Translate this page into:
Etiological beliefs of patients with neurological disorders attending a tertiary care center: A cross-sectional study
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The understanding and management of neurological disorders is undergoing revolutionary changes over the last three decades in the background of ever increasing advances in medical technologies, diagnostic techniques, therapeutic processes and, molecular and genetic medicine. The fruits of these advances can reach patients only if the psychosocial hurdles in their delivery are identified, acknowledged and addressed.
Aim:
To explore the beliefs and practices of patients with neurological disorders in a tertiary care center in the eastern Nepal.
Materials and Methods:
One hundred patients attending neurology/medicine outpatient for neurological disorders were interviewed about their beliefs regarding the triggering factors, causation and treatment-seeking behavior particularly from traditional healers.
Result:
Of the 100 patients (49 males, 51 females) recruited in the study, 51% expressed having ‘no idea’ about their illness. Only 20% patients gave medically congruent explanation for their illness. Psychological factors were attributed as triggering factors by 16% of patients, of which two-thirds were females. Chance, destiny and ‘jadu tona’ topped the list of triggering factors. Forty-four percent patients had sought help of traditional faith healers (‘Dhami Jhakri’) before seeking medical help. Traditional faith healers were approached by patients irrespective of their educational background. Fifty-nine percent of patients who first sought traditional faith healers, believed in ‘jadu-tona’. Of those interviewed, 16% were planning to go to a faith healer in near future.
Conclusion:
The beliefs of patients with neurological disorders frequently do not conform to current medical opinion. There is need for greater communication and education of patients by their treating physicians.
Keywords
Attitude
beliefs
neurological disorders
practices
Introduction
There has been a revolution in the field of management of neurological disorders over the last around two decades. Advances in molecular and genetic medicine have resulted in more accurate diagnosis of neurological disorders. We have greater insight of the underlying processes causing the neurological derangements. The fruit of these advances can reach the patients only if their perceptions, opinion and practices are congruent with the newer information and developments. Patients form divergent opinions about the etiology of diseases and have their own view about the treatment of disorders. They are often unaware about the technical jargon and search for explanations about their problems depending on their education level, family background, social and cultural practices. Their opinions and perceptions may not match with the current medical knowledge and practices. In a developing country, poverty, ignorance and illiteracy prevails. People still believe in traditional faith healing, witchcraft and quacks. These beliefs and practices are likely to influence time to seek medical advice and persistence with appropriate medical regimen. It is imperative for the treating physician to know, understand, acknowledge and address the issues related to beliefs and perceptions of patients so that the patients get the most out of the medical therapy. We explored the beliefs of patients undergoing treatment as outpatients in a tertiary care center in Nepal for neurological diseases and tried to assess how far do opinions of patients with neurological disorders conform to the current medical opinion.
Materials and Methods
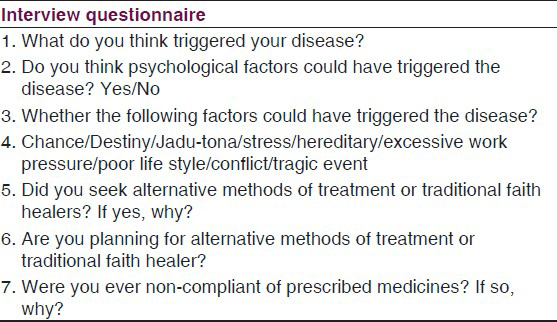
The study was a descriptive cross-sectional study of 100 patients with neurological disorders presenting to the neurology/medicine outpatient of a tertiary care center in the eastern Nepal. The patients already diagnosed by treating physician/neurophysician were selected by convenient sampling method and interviewed using a short questionnaire consisting of open ended, closed ended and mixed type questions from amongst those aged 16 year and older [Table 1]. All the patients had undergone relevant investigations including CT scan head, nerve conduction study and blood and urine investigations as required for establishing the diagnosis prior to inclusion in the study. Patients who refused consent or were unable to answer the questions due to their critical illness status, dementia, severe aphasia or anosognosia were excluded from the study. The demographic data including age, sex, residence, education level and economic status were recorded. The survey questions were asked and elaborated whenever required and recorded by one of the coauthors. The data collected was analyzed using descriptive statistics.
