Translate this page into:
Uncontrolled seizures resulting from cerebral venous sinus thrombosis complicating neurobrucellosis
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cerebral venous sinus thrombosis is a rare form of stroke caused by thrombosis in venous sinuses of the brain. In this study, we reported on a patient with venous sinus thrombosis and brucellosis who presented with uncontrolled seizure despite being treated with anti-epileptic drugs at high doses. The case was a 33-year-old woman with a history of controlled complex partial seizure who presented with headache, asthenia, and uncontrolled seizure for one month. She was febrile and a brain CT scan indicated hemorrhagic focus in the left posterior parietal and the temporal lobe. Magnetic resonance imaging and magnetic resonance venography also proved venous sinus thrombosis in the left transverse sinus. Besides [In addition], a laboratory assessment confirmed brucellosis. Following the treatment with anti-coagulant, anti-brucellosis, and anti-epileptic agents, the patient was discharged in good condition with medical orders. Clinical suspicion and accurate evaluation of a patient's history is the most important clue in diagnosis and treatment of brucellosis and cerebral venous sinus thrombosis, especially in uncontrolled seizure in patients who had previously been under control.
Keywords
Brucellosis
cerebral venous sinus thrombosis
neurobrucellosis
seizure
Introduction
Cerebral venous sinus thrombosis (CVST) is a rare disorder which is potentially followed by serious consequences and high mortality,[12] forming less than 1% of all the strokes.[3] It is an uncommon condition and its clinical presentation and prognosis varies from complete recovery to death.[1] Although CVST affects young-to-middle-aged patients with the mean age of 37-38 years old,[4] based on relevant reports, it is more prevalent among women.[24] It presents such symptoms as progressive headache, vision disorders, papilledema, seizure, decreased awareness, and signs similar to those in subarachnoid hemorrhage.[5]
The risk factors include increased inherited and acquired coagulation, infections, dehydration, ketoacidosis, polycythemia, hyperviscosity, pregnancy, consumption of oral contraceptive pills, alternative hormone therapy, malignancies, and the like.[6] CVST is more frequent among young women in the puerperium compared to those in pregnancy, as it is reported that oral contraceptive pills increase the risk of the condition by 13 times.[47] Other studies have shown otitis, mastoiditis, sinusitis, meningitis, and systemic infectious diseases may also cause CVST.[58] Nonetheless, to the best of the researcher's knowledge, no evidence of brucellosis as a correlated factor of CVST has been found to date.
Seizure is a symptom of CVST, the incidence of which varies from 7% to 15% during the presentation and can rise up to 40% during the course of the illness. Of course, it is not common during the acute phase of arterial thrombosis.[1] However, due to the significance of prognosis and variation in the presentation of CVST, in the current study, we reported a patient with CVST complicating brucellosis who suffered from uncontrolled seizures.
Case Report
The case was a 33-year-old woman who was referred to the Neurology Clinic of Vali-e-Asr Hospital, Arak, Iran, with headache, asthenia, decreased appetite, fever, sweating, and increased number of seizures up to 3-4 times a day. Night sweats and fever; suspicious myalgia description, and residence in rural area and being in contact with farm animals; counseling for infectious diseases; and medical assessments for brucellosis and hepatitis C and B were in the patient's history. The patient's history indicated that she was diagnosed with a complex partial seizure persisting for 10 years. A month before referral to the hospital, her seizure had gone out of control and, despite the patient's frequent visits and increased drug dose, the treatment had not been successful. Prior to admission, the patient was prescribed 50 mg lamotrigine and 400 mg carbamazepine three times a day and 1 mg folic acid once a day.
Physical examination
The patient's body temperature was 37.8 °C, which did not pose any significant problems. A nervous system examination also indicated that the patient was in a complete state of awareness and did not demonstrate neck stiffness.
Laboratory tests
Routine lab tests reported increased liver enzymes and normal CBC. The results of Wright's agglutination test (1/640), Coombs-Wright test (1/640), and 2ME (1/320) were positive and confirmed brucellosis, while hepatitis C and B were not verified. Concurrently, an evaluation was carried out to discover the cause of abrupt increase in the frequency of seizures in spite of treatment with antiepileptic drugs. A brain CT scan revealed hyper-dense areas in the left posterior parietal and temporal lobe together with peripheral hypo-density, hemorrhagic focus, and edema around it [Figure 1]. An MRI indicated a suspicious lesion similar to those in hemorrhagic infarction or hematoma in the left temporal lobe and an abnormal signal in the left transverse sinus [Figure 2]. Hence, on suspicion of venous sinus thrombosis, an MRV was prescribed for the patient [Figure 3].
