children die within five months, and only three cases have survived beyond five years.[12679] There are only two previously reported cases in adults, aged 23 and 20 years, located in the fronto-temporal and temporal lobes.[34]
Both cases, however, have been reported before the era of immunohistochemistry. The case details are provided in Table 1.
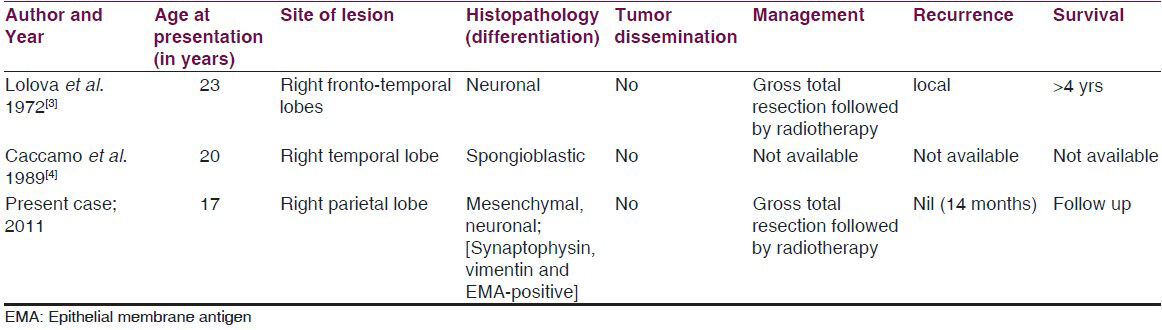
Similar to the previously reported cases, our case presented with signs of raised intracranial tension and showed a predominantly large hypointense lesion on T1WI, hyperintense on T2WI, in the left parietal region, with surrounding edema and mass effect with midline shift, and showed enhancement on contrast[27] On histopathology, multiple lines of differentiation, including, neuronal and mesenchymal elements, and glial differentiation were reported by employing immunohistochemistry.[126810] In the case reported here, evidence for neuronal and mesenchymal differentiation was evident and follow-up confirmed 14 months of recurrence-free survival.
Supratentorial location, gross total resection, absence of cerebrospinal fluid (CSF) dissemination, and postoperative aggressive chemoradiotherapy are reported to be associated with a favorable outcome.[2689] To date five long-term survivors (three children and two adults) are reported and have been reviewed by Matsumotu et al.[11] All cases with long-term survival underwent gross total excision of the tumor followed by chemoradiotherapy. Although Moftakhar et al.,[2] in their review of 36 published cases of medulloepithelioma noted that age and sex had no influence on the prognosis, all the older patients reported, including the present case had longer survival.[34] This may be attributed to the feasibility of aggressive chemotherapy and radiotherapy, with gross total resection in adults compared to children. In children, the risk of radiation-induced effects on the developing brain, such as, cognitive decline or development of secondary tumors are high, precluding aggressive adjuvant therapy. Newer modalities of treatment, such as, myeloablative therapy or high-dose chemotherapy, with autologous hematopoietic progenitor cell rescue (HDC/AuHCR) have been evaluated in the treatment of highly malignant CNS PNETs in children and young adults, including medulloepitheliomas,[9] as an alternative to radiotherapy. Its effectiveness remains to be proven.
It is tempting to speculate if the degree of histological differentiation could influence survival. A greater degree of differentiation makes tumors refractory to chemo- and radiotherapy and more prone to relapse as demonstrated in PNETs.[12] Perhaps this accounts for poor survival in medulloepitheliomas that display differentiation along divergent lines, such as, neuronal, glial, and mesenchymal elements, unlike PNETs that are highly undifferentiated. Interestingly, Moftakhar and colleagues noted that all cases of medulloepitheliomas with recurrences had well-differentiated tumors,[2] This aspect could not be investigated in two cases reported in adults as immunohistochemistry was not performed to ascertain the degree of differentiation. Whether the lineage of differentiation could influence prognosis or survival has not been explored. The case reported here demonstrated a predominant neuronal and mesenchymal line of differentiation, without glial or epithelial differentiation.
Necessity to look for alternative molecular markers and directed treatment similar to INI-1 in atypical teratoid rhabdoid tumors is emerging. In recent times, hTERT oncogene amplification has been demonstrated in a proportion of embryonal tumors, particularly medulloblastomas, as well as, medulloepitheliomas.[13] A correlation with survival has been suggested and whether this might emerge as a molecular marker in future remains to be seen.
Conclusion
Medulloepithelioma is a rare PNET of childhood with dismal prognosis. Its occurrence in late adolescence and in adults is extremely rare with only two other cases reported in literature. Gross total resection followed by Radiotherapy and Chemotherapy is the current mode of treatment.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- The 2007 WHO classification of tumors of the central nervous system. Acta Neuropathol. 2007;114:97-109.
- [Google Scholar]
- Long-term survival in a child with a central nervous system medulloepithelioma. J Neurosurg Pediatr. 2008;2:339-45.
- [Google Scholar]
- Cerebral medulloepithelioma. Histological and histochemical study of a case. J Neurol Sci. 1972;15:173-82.
- [Google Scholar]
- An immunohistochemical study of the primitive and maturing elements of human cerebral medulloepitheliomas. Acta Neuropathol. 1989;79:248-54.
- [Google Scholar]
- CNS and miscellaneous intracranial and intraspinal neoplasms. In: Reis LA, Smith MA, Gurney JG, Linet M, Tamra T, Young JL, eds. Cancer incidence and survival among children and adolescents. Bethesda, MD: United States SEER program 1975-1995. National cancer institute SEER program, United States of America: NIH Publication; 1999. p. :51-63. No. 99-4649
- [Google Scholar]
- Medulloepithelioma of the optic nerve with intradural extension-report of two cases and a review of the literature. Childs Nerv Syst. 2000;16:329-33.
- [Google Scholar]
- Unusual clinical and MRI features of a cerebellopontine angle medulloepithelioma. Pediatr Neurosurg. 2006;42:299-303.
- [Google Scholar]
- Recurrent central nervous system medulloepithelioma: Response and outcome following marrow-ablative chemotherapy with stem cell rescue. J Pediatr Hematol Oncol. 2005;27:264-6.
- [Google Scholar]
- Cerebral medulloepithelioma-electron microscopy and immunohistochemistry. Acta Neuropathol. 1990;80:103-7.
- [Google Scholar]
- Cerebral medulloepithelioma with long survival. Neurol Med Chir (Tokyo). 2007;47:428-33.
- [Google Scholar]
- Differentiation, proliferation and apoptosis in primary and recurrent primitive neuroectodermal tumors of childhood. Childs Nerv Syst. 2001;17:320-7.
- [Google Scholar]
- hTERT gene amplification and increased mRNA expression in central nervous system embryonal tumors. Am J Pathol. 2003;162:1763-9.
- [Google Scholar]