Results
Our study included 49 males and 51 females. Majority of our patients were in the age group 16 to 60 years (87%). Eighty three patients were Hindus and thirteen were Buddhist. The rest followed other religions. Eighty percent of our patients were from Sunsari district of Nepal and 15% were from Morang district. The remainder of the participants belonged to other areas. Our study population included 70 literate patients. Forty patients had studied up to primary level, 22 had studied up to secondary and 18 had studied beyond secondary level. The neurological diagnoses of the patients included migraine (30%), idiopathic and symptomatic epilepsy (28%), neuropathy (15%), central nervous system infections (12%), stroke (11%) and miscellaneous others (4%). The duration of neurological disease was more than 1 year in 52 of the 100 patients with 24 patients of these having had the disease for more than 5 years.
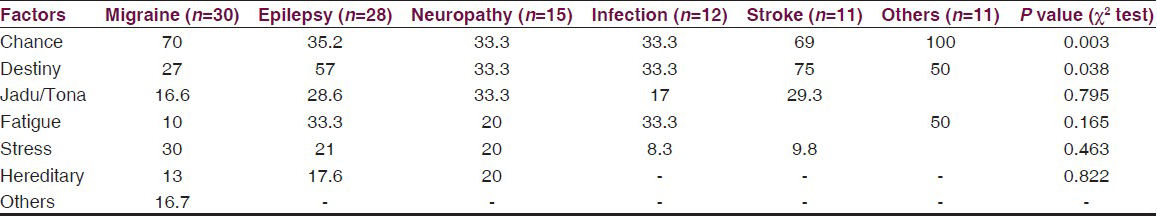
In response to the first open ended question as to what they thought triggered their disease, 51% responded by expressing “No idea” about the triggering factor for their illness. Twenty-nine percent of patients gave non-congruent response and 20% gave medically congruent explanation about the triggering factor. Interestingly, when asked to respond in ‘yes or no,’ the closed ended question regarding psychological factors as likely attributed cause of their illness, only 16% of patients answered affirmatively. Females more often felt that psychological factors triggered their illness. Chance, destiny and ‘jadu-tona’ (witchcraft) topped the list of factors triggering the illness along with stress in daily life in response to the third question [Table 2]. In response to the fourth, mixed type of question regarding approaching traditional faith healer or alternative medicine, 46 percent of patients reported using alternative methods including use of services of Dhami Jhakri (traditional faith healers) even prior to seeking medical advice. Of those who first sought alternative methods, 44 consulted traditional faith healers and one each approached ayurvedic doctor and homeopath. Only 16 of the 44 patients who first sought traditional healer's help were illiterate. Seven of the 44 patients were educated beyond higher secondary. While fifty nine percent of patients expressed strong belief in Dhami Jhakri, the rest 41% did not have any faith in the traditional faith healers. All of them expressed family and relatives’ suggestions as one of the reason for first going to a traditional healer. Interestingly, in response to the fifth question, 16% of patients admitted to planning for trying alternative methods including visit to the traditional faith healer when interviewed. The sixth question elicited history of non-compliance of prescribed medicines in 21% of patients. Eight of the twenty non-compliant patients stopped medicines because of having not been cured by the medicine. Three patients reported adverse drug effects as the reason for stopping the medicine without doctor's advice and the other three thought that they were cured and did not need to continue any medicine. Six patients did not come out with any reason for non-compliance.