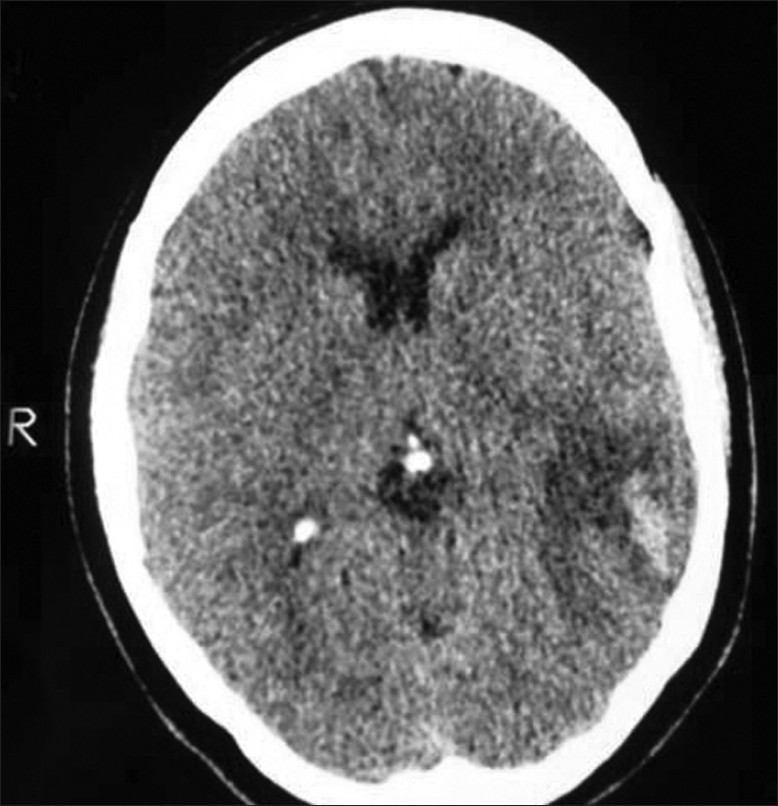
- CT scan of the brain; hemorrhagic infarction and peripheral edema in the left posterior parietal and the temporal lobes
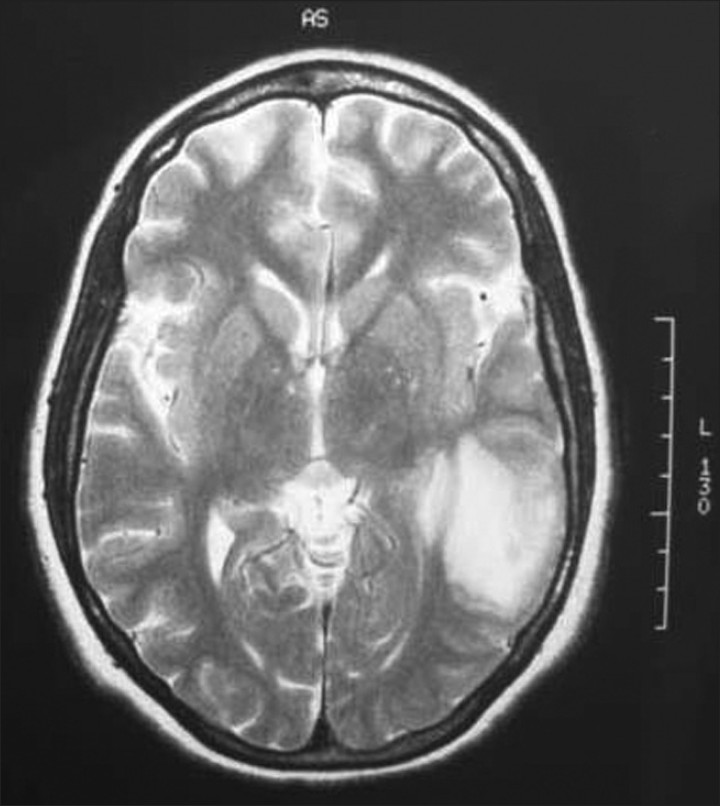
- MRI of the brain; hemorrhagic infarction of the left temporal lobe
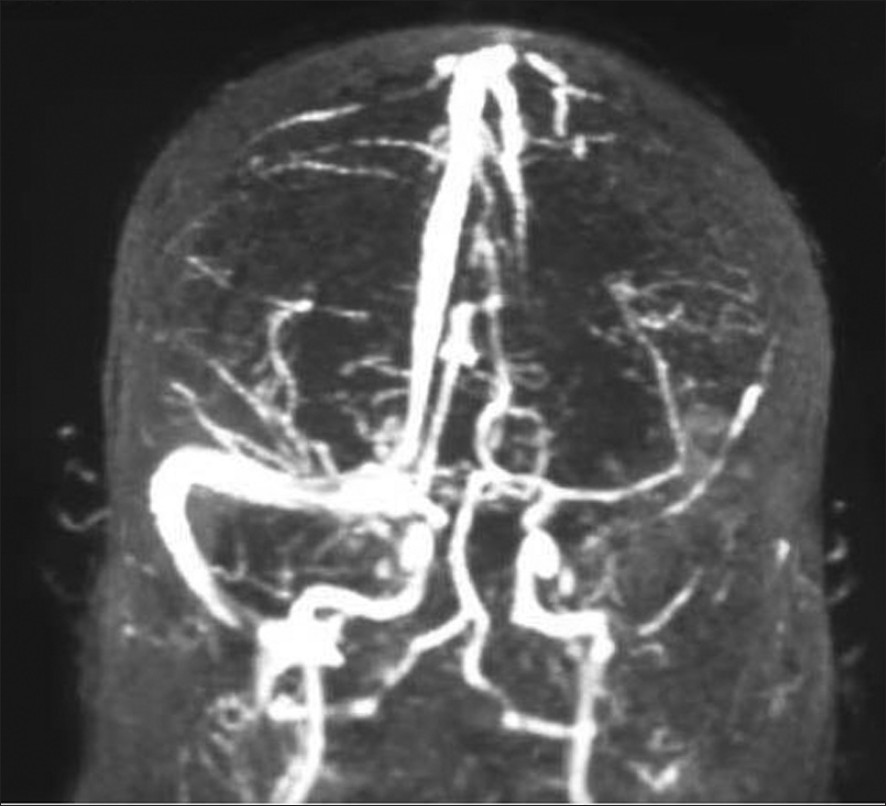
- MRV of the brain; the left transverse sinus thrombosis
Treatment and follow-up
With the verification of brucellosis, treatment was performed by administration of Rifampin (600 mg/d), Doxycycline (100 mg two times a day), and Streptomycin 1 g/day. Streptomycin was stopped after 10 days while Rifampin and Doxycycline continued for eight weeks. In addition, Warfarin and Heparin were administered, eventually leading to the control of seizures. Three days after admission and the initiation of treating brucellosis and CVST, seizure was finally under control and the fever and other symptoms disappeared. Therefore, the patient was discharged with anti-brucellosis drugs Carbamazepine 200 mg three times per day, and Warfarin, in good general health conditions without fever and signs of infection.
