Translate this page into:
A diagnostic and therapeutic challenge involving a case of dysphagia in association with cervical osteophytosis and a dental pain
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Herein, presenting a case of a 42-year-old female with the chief complaint of dysphagia. The problem was assumed to be of dental origin, due to the onset of dental pain followed by dysphagia. A cervical radiograph revealed the presence of osteophytic lipping which proved to be the cause of dysphagia. Confusing and overlapping disease entities showing similar symptoms need thorough investigation. Dysphagia related to cervical spondylosis may have a direct connection with the person's occupation. Dentistry is considered a potentially hazardous occupation with regard to musculoskeletal disorders. However, additional studies are required to understand the occupational hazards faced by dentists.
Keywords
Cervical pain
dentist
dysphagia
toothache
Introduction
While dysphagia is reasonably common, it is a serious problem requiring immediate investigation and management. It is commonly seen in old age as a result of musculoskeletal and degenerative changes. It can also be associated with diseases involving the oropharynx, esophagus, the nervous system, or a combination thereof.
Dysphagia due to musculoskeletal disorders (MSDs) such as osteophytosis is relatively uncommon. Overloading the soft tissues and bone eventually causes osteophytes to form in order to compensate for the greater stresses being imposed on the surrounding bone and soft tissue.[1]
In the present case, osteophytosis may have been caused by a work-related MSD. It has been reported that 30%-50% of workers are exposed to significant physical occupational hazards leading to MSDs.[2] Dentistry is a profession where work load may lead to various MSDs.
Case Report
A 42-year-old female patient was referred to the dental department complaining of difficulty in swallowing. She reported pain with every swallow (odynophagia), causing constant discomfort, but no other obvious symptoms or systemic problems. She had been a practicing dentist for the last 12 years, and reported mild pain on swallowing which had worsened within 2-3 days of onset. She was prescribed medication (azithromycin 500, cephalexin 500, and ibuprofen) for throat infection without any relief. Subsequently, she developed intermittent but acute throbbing pain and tenderness in her maxillary molars on the right side, and was referred to the dental department.
On examination, pain on percussion was evident with regard to teeth #16 and #17. Intraoral radiography showed proximal caries in tooth #17, while tooth #16 had evidently been satisfactorily root canal treated. As the pain was not relieved by medication (cephalexin 500 and serratiopeptidase-diclofenac potassium), endodontic treatment was administered to tooth #17. Four days after the treatment, the patient resumed with persistent dysphagia, without tooth pain. On examination, previously root canal treated tooth #16 was tender, and was therefore considered for re-endodontic treatment. A complaint of severe piercing pain on instrumentation to the mesio-buccal canal of tooth #16 perplexed endodontists, ultimately they decided to go for mesial root resection expecting that it would resolve the problem, but the dysphagia persisted [Figure 1].
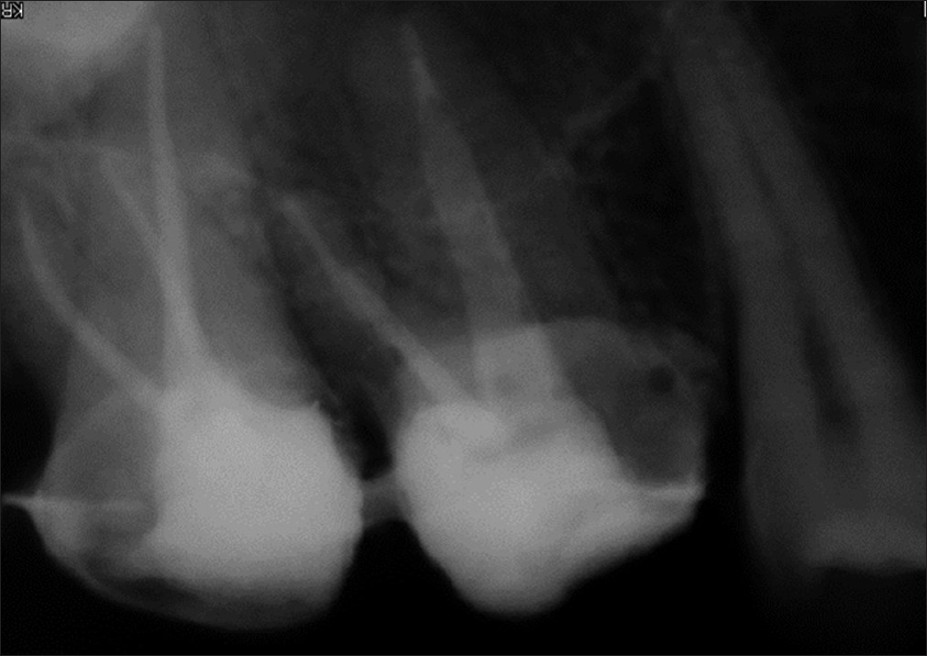
- Endodontic treatment of both molars, completed; tooth #16 shows a resected mesial root and provisional crowns cemented in place
A fortnight later the patient returned with worsened dysphagia without dental pain. At the eye/ear-nose-throat (ENT) department, the otorhinolaryngologist diagnosed the case as tonsillitis, and a week later, as sinusitis. The treatment plan was changed with each different diagnosis, without any relief. The patient was then advised to undergo endoscopy, which ultimately proved to be normal. Ultrasonography (USG) of the neck and thyroid function tests also turned normal.
