Translate this page into:
Neurocysticercosis presenting as Millard Gubler syndrome
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neurocysticercosis is a common childhood neurological illness in India. A variety of presentations have been reported in the literature, including weber syndrome. Neurocysticercosis, manifesting as Millard Gubler syndrome, have not been reported in literature. Therefore, we report a child presented to us with Millard Gubler syndrome due to pontomedullary neurocysticercosis and was treated successfully.
Keywords
Cranial nerve palsy
Millard Gubler syndrome
neurocysticercosis
Introduction
Neurocysticercosis is the most common parasitic infection of central nervous system and result from infection with the intermediate stage of Taenia solium. In India, cysticercosis is highly prevalent and CNS involvement is seen in 60%–90% of infested patient.[1] Cerebrum and cerebellum are common sites but may involve brainstem, basal ganglion, thalamus, and lateral sinus. Seizures are the commonest presenting feature in majority but can present with headache, focal deficits, hydrocephalus, and raised intracranial pressure.[2] Cysticercal granuloma as cause of Weber's syndrome and ptosis[3] has also been reported. We report a case of pontomedullary neurocysticercosis presenting with left VI and VIIth cranial nerve palsy of lower motor neuron type and contralateral hemiplegia, i.e., Millard Gubler syndrome, which is not reported till date.
Case Report
A 7 year girl presented in outpatient department with history of vomiting and deviation of angle of mouth to right side for 3 days. There was no history of fever, headache, seizures, altered sensorium, diplopia, nasal regurgitation of feeds, trauma, ear discharge, rash, recent vaccination, and history of contact with an open or treated case of tuberculosis. There was no known significant past medical history.
Examination of patient revealed palsy of VIth and VIIth cranial nerve of left side with right-sided grade III/V Weakness, upper motor neuron type, of upper and lower limbs. Her right-sided babiniski's sign was positive with exaggerated deep tendon reflexes on same side. There was no sensory loss. Pupils were normal in size and reacting normally to light. On fundus examination, there was no retinal cyst and evidence of papilloedema. She was oriented and hemodynamically stable. Rest of the systemic examination was unremarkable.
On investigation, his complete blood count CBC , X-ray chest, blood glucose, electrolytes, liver and renal function tests were normal. Mantoux test was negative at 72 h. Cerebrospinal fluid study showed cells 8/mm3 protein; 48 mg/dl, and glucose was 68 mg/dl. Cysticercal IgG and IgM antibody were strongly positive in CSF by ELISA. Contrast-enhanced computed tomograph (CECT) of cranium revealed single-ring enhancing lesion, with eccentric dot and perilesional edema at pontomedullary area of brain stem suggestive of inflammatory granuloma with possibility of neurocysticercosis [Figure 1]. Magnetic resonance imaging (MRI) of brain showed a well-defined ring enhancing lesion with thick rim noted in pontomedullary area of brain stem [Figure 2], which appeared hypointense on T1-weighted and hyperintense on T2-weighted images. FLAIR images showed suppression of internal signal with mild perilesional edema; further suggestive of neurocysticercosis in its colloidal-vesicular stage. Ultrasonography of orbit (B-scan) was unremarkable.
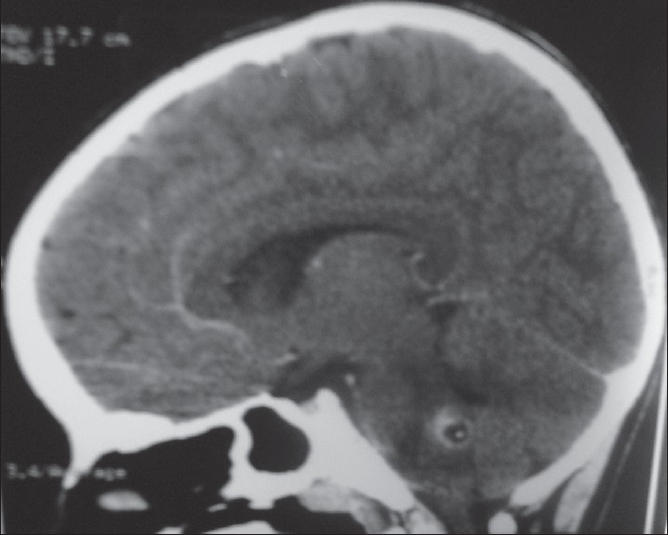
- Coronal CECT image showing solitary ring enhancing lesion, with eccentric scolex, in pontomedullary area
