Translate this page into:
Pericallosal lipoma associated with subcutaneous lipoma in an adult
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
SuIntracranial lipomas are rare and they generate 0.06-0.46% of all intracranial lesions.[1] They often occur in the supratentorial midline at the pericallosal cistern. And they are called as pericallosal lipoma. Suprasellar cistern, chiasmatic cistern, cerebellopontine angle, silvian fissure, quadrigeminal cistern are the other locations that they are seen. In the past, the intracranial lipomas were described as benign tumors. However, now, they are described as congenital malformations caused by the differentiation of persistent primitive meninges as a form of adipose tissue.[1] A 26-year-old female patient. She was born mature and as normal birth. She is the fourth child of the family, and there is no subcutaneous lipoma history in the family. There is swelling on the scalp. The patient was taken to other medical centers by her family during her childhood. However, after being an adult, she didn’t want to go to the medical centers because she didn’t want her lesion to be known, and she hasn’t gone to the controls for nearly 15 years. The patient doesn’t describe any headache or attack history. The patient applied to the polyclinic because she couldn’t comb her hair easily, and she didn’t want her lesion to be seen in terms of cosmetics. She covers her hair to hinder her lesion to be seen from outside. In her examination, hypertelorism, neck shortening, oversized head, or mental retardation were not identified. Her cranial nerve examination was normal, and optic fundus was normal. On the scalp area, there were subcutaneous lipoma lesion, which had extended towards the extracranial area through anterior fontanelle and which was about 12 × 10 cm size and in motion with palpation and having stiffness like rubber and which was spread on frontal bone in front and on the sides and back of the parietal bones. Although the lesion was on the scalp area, there was no hair on the lesion. In MRI examination, in T1- and T2-weighted cranial MRI views, there was a view compatible with lipoma settled on corpus callosum, which has filled hyperintense interhemispheric fissure [Figure 1]. The subcutaneous lipoma was present, in which a small portion was also detected underlying the closure defect of the anterior fontanelle [Figure 2]. An irregular azygos anterior cerebral artery were also detected [Figure 3]. Venous collector veins of subcutaneous lipoma were entering into superior sagittal sinus [Figure 4]. An operation with the cosmetic purposes for the subcutaneous lipoma was proposed to the patient. The patient refused the operation. Symptomatic treatment of the patient was not performed because the patient did not describe any headache or attack history. The patient was called to the controls after 3 months, and recommendations were made.
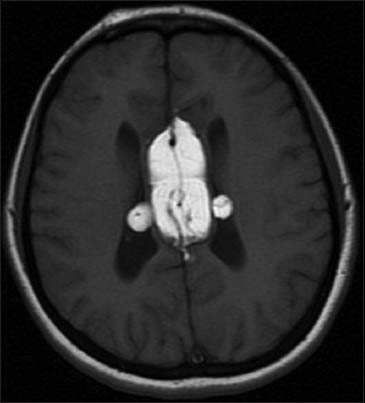
- T1-weighted magnetic resonance imaging examination shows corpus callosum lipoma with intraventricular extension

- Axial T1-weighted magnetic resonance imaging reveals intracranial part of subcutaneous lipoma (white arrow)
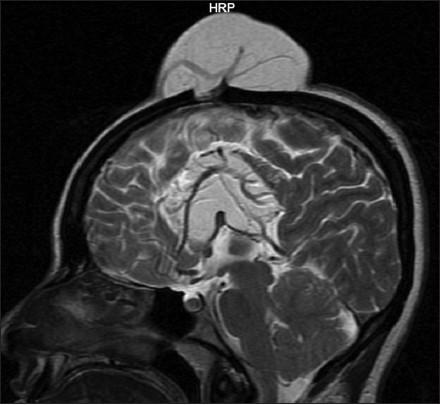
- Sagittal T2-weighted magnetic resonance imaging examination demonstrates corpus callosum lipoma and huge subcutan lipoma with anterior fontanelle bone defect. Irregular azygos anterior cerebral artery is also seen
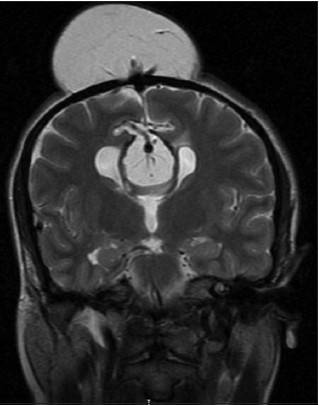
- Coronal T2-weighted magnetic resonance imaging examination demonstrates venous drainage of subcutaneous lipoma to the superior sagittal sinus