The patient was referred to the orthopedic department where they revealed a “stiff neck,” which proved to be the main cause of dysphagia. On palpation and pressure at C3 and C4 levels, the patient experienced pain with restricted spinal movements. Cervical radiographs revealed osteophytic projections impinging upon the posterior pharyngeal wall at the levels of C3, C4, and C5, and cervical hypolordosis [Figure 2]. The osteophyte at the pharyngo-esophageal junction was positioned in such a way that it interfered with the swallowing movement. The patient was ultimately diagnosed with osteophytosis involving C3, C4, and C5.

- Lateral cervical spine radiograph showing osteophytes at C3, C4, and C5
The initial treatment planned was nonsurgical. The patient was referred to the chiropractor/physiotherapist for management of stiff neck. In conjunction with nonsteroidal anti-inflammatory drugs, the nutritional supplements were prescribed for a month.
The treatment also included muscle relaxant massages, spinal adjustment with neck exercise, and traction sessions.
Discussion
Dysphagia is known to be caused either due to extrinsic compression of esophageal lumen or some intrinsic pathologies of esophageal wall.[3] In most cases, the osteophytes remain asymptomatic while in a few, it has been documented with severe dysphagia. Osteophytic compression can occur at any level of the vertebral column, but more commonly at the C5-6 level. Therefore, cervical osteophytes should be suspected as a cause of swallowing difficulties when other explainable causes are absent. Although rarely encountered, these osteophytes are most commonly found between C3 and C6.[4] Similarly, in the present case, the patient depicted a severe form of dysphagia due to the formation of osteophytes at C3, C4, and C5 levels. The diagnosis was delayed due to the lack of association of significant conditions where the dysphagia is more commonly seen.
Three different theories have been postulated for occurrence of dysphagia. Mechanical distortion of the esophagus may occur due to the mass effect of a large anterior osteophytes; osteophytes may also cause dysphagia if they are located opposite a fixed point of the esophagus such as the cricoid cartilage (C 6 level).[5] Besides, osteophytes may cause an inflammatory reaction around the esophagus resulting in edema and cricopharyngeal spasm.[6] We consider the last theory as a credible cause of dysphagia in the present case.
Though the dysphagia is expected to be chronic in anterior osteophytosis, in the present case it was acute and relatively more troublesome due to the triggering dental pain. Dysphagia and odynophagia, however, are common symptoms in oral medicine as well, which can appear following oropharyngeal infections, dental surgeries, or even after procedures as simple as dental extractions.[7] Since there is hardly any relevant documentation which could associate the osteophytosis with dental pain and dysphagia, in the present case, the occurrence of unbearable dental pain in conjunction with dysphagia may have been merely coincidental.
Various causes of dysphagia have been documented in the literature. Dysphagia due to osteophytes has been reported by a few in the past, but more recently Kapetanakis et al.,[8] documented a case of giant osteophytes in an 81-year-old patient, causing dysphagia; while Khan et al.[9] have reported a case in which dysphagia developed because of anterior cervical osteophytes in the setting of osteoarthritis. Yet another case of anterior cervical osteophytes with multilevel disc prolapse causing dysphagia was detected by Mishra et al.[10]
In the present case, it was more confusing to assess the cause of dysphagia as the patient was relatively young without any systemic diseases, which brought us to the conclusion that the osteophytosis may have some relation to the MSD acquired as a professional hazard, which can be a matter of concern for the dental professionals.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Degenerative and inflammatory diseases of the spine. In: Benzel EC, ed. Biomechanics of Spine Stabilization. Rolling Meadows. IL: pAmerican Association of Neurological Surgeons Publications; 2001.
- [Google Scholar]
- Dysphagia associated with cervical spine disorders: Pathollogic relationship.? J Spinal Disord. 1988;1:312-6.
- [Google Scholar]
- Dysphagia Caused by Multilevel Cervical Osteophytes. Am J Phys Med Rehabil. 2008;87:607.
- [Google Scholar]
- Hypertrophic cervical osteophytes causing dysphagia: A review. J Neurosurg. 1980;53:338-44.
- [Google Scholar]
- Evaluation and correction of dysphagia-producing cervical osteophytosis. Laryngoscope. 1974;84:2045-50.
- [Google Scholar]
- Aphonia and dysphagia following dental extraction. Report of a case. Dent Pract Dent Rec. 1966;16:205.
- [Google Scholar]
- Can a giant cervical osteophyte cause dysphagia and airway obstruction. A case report? Wien Klin Wochenschr. 2011;123:291-3.
- [Google Scholar]
- Anterior cervical osteophytes with multilevel disc prolapse causing progressive dysphagia and quadriparesis. Neurol India. 2012;60:366-7.
- [Google Scholar]