Discussion
The beliefs, perceptions, opinions and practices of patients have significant influence on the delivery of timely, consistent and appropriate treatment to patients with neurological diseases. Generally the neurological diseases have been perceived to be incurable, untreatable and often associated with supernatural forces. Developments in the field of neurology over the recent around 3 decades have proved these perceptions wrong. There is greater recognition for exploring the psychosocial, organizational and political factors influencing causation of neurological disorders.[1] We surveyed 100 patients with neurological disorders and found majority of patients having no idea of the factors causing their illness or had medically non-congruent views about the neurological disorders. Croquelois et al. in a similar study interviewed inpatients in neurology department of their university hospital in Switzerland. In their study, 49% of patients interviewed expressed that they had ‘no idea’ about the triggering factor for their illness.[2] This is similar to 51% of our patients expressing ‘no idea’ about the triggering factor for their illness. The medically congruent explanation for their illness was reported by 20% in our study group similar to 16% reported by Croqueloise et al.[3] We asked additional questions to our patients in view of the generally culturally accepted practice of going to Dhami Jhakri (traditional faith healer) in Nepal. We asked about their visits to the faith healer or alternative systems of medicine prior to seeking help from modern medicine system. Interestingly, good number of patients expressed plans to consult faith healer even while on therapy. The practice of seeking traditional healers first in preference to a qualified doctor was observed even among those who had received formal education. Generally, epilepsy is believed to be associated with higher rate of attribution to supernatural forces and faith healing practices among patients. Interestingly, in a study that included faith healing practices among epileptics from northwest India, authors reported that only 7.5% patients of their sample population of 400 idiopathic and symptomatic epileptics approached faith healers.[4] While our sample population included only 28 epileptics, the higher overall faith healing seeking behavior across various neurological disorders including migraine, stroke, neuropathies in our study is likely related to the different prevalent sociocultural mileu of our sample population. Fifty nine percent of our patients expressed strong belief in traditional faith healers. Forty four percent patients of our study group approached traditional faith healers before contacting modern medicine practitioner. In a study from India, Khwaja et al. reported delay in seeking medical help in 33% of epileptic patients due to their religious beliefs and superstitions.[5] Another study conducted among South Asians population of Britain revealed that 54% of epileptics sought traditional healers’ help.[6] Several authors have reported lack of congruency in knowledge and perceptions of patients leading to non-compliance of medicine and medical advice among stroke patients.[78]
It appears that the social and cultural background of patient plays a strong role in type of remedy sought by them. The behavior of seeking traditional faith healing persists despite change in educational and economic status. This could be due to influence of family and relatives. Lack of availability of qualified doctors in immediate near vicinity is also an important issue in Nepal. Traditional healers are there in the community even in remote and not well connected areas.
Our survey confirmed strong beliefs of patients in traditional faith healers across all the neurological diagnoses in our sample population taken from amongst the outpatients of the tertiary care center in eastern Nepal. There is a need to effectively communicate and educate patients. While qualitatively the beliefs of patients may be similar across different political, social, cultural and economic boundaries, the contribution of different beliefs in attitudes and practices of patients appear to differ.
Conclusion
Patients’ beliefs about the factors triggering their neurological disorders often do not conform to medical opinion. Physicians need to consider patients’ beliefs while explaining the disease and treatment so that the patients compliance improves and there is better doctor–patient relationship. Further studies with appropriate sample size addressing the etiological beliefs of patients suffering from individual neurological disorders need to be conducted to explore issues specifically related to the particular neurological condition.
Acknowledgment
We acknowledge the facilitation of conduct of study by Professor Prahlad Karki, Head, Department of Internal Medicine, BPKIHS and Dr. R Laxmi Chauhan, former Assistant Professor (Internal Medicine), BPKIHS, Dharan.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Epidemiology, aetiology and clinical management of epilepsy in Asia: A systematic review. Lancet Neurol. 2007;6:533-43.
- [Google Scholar]
- Diseases of the nervous system: Patients’ aetiological beliefs. J Neurol Neurosurg Psychiatry. 2005;76:582-4.
- [Google Scholar]
- Risk awareness and knowledge of patients with stroke: Results of a questionnaire survey 3 months after stroke. J Neurol Neurosurg Psychiatry. 2006;77:726-8.
- [Google Scholar]
- Psychosocial, demographic and treatment-seeking strategic behavior including faith healing practices, among patients with epilepsy in northwest India. Epilepsy Behav. 2008;13:323-32.
- [Google Scholar]
- Relegious beliefs about causes and treatment of epilepsy. Br J Gen Pract. 2005;55:26-31.
- [Google Scholar]
- Knowledge of stroke risk factors among primary care patients with previous stroke or TIA: A questionnaire study. BMC Fam Pract. 2010;11:47.
- [Google Scholar]
- Satisfaction with information and advice received by stroke patients. Clin Rehabil. 1997;11:68-72.
- [Google Scholar]