More than half of the intracranial lipomas are seen together with neural tissue anomalies such as agenesis of corpus callosum, cortical dysplasia, vascular anomalies,[1] and they occur as a result of the deterioration of the persistent primitive meninges during differentiation.[2] Intracranial lipomas together with subcutaneous lipomas are seen rarely.[34] They may have a direct continuity (with cranium bifidium) with fibrolipomatosis stalk or there is no connection. According to Truwit and Barkovich,[1] the connection of intracranial lipoma to subcutaneous lipoma through cranium bifidium occurs with invagination of primitive meninges. In our case, a small piece of lipoma was entering into the intracranial region through the bone defect at the anterior fontanelle. The venous drainage of subcutaneous lipoma was drained into the superior sagittal sinus. Interhemispheric lipomas are divided into two as curvilinear type and tubulonodular type, and each of them has distinct features. The curvilinear types are at the posterior localization and thin; on the other hand, the tubulonodular types are at the anterior and larger. The tubulonodüler type can be seen together with agenenis of corpus callosum, calcification, frontal bone defect, and mental changes. When tubulonodular type occurs before the closure of the anterior neuropore, it is together with other anomalies. On the other hand, because curvilinear type occurs later, it is not together with cerebral anomalies. Yet, such typing at each case may not be possible. The vascular pathologies such as the distention at the adjacent artery or veins, kink, arteriovenous malformation, aneurysm can be together with intracranial lipomas. The intracranial lipomas are usually asymptomatic. However, they can be symptomatic if they have accompanying development anomalies. Dysgenesis or agenesis of the corpus callosum and the cortical malformation can cause attack[5] and hydrocephalus[3] by lipoma mass effect in the quadrigeminal cistern. Our patient was asymptomatic. Magnetic Resonance Imaging (MRI) is the best way of diagnosis in the lesion follow-up and in showing the presence of calcification around the lipoma and the lesion follow-up, and in showing the presence of the dysgenesis/agenesis of corpus callosum and the intracranial lipomas. The intracranial lipomas are seen in T1- and T2-weighted MRI images as hyperintense. In our patient, there was bilateral lipoma in the choroid plexus of the lateral ventricle. If there is a link between intracranial and sub-cutaneous lipoma, this can best be seen through an MRI examination. The treatment of the intracranial lipomas are usually conservative.[1] The existing corpus callosum is not suitable for surgery, and if there are cranial nerve disorders, attack or headache history, the symptomatic treatment can only be given towards these.[5] The treatment of the extracranial lipomas can be made as surgical in terms of cosmetics and in order to prevent a possible infection related to the rupture of the vesicle. Extracranial lipomas can be treated during early childhood such as congenital malformations.[4] No patients in adulthood have been reported as our case. According to our case, it is being understood that subcutaneous lipoma hasn’t caused any problems until adulthood, except being a cosmetic problem. The surgical removal of the subcutaneous part is required for cosmetic reasons. The intracranial extent of the lipoma before operation and the vascular structures should be evaluated in detail.
References
- Pathogenesis of intracranial lipoma: An MR study in 42 patients. AJNR Am J Neuroradiol. 1990;11:665-74.
- [Google Scholar]
- Lipomas in the corpus callosum and the forehead, associated with a frontal bone defect. Surg Neurol. 1984;22:503-8.
- [Google Scholar]
- Case report. Interhemispheric lipoma associated with subcutaneous lipoma. Eur Radiol. 1998;8:628-30.
- [Google Scholar]
- Interhemispheric lipoma associated with frontal subcutaneous lipoma. J Plast Reconstr Aesthet Surg. 2009;62:e427-9.
- [Google Scholar]
- Parietal lipoma associated with cortical dysplasia and abnormal vasculature: Case report and review of the literature. AJNR Am J Neuroradiol. 2000;21:1718-21.
- [Google Scholar]