In the third month after treatment, Wright's agglutination and 2ME tests showed 1/40 and 1/20 respectively. These values of Wright's agglutination and 2ME tests are negative in Iran based on guidelines for tuberculosis control program. The prescribed Warfarin continued for one year and during the first year an MRI and MRV showed a decline in venous sinus thrombosis symptoms and brain bleeding.
Discussion
Noticing a wide range of clinical symptoms, the diagnosis of brucellosis and venous sinus thrombosis was difficult. Accordingly, the patient's history and clinical suspicion must be considered with meticulousness. With regard to the case under study, the co-occurrence of CVST and brucellosis increased the likelihood of recurrence of seizures. However, CVST is one of the manifestation of neurobrucellosis.[9] Moreover, the increased dosage of Carbamazepine before admission might have been the reason of uncontrolled seizures.[10]
Uncontrollable seizure was the most important clinical feature of the patient. This symptom might have occurred as a result of administration of high dose of epileptic drugs [-especially Carbamazepine-] or due to the occurrence of brucellosis as a febrile infectious disease and CVST accompanied by hemorrhagic focus and peripheral edema.[910] Also, the increased level of liver enzymes in the patient could be due to a high dose of drugs (drug-induced hepatitis or anticonvulsants) or the involvement of liver by brucellosis.