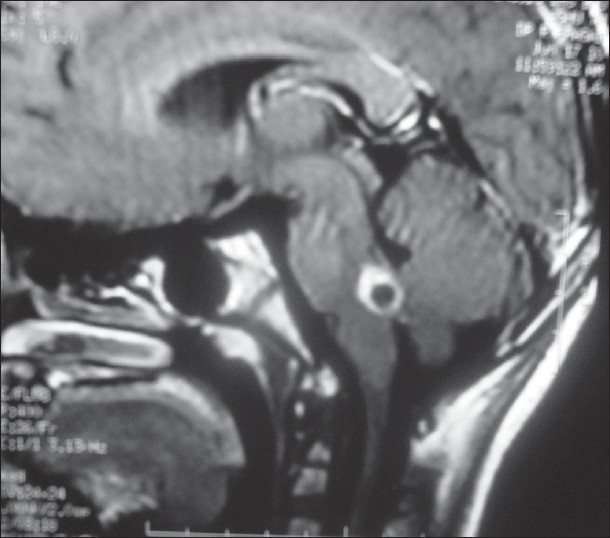
- MRI of cranium showing thick cyst wall enhancement with mild perilesional edema, depicting colloidal–vesicular stage of cysticercosis in pontomedullary area
Patient was administered 20% mannitol (1 gm/kg/dose i.v. 8 hourly for 48 h), dexamethasone (0.5 mg/kg/day for 2 days), and then prednisolone 2 mg/kg/day along with acetazolamide at 75 mg/kg/day. On 3rd day of steroid, oral albendazole at 15 mg/kg/day was started. Steroid was stopped after 7 days and patient was discharged on oral albendazole which was to continue for 28 days and advice of physiotherapy. At discharge, there was no vomiting but deviation of angle of mouth and right-sided weakness persisted. She was called for follow-up after 15 days and found to have no deviation of angle of mouth and weakness. Patient is doing well at 1 and 3 months of follow-up with no clinical evidence of cranial nerve palsy and hemiparesis. Repeat MRI of brain at 3 month was normal.
Discussion
Neurocysticercosis is a life-threatening illness. It has pleomorphic manifestations and includes seizures, headache, and focal neurological deficits. Unusual manifestations are stroke, visual loss, ataxia, dystonia, dementia, and hydrocephalus.[24] Cysticercal granuloma as cause of Weber's syndrome and ptosis[5] have also been reported. Cerebral infarction may result from obstruction of small terminal arteries or vasculitis. Intraventricular (5%–10%) and meningeal cysticerosis are associated with hydrocephalus, signs of meningeal irritation, and raised intracranial pressure. Neuroretinitis and occipital lobe syndrome have been reported in four patients of neurocysticercosis.[6] We here report a case of neurocysticercosis presenting as left VI and VIIth cranial nerve palsy of lower motor neuron type and contralateral hemiplegia, i.e., Millard Gubler syndrome, which is unreported in literature.
CT scan and MRI are useful in anatomical localization of cysts, but MRI cranium is more sensitive in picking up active lesions. Our case fulfilled the imaging absolute diagnostic criteria (histologic demonstration of the parasite from biopsy of a brain or spinal cord lesion, cystic lesions showing the scolex on CT or MRI, and direct visualization of subretinal parasites by funduscopic examination).[7] Patients with active cysts remain at risk of serious complication. Therefore, all patients with multiple cysts should receive treatment with steroid to reduce intracranial pressure and edema; thereafter cysticidal drug, i.e., albendazole. Efficacy of treatment should be monitored by repeat CT/MRI after 3 months.[7]
Our patient improved and became asymptomatic with steroid treatment and albendazole. Recognizing this clinical entity would avoid unnecessary antituberculous treatment and surgical intervention. Cysticercosis is common in tropical countries including India but neurocysticercosis of brain stem is rare. Millard Gubler syndrome as presentation of neurocysticercosis is unreported.
Source of Support: Nil
Conflict of Interest: None declared
References
- Clinical spectrum of 500 children with neurocysticercosis and response to albendazole. J Child Neurol. 2000;15:207-13.
- [Google Scholar]
- Sudden onset ptosis caused by midbrain neurocysticercosis in 2 children. J Child Neurol. 2008;23:334-7.
- [Google Scholar]
- Clinical pleomorphism of neurocysticercosis in children: Some unusal manifestations. J Pediatr Neurol. 2006;4:103-9.
- [Google Scholar]
- Optic nerve cysticercosis: Case report and review of current management. Orbit. 2005;24:159-62.
- [Google Scholar]