Owing to the presence of hemorrhagic lesion, cerebrospinal fluid sampling was not conducted. As a result, we could not prove the occurrence of neurobrucellosis. Nevertheless, in solely one case study, venous sinus thrombosis was referred to as a manifestation of the occurrence of brucellosis. No other supporting studies were found.[11]
Different studies have indicated the necessity and importance of clinical suspicion of brucellosis in spite of the negative results of the serologic tests for the disease in different neurologic manifestations,[1213] which indicates a wide range of clinical manifestations and a high rate of mortality and morbidity of the disease.[9]
Tuberculosis is an endemic disease in Iran[14] and neurotuberculosis happens in many forms. The disease presentation is similar to neurobrucellosis. Therefore, careful evaluation for neurobrucellosis and brucellosis is essential in a patient suspected of any of these probable diagnoses, especially if the empirical therapy fails.[15] Furthermore, as brucellosis rarely entangles the nervous system, appropriate serological and microbiological tests are helpful for differential diagnosis from chronic infections, especially tuberculosis.[16] In addition, brucellosis and particularly neurobrucellosis should be addressed in the differential diagnosis of CVST.[9]
Prognosis of venous sinus thrombosis depends on different factors. De Bruijn studied 59 patients with this disease and showed that cerebral hemorrhages, papilledema, CNS disturbance, coma, age above 33, and involvement of straight sinus were accompanied by poor prognosis, while an increase of intra-cerebral pressure and the appearance of delta signs in the CT scan were accompanied by good prognosis. In fact, cerebral hemorrhage increases the poor prognosis of CVST by ten times.[1]
Conclusion
Overall, co-morbidities of CVST with other infectious or non-infectious diseases may affect the prognosis of the disease. Also, a clinical suspicion and accurate evaluation of the patient's history are the most important clues in the diagnosis and treatment of uncontrolled seizure. As for the patient in this research, CVST and brucellosis treatment controlled the seizure. Thus, it is advisable to take account of the factors that might have provoked seizure so as to provide the patient with effective care and management as promptly as possible.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients. J Neurol Neurosurg Psychiatry. 2001;70:105-8.
- [Google Scholar]
- EFNS guideline on the treatment of cerebral venous and sinus thrombosis. Eur J Neurol. 2006;13:553-9.
- [Google Scholar]
- Venous disease: Cortical veins and sinuses stroke pathophysiology, diagnosis and management. Stroke. 2005;53:731-43.
- [Google Scholar]
- Cerebral venous sinus thrombosis in Saudi Arabia. Neurosciences (Riyadh). 2011;16:329-34.
- [Google Scholar]
- Cerebral venous thrombosis: A new manifestation of neurobrucellosis. Clin Infect Dis. 1999;28:399-400.
- [Google Scholar]
- Carbamazepine overdose: A prospective study of serum levels and toxicity. J Toxicol Clin Toxicol. 1990;28:445-58.
- [Google Scholar]
- Neurobrucellosis with transient ischemic attack, vasculopathic changes, intracerebral granulomas and basal ganglia infarction: A case report. J Med Case Rep. 2010;4:340.
- [Google Scholar]
- Cerebral venous thrombosis: A new manifestation of neurobrucellosis. Clin Infect Dis. 1999;28:399-400.
- [Google Scholar]
- Epidemiology of tuberculosis in the Southeastern Iran. Eur J Epidemiol. 2005;20:879-83.
- [Google Scholar]
- Neurobrucellosis with transient ischemic attack, vasculopathic changes, intracerebral granulomas and basal ganglia infarction: A case report. J Med Case Rep. 2010;4:340.
- [Google Scholar]
- Brucella meningoencephalitis with hydrocephalus masquerading as tuberculosis. Asian Pac J Trop Med. 2010;3:835-7.
- [Google Scholar]






